Diagnosis and treatment of early stage Parkinson's disease
O.S. Levin1,2, A.V. Rosinskaya3
1Russian Medical Academy of Postgraduate Education; 2Center for Extrapyramidal Diseases (Moscow); 3Room of extrapyramidal disorders of Primorsky Regional Clinical Hospital No. 1 (Vladivostok)
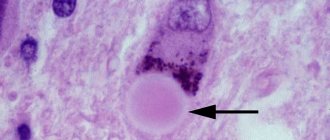
Parkinson's disease (PD) is a progressive neurodegenerative disease characterized by the combination of hypokinesia with muscle rigidity and/or resting tremor, as well as later developing postural instability and a wide range of non-motor disorders, including autonomic, mental, dyssomnic and sensory symptoms. The formation of neurotoxic aggregates of the small presynaptic protein alpha-synuclein (the main component of Lewy bodies), accompanied by the death of pigmented neurons in the ventrolateral parts of the substantia nigra pars compacta, is considered to be the main link in the pathogenesis of PD. However, in recent years it has been established that only the main motor symptoms of parkinsonism correlate with damage to the substantia nigra; at the same time, the degenerative process in PD also involves other groups of neurons in various areas of the brain, as well as in the peripheral nervous system, which underlies numerous non-motor manifestations of the disease [1, 3].
Mechanisms of PD development
This is a synucleinopathy. When neurodegenerative processes occur, alpha-synuclein protein gradually accumulates inside cells. It is called Lewy body. At the onset of the disease, Lewy bodies can be found only in parts of the peripheral nervous system. They are localized in the plexuses of Meissner and Auerbach, located in the gastrointestinal tract. With further progression of the pathology, Lewy bodies “capture” the nuclei of the brain stem and the substantia nigra of the medulla oblongata.
Severe forms of Parkinson's disease are characterized by the fact that Lewy bodies disrupt the normal functions of the cerebral cortex. In this case, one can judge the topical distribution of neurodegenerative changes: while the substantia nigra is not affected, the clinical picture will be dominated by non-motor symptoms. As the pathology spreads, nigral neurons begin to die, which is accompanied by the appearance of motor symptoms.
Epidemiology
According to a continuous population study, the prevalence of PD in Russia is 139 cases per 100,000 population, the incidence of PD is 16 cases per 100,000 population per year. With increasing age, the risk of PD increases, and the detection rate of PD among people over 65 years of age is already about 1%. Most cases of the disease occur between the ages of 60 and 70 years. However, in 15% of cases, PD debuts before the age of 45 years.
Based on the available data and the age-sex structure of the Russian population, we can roughly estimate the total number of patients with PD in our country at 210 thousand, with the disease occurring in approximately 20 thousand patients each year. Approximate calculations show that at least a quarter of patients (that is, more than 50 thousand) end up outside the scope of medical care, and most of these are patients with an early stage of the disease [3].
Diagnostics
The diagnosis of PD is carried out in 2 stages. At the first (syndromic) stage, parkinsonism syndrome must be distinguished from other conditions that mimic it (Table 1).
Table 1. Conditions requiring differential diagnosis with parkinsonism.
| If there is tremor | In the absence of tremor |
| Increased physiological tremor Essential tremor Dystonic tremor Hepatolenticular degeneration | Apathetic-abulic syndrome Depression Frontal dysbasia Humeral periarthropathy Hypothyroidism Cervical osteochondrosis Dementia with the phenomenon of paratonia (continuity) Catatonia |
Identifying signs of hypokinesia is key in differential diagnosis. Initial symptoms of hypokinesia may be characterized by difficulty writing, pressing buttons on a remote control, brushing teeth, typing on a keyboard, removing small objects such as coins from a bag or pocket, putting on slippers, etc. Sometimes, already at an early stage, weakness and lag of one of the legs when walking appears with a change in the usual gait pattern. Characterized by a weakening of friendly arm movements when walking (acheirokinesis), impaired recharging of the watch (“Rolex symptom”). A weakened voice, slowness, weakening of intonation, or unclear speech may be noticed (especially when pronouncing morphologically complex words quickly). When examined to identify hypokinesia, the patient is asked to perform certain movements for about 20 seconds at the fastest pace and with maximum amplitude. In this case, the doctor should pay attention to the slow initiation of movement, asymmetry of movements, but most importantly - to a special form of exhaustion of movements (decrement), which, as they are repeated, become increasingly slower, decrease in amplitude, and require more and more effort from the patient. The phenomenon of exhaustion can be detected in all movements assessed, but is sometimes noted only in one of the tests. It should be borne in mind that the slowness and awkwardness of movements characteristic of patients with parkinsonism at an early stage can be confused with manifestations of pyramidal and cerebellar insufficiency, as well as severe depression, however, these conditions are not characterized by a decrement of movements as they are repeated. It should be borne in mind that hypokinesia can be difficult to detect against the background of severe tremor in a limb, however, even in this case it is important not to miss a diagnostically significant phenomenon: with parkinsonism, after performing a test for hypokinesia, the patient often holds his hand in a fixed, tense position and is not able to quickly relax.
Muscle rigidity is manifested by stable (as opposed to spasticity) resistance to passive movements in the wrist, elbow, shoulder, knee joints, as well as in the neck, and subjectively by stiffness and unpleasant painful sensations in the limbs. In some patients, when checking their tone, the “gear wheel” phenomenon is revealed. Rigidity should be distinguished from the phenomenon of resistance (gegenhalten), characteristic of patients with dementia and damage to the frontal lobes. Counter-containment changes rapidly depending on the direction and speed of passive movement.
Slow (3–4 Hz) resting tremor in one arm or leg is one of the common initial manifestations of parkinsonism. The presence of a classic resting tremor of the “rolling pills” or “counting coins” type is most characteristic of PD. To identify latent tremor, the patient is asked to make movements with the other hand, walk around, and perform a distraction task (for example, subtracting from 100 by 7). To identify tremors in the leg, you need to examine the patient in a sitting or lying position. However, in the absence of hypokinesia, rest tremor does not allow diagnosing either parkinsonism or PD. It should be taken into account that, on the one hand, essential and dystonic tremor can be observed at rest, on the other hand, postural and kinetic tremor is often observed in PD.
The initial manifestation of PD, especially in young people, may be foot dystonia, which appears or worsens when walking, and much less often - dystonia of other localization.
Early non-motor disorders. Starting from the earliest (prodromal) stage of the disease, the patient may be bothered by emotional depression, increased irritability, fatigue or a feeling of constant fatigue, as well as autonomic disorders such as sweating disorders (“defective thermostat”), for example, profuse sweating in cold weather, and also a tendency to constipation, frequent and/or imperative urination, increased drooling at night (the “wet pillow” symptom), erectile dysfunction. Hypoosmia often occurs already in the premotor stage of PD, but rarely attracts the attention of the patient himself, and a formalized study is necessary to identify it (using special techniques, for example, the University of Pennsylvania Olfactory Test - UPSIT). Identifying signs of rapid eye movement sleep behavior disorder syndrome (anxious dreams, vocalizations, sleep-talking, movements reflecting the content of dreams), which may precede other manifestations of the disease for many years, may be of important diagnostic importance. These non-motor manifestations may improve the accuracy of diagnosis based on early motor symptoms of the disease.
The debut manifestations of PD are also chronic pain syndromes, most often in the back and scapulohumeral region, associated with increased muscle tone, limited mobility and postural disorders.
Already at an early stage, signs of mild cognitive impairment may be detected, in particular instability of attention and slowness of thinking, difficulty finding words (the “tip of the tongue” phenomenon).
"Red flags". The second stage - the stage of nosological diagnosis - comes down to the differential diagnosis of PD with other nosological forms of parkinsonism. It requires a clinical assessment of the history and neurological examination findings. It is important to clarify the drug history. Drugs such as metoclopramide, sodium valproate, cinnarizine, amiodarone can cause drug-induced parkinsonism. Discontinuation of the drug that triggered the development of parkinsonism may not lead to immediate regression of symptoms. Sometimes, after taking the drug and a short-term improvement, the condition worsens again, which indicates a latently developing degenerative process that was “unmasked” by the side effects of the drugs.
A neurological examination may reveal symptoms that are atypical for PD, requiring the exclusion of other diseases that cause parkinsonism. Among them are: symmetry, rapid progression of symptoms with early loss of the ability to move within 5 years, early development of postural instability with falls, lack of a persistent positive effect of adequate doses of levodopa, early development of autonomic failure, rapid onset of dementia (within 1- year), limited mobility of the eyeballs (especially paresis of downward gaze), early development of severe pseudobulbar syndromes, axial dystonia, pyramidal and cerebellar signs, the presence of focal disorders of cortical functions.
Chapter 13. Antiparkinsonian drugs (R.N. Alyautdin)
Pharmacology. Textbook - ed. Alyautdina R.N.
Antiparkinsonian drugs are drugs used to treat Parkinson's disease, parkinsonism syndrome, including drug-induced parkinsonism.
Parkinson's disease (shaking palsy) is a chronic neurodegenerative disease, the basis of which is damage to the pigment-containing dopaminergic neurons of the dense part of the substantia nigra of the brain. The main clinical manifestations of the disease: bradykinesia (stiffness of movements), rigidity (increased skeletal muscle tone) and tremor (shaking) of the hands and head. Clinical manifestations of the disease occur when 70-80% of dopaminergic neurons in the brain die. Parkinson's disease (first described by the English physician James Parkinson in 1817) occurs in 1% of the population under the age of 60 years and in 5% over 60 years of age. A possible cause of the disease is the formation of free oxygen radicals during the oxidative metabolism of dopamine in the substantia nigra of the brain, which can cause the destruction of dopaminergic neurons. There is evidence that there is a genetic predisposition to Parkinson's disease.
The cause of parkinsonism syndrome, also manifested by shaking paralysis, can be infectious diseases of the nervous system (viral encephalitis), vascular diseases of the brain, skull injuries, intoxication (carbon monoxide, manganese, ethanol), syphilitic brain lesions.
Drug-induced parkinsonism is a form of parkinsonism syndrome that develops with long-term use of certain medications, for example, typical antipsychotics (phenothiazines, butyrophenones).
Parkinsonism is classified as an extrapyramidal disorder. The extrapyramidal system, in particular the caudate nucleus and putamen, united in the so-called neostriatum, corrects and refines movements. This is achieved by influencing the motor areas of the cerebral cortex through the thalamus. The activity of cholinergic neurons of the neostriatum, which control the functions of the thalamus, is inhibited by dopaminergic neurons located in the substantia nigra: the axons of dopaminergic neurons of the substantia nigra terminate in the neostriatum and release dopamine, which, by stimulating D2 receptors located on cholinergic neurons, has an inhibitory effect on these neurons (Fig. 13.1). In Parkinson's disease, the number of dopaminergic neurons decreases, which leads to increased cholinergic influences in the neostriatum and the appearance of characteristic motor disorders.
In addition, according to some data, the activity of cholinergic neurons is controlled by glutamatergic neurons. The axons of these neurons terminate in the neostriatum and release glutamate, which stimulates NMDA receptors located on cholinergic neurons and thus increases their activity, resulting in an increase in the release of acetylcholine in the neostriatum.
In Parkinson's disease, due to a decrease in inhibitory dopaminergic influences in the neostriatum, stimulating glutamatergic influences begin to prevail and this leads to a greater increase in the activity of cholinergic neurons of the neostriatum and to the development of characteristic symptoms of the disease. To relieve these symptoms, it is necessary to restore the disturbed balance between these systems in the neostriatum, which can be achieved by increasing dopaminergic influences, decreasing the influence of glutamatergic neurons, and decreasing the influence of cholinergic neurons.
Rice. 13.1. Localization of action of antiparkinsonian drugs. MAO-B – monoamine oxidase B; D,-P – dopamine receptors .
D2– Postsynaptic dopamine receptors
Currently, the following antiparkinsonian drugs are mainly used in the treatment of Parkinson's disease: Drugs that stimulate dopaminergic transmission Dopamine precursor
Levodopa Monoamine oxidase B inhibitors
Selegiline (Deprenil, Eldepril, Yumex) Drugs that increase dopamine release
Amantadine (Midantan) Drugs that stimulate dopamine receptors (dopamine receptor agonists)
Bromocriptine (Parlodel), pergolide (Permax), pramipexole
(Mirapex), ropinirole (Requip) Drugs that inhibit cholinergic transmission
Central anticholinergics: Trihexyphenidyl (Cyclodol), biperiden (Akineton).
Drugs that stimulate dopaminergic transmission
Levodopa is a levorotatory isomer of dioxyphenylalanine (L-DOPA), the immediate precursor of dopamine. Dopamine does not cross the blood-brain barrier. Levodopa crosses the blood-brain barrier by active transport (using a transport system that transports aromatic amino acids across membranes). In intact dopaminergic neurons, levodopa, under the influence of DOPA decarboxylase, is converted into dopamine, which is released from the endings of dopaminergic fibers and stimulates D2 receptors on cholinergic neurons of the neostriatum (see Fig. 13.1). As a result, the activity of these neurons decreases, which leads to the elimination of parkinsonism symptoms. Levodopa is one of the most effective antiparkinsonian drugs: it reduces bradykinesia, muscle rigidity and, to a lesser extent, tremor.
Levodopa is absorbed from the intestine by active transport using the transmembrane transport system for aromatic amino acids. As a result, foods rich in protein can reduce the absorption of levodopa. In the intestinal wall and in the liver, levodopa undergoes intensive metabolism under the action of DOPA decarboxylase, which leads to the conversion of more than 90% of the administered drug into dopamine. Dopamine formed in peripheral tissues does not penetrate the brain and causes a number of side effects. Part of levodopa is also metabolized by MAO and COMT, as a result, only 1-3% of levodopa enters the central nervous system.
To prevent decarboxylation of levodopa in peripheral tissues, DOPA decarboxylase inhibitors, which do not penetrate the blood-brain barrier, carbidopa and benserazide, are used. In this case, a larger amount of levodopa (about 10%) enters the brain tissue and reaches the site of its action. This allows you to reduce the prescribed dose of levodopa. In addition, by reducing the formation of dopamine in peripheral tissues, the peripheral side effects of levodopa are reduced.
Currently, levodopa is produced in combination with peripheral DOPA decarboxylase blockers and is part of combination
drugs Nakom, Sinemet, Duellin (levodopa and carbidopa) and Madopar (levodopa and benserazide).
Indications for the use of drugs containing levodopa are Parkinson's disease and parkinsonism (with the exception of drug-induced parkinsonism). Take medications orally only after meals. Levodopa is well absorbed from the gastrointestinal tract. The effect develops slowly (after 1 week) and reaches a maximum after 1 month. Treatment with levodopa is carried out for a long time.
When using levodopa, orthostatic hypotension, tachycardia, and cardiac arrhythmias occur, which are associated with the formation of dopamine in peripheral tissues and the effect of dopamine on blood vessels and the heart. In addition, nausea and vomiting are common side effects, which occur due to dopamine stimulation of the D2 trigger zone of the vomiting center. These effects are reduced when peripheral DOPA decarboxylase inhibitors are used concomitantly with levodopa. In addition, to prevent nausea and vomiting, a dopamine receptor blocker, domperidone, is prescribed, which does not penetrate the blood-brain barrier, but acts on the trigger zone of the vomiting center (the trigger zone of the vomiting center is not protected by the blood-brain barrier). However, domperidone does not block dopamine receptors in the neostriatum and therefore does not reduce the effectiveness of levodopa.
Side effects such as psychosis, hallucinations, insomnia, anxiety, depression, and impaired coordination of movements are associated with the action of dopamine in the central nervous system. To eliminate psychoses, the centrally acting dopamine receptor blocker clozapine (an atypical antipsychotic) is used, which blocks D4 receptors to a greater extent than D2 receptors in the central nervous system and therefore affects the effectiveness of levodopa to a lesser extent than typical antipsychotics.
Some patients with long-term use of levodopa experience dyskinesias (involuntary choreiform movements of the face, neck, and limbs). With prolonged use, an “on/off” syndrome is observed, manifested by a sudden sharp increase in the symptoms of the disease. To reduce this phenomenon, combined levodopa preparations (levodopa + benserazide and levodopa + carbidopa) with delayed release of active substances (Madopar GSS, Sinimet-SR) are used.
Contraindications include angle-closure glaucoma, diabetes mellitus, psychosis, heart rhythm disorders, liver and kidney function, pregnancy, lactation, and age under 25 years.
With long-term (more than 5 years) use of levodopa, the effectiveness decreases, which is associated with the progressive degeneration of dopaminergic neurons.
To increase the effectiveness of levodopa, in addition to DOPA decarboxylase inhibitors, COMT inhibitors are prescribed simultaneously with levodopa. One such drug is entacapone (Comtan). The drug does not penetrate the blood-brain barrier and delays the metabolism of levodopa in peripheral tissues, while the amount of levodopa entering the central nervous system increases, which makes it possible to reduce the dose of levodopa. The use of COMT inhibitors is believed to reduce the severity of the on/off syndrome.
In addition, to increase the effectiveness of treatment, levodopa is usually combined with other antiparkinsonian drugs that improve dopaminergic transmission. These include selegiline (an MAO-B inhibitor), amantadine (a drug that releases dopamine from presynaptic terminals), and dopamine receptor agonists.
Selegiline is a selective inhibitor of MAO-B, an enzyme that primarily inactivates dopamine. Selegiline, by inhibiting MAO-B, reduces the destruction of dopamine in neurons of the substantia nigra (see Fig. 13.1) and potentiates the effect of levodopa, which makes it possible to reduce the dose of levodopa by an average of 30%. Selegiline is prescribed in combination with levodopa. As monotherapy, the drug is used only in the early stages of the disease. Selegiline is believed to have a neuroprotective effect by delaying the destruction of dopaminergic neurons in the brain. This effect is explained by the fact that, by inhibiting the oxidative metabolism of dopamine, selegeline reduces the formation of free oxygen radicals, which cause the death of dopaminergic neurons.
Side effects: nausea, vomiting, hypotension, impaired concentration and confusion.
Amantadine enhances the release of dopamine from intact neurons into the synaptic cleft and disrupts the neuronal reuptake of dopamine (see Fig. 13.1). Increasing the concentration of dopamine in the central nervous system leads to a weakening of the symptoms of Parkinson's disease. In addition, it is possible that amantadine interacts with NMDA receptors on cholinergic neurons of the basal ganglia. It is believed that amantadine, by blocking these receptors, prevents the stimulating effect of glutamate on cholinergic neurons, which leads to inhibition of cholinergic transmission in the neostriatum. Amantadine is also believed to have some anticholinergic activity. The neuroprotective effect of amantadine on dopaminergic neurons of the substantia nigra is discussed, which is associated with the blockade of NMDA receptors localized on these neurons. As a result, the flow of calcium ions into nerve cells is reduced, which prevents their destruction.
Amantadine has a moderate antiparkinsonian effect. It is used for Parkinson's disease and parkinsonism (with the exception of drug-induced parkinsonism), especially with contraindications to levodopa. Amantadine is also prescribed in combination with levodopa. Addiction to the drug quickly develops.
Side effects include agitation, irritability, insomnia, dizziness, orthostatic hypotension, and convulsions.
Dopamine receptor agonists. Unlike levodopa, drugs in this group directly excite dopamine receptors in the neostriatum (see Fig. 13.1). Pergolide is a non-selective agonist of D1 and D2 receptors. Bromocriptine, pramipexole and ropinirole exhibit greater activity against class B2 dopamine receptors (pramipexole and ropinirole stimulate D2 and B3 receptors of this class). Pergolide and bromocriptine are ergot alkaloid derivatives.
Bromocriptine is a semi-synthetic derivative of the ergot alkaloid ergocryptine. The antiparkinsonian activity of bromocriptine is associated with stimulation of B2 receptors in the neostriatum. In addition, bromocriptine, by stimulating B2 receptors, reduces the release of prolactin from the anterior pituitary gland (see section 31.1.1. “Drugs of hypothalamic and pituitary hormones”).
Bromocriptine and pergolide are mainly used in combination with levodopa when satisfactory results are not obtained or in cases of on/off syndrome. Pramipexole and ropinirole are more effective than bromocriptine and are prescribed both as monotherapy and in combination with levodopa. The duration of action of dopamine receptor agonists is superior to levodopa.
At the beginning of treatment with dopamine receptor agonists, orthostatic hypotension, nausea, and vomiting occur (due to stimulation of D2 receptors in the trigger zone of the vomiting center), which can be prevented by prescribing the peripheral dopamine receptor blocker domperidone. With prolonged use, hallucinations, psychoses, and the development of dyskinesia are possible. Pramipexole and ropinirole are also characterized by increased drowsiness and sudden onset of sleep.
Drugs that inhibit cholinergic transmission
Trihexyphenidyl is a central anticholinergic blocker, blocking M1-cholinergic receptors of the neostriatum, reduces the symptoms of parkinsonism. The drug has a moderate antiparkinsonian effect. Mainly reduces tremor and muscle rigidity, with little effect on bradykinesia.
Biperiden is a central anticholinergic blocker, similar in properties to trihexyphenidyl.
Indications for the use of central anticholinergic drugs: early stages of Darkinson's disease and parkinsonism. Used for drug-induced parkinsonism, in particular, prescribed for the prevention and elimination of extrapyramidal disorders caused by antipsychotic drugs.
Side effects associated with blockade of peripheral M-cholinergic receptors: disturbance of accommodation, dry mouth, palpitations, constipation, urinary retention. Side effects associated with blockade of central M-cholinergic receptors are impaired memory and concentration, especially in elderly patients. In case of an overdose, agitation and hallucinations are possible.
Contraindications: glaucoma, prostate hypertrophy, hypersensitivity to the drug, breastfeeding.
Interaction of antiparkinsonian drugs with other drugs
| Antiparkinsonian drugs | Interacting drug (group of drugs) | Result of interaction |
| Levodopa | Benzodiazepines | Weakening the anxiolytic effect |
| Inhalation drugs for anesthesia | Increased risk of cardiac arrhythmia | |
| MAO inhibitors | Increased blood pressure | |
| Antihypertensive drugs | Potentiation of the hypotensive effect | |
| Iron supplements | Decreased iron absorption | |
| Metoclopramide | Increased plasma concentrations and toxicity of levodopa | |
| Selegilin | Increased risk of dyskinesia, nausea, orthostatic hypotension, hallucinations | |
| Pyridoxine | Activation of DOPA decarboxylase, decrease in levodopa concentration | |
| Bromocriptine | Antibiotics – macrolides | Increased plasma concentrations of bromocriptine |
| Metoclopramide, Domperidone | Reduction of hypoprolactinemia caused by bromocriptine | |
| Antipsychotics | Antagonism with the hypoprolactinemic and antiparkinsonian effects of bromocriptine | |
| Trihexyphenidyl, Biperiden | Anticholinergics and other drugs with anticholinergic activity | Potentiation of anticholinergic action |
Basic drugs
| International nonproprietary name | Patented (trading) titles | Release forms | Patient Information |
| Levodopa | Nakom, Sine-met, Duellin (levodopa + car-bidopa), Mado-par (levodopa + benserazide) | Tablets of 0.1, 0.125, 0.15, 0.2 and 0.25 g of levodopa | It is administered orally, the initial dose is 125 mg of levodopa 3-4 times a day, the daily dose is 750 mg-1.5 g in several doses after meals. |
| Selegilinum | Deprenil, Eldepril, Yumex | Tablets of 0.005 g in packs of 50 and 1000 pcs. | Take orally, starting with 5 mg in the morning (with breakfast); if there is no result, the dose is increased to 10 mg per day |
| Amantadine (Amantadinum) | Midantan | Tablets of 0.1 g in a package of 100 pcs. | Take orally, after meals, starting with 50-100 mg 2 times, then 3-4 times a day. The daily dose is 200-400 mg. Course – 2-4 months |
| Bromocriptine (Bromocripti- num) | Parlodel | Tablets of 0.0025 g of bromocriptine monosulfonate in bottles of 100, 500 or 1000 pcs. | Taken orally with meals - the initial dose is 1.25 mg at bedtime, followed by an increase after 2-3 days to 1.25 mg 2 times a day. If necessary, the dose is increased every 2-4 weeks by 2.5 mg per day. The average effective dose is 10 mg, the maximum is 40 mg/day. Incompatible with alcohol |
| Trihexyphenidyl (Trihexyphe-nidylum) | Cyclodol | Tablets of 0.002 g in a package of 50 pcs. | Taken orally, starting from 10 mg/day; increasing the dose by 2 mg/day. The usual maintenance daily dose is 6-10 mg (less for the elderly), in severe cases - 12-15 mg/day in 3-4 doses. Higher doses: single - 10 mg, daily - 20 mg |
Additional research methods
At the moment, there are no laboratory or instrumental research methods that would be mandatory for every patient with suspected PD. In recent years, patients with PD have often undergone CT or MRI of the brain, but most often this is not necessary, and in most cases the diagnosis can be made based on clinical findings. However, if the clinical picture in a patient with parkinsonism syndrome deviates from the classic variant characteristic of PD, in particular, there is no typical response to dopaminergic drugs, then neuroimaging is necessary.
When the onset of the disease is before 50 years of age, it is important to exclude hepatolenticular degeneration, which may be indicated by a corneal Kayser-Fleischer ring, low ceruloplasmin levels, increased signal intensity from the basal ganglia and cerebellum on T2-weighted MRI images, and increased urinary copper excretion.
Transcranial sonography of the deep structures of the brain may also have diagnostic significance, revealing in PD hyperechoic changes in the projection of the substantia nigra, associated with the accumulation of iron and established in 92% of cases of clinically probable PD, but its results can only be interpreted in a clinical context.
Of the practically important, but not yet available in our country, diagnostic methods include positron emission tomography (PET) and single-photon emission computed tomography (SPECT), which make it possible to study synaptic transmission at all levels, as well as monitor the pathological process. When detecting a decrease in the accumulation of F18-fluorodopa with PET and β-CIT with SPECT in the striatum, we can talk about the involvement of presynaptic nigrostriatal terminals in the pathological process (primary parkinsonism). Determination of decreased accumulation of 11C-raclopride (D2 receptor ligand) in PET will indicate a decrease in the number of dopamine receptors in the striatum (parkinsonism “plus”).
General principles for starting treatment
Since at the moment the ability to slow down the process of degeneration due to the neuroprotective effect (the ability to protect intact cells from damage) or the neuroreparative effect (the ability to restore the activity of partially damaged cells) has not been convincingly proven in any of the drugs used, treatment is still based on symptomatic action. However, the potential for a neuroprotective effect, supported by experimental or clinical data, should be taken into account when prescribing treatment.
Currently, a widely accepted concept emphasizes the importance of early administration of dopaminergic therapy - immediately after diagnosis - in order to more quickly correct neurochemical imbalances in the brain and support compensation processes.
If previously the need for maintaining monotherapy as long as possible was emphasized, at present the advantages of this approach do not seem obvious - compared with an early transition to a combination of drugs with different mechanisms of action. The need for monotherapy or combination therapy should be decided individually. In any case, when choosing drugs and their dosage, one should strive not for complete elimination of symptoms, but for a significant improvement in function, allowing one to maintain everyday and professional activity. At the same time, you should avoid making several changes to the treatment regimen at once (for example, increasing the dose of several drugs at once or adding several drugs at once), this allows you to separately evaluate the effectiveness and safety of each of the prescribed drugs.
Principles for choosing an antiparkinsonian drug
The choice of drug at the initial stage of treatment is carried out taking into account age, severity of the motor defect, labor status, state of neuropsychological functions, the presence of concomitant somatic diseases, and the individual sensitivity of the patient. In addition to achieving optimal symptom control, the choice of drug is determined by the need to delay the development of motor fluctuations and dyskinesias (Table 2).
Table 2. Choice of drug for initial treatment of Parkinson's disease.
| Drugs | Can be used as first choice | Degree of symptomatic improvement | Neuroprotective potential | Risk of side effects | |
| Fluctuations and dyskinesias | Other side effects | ||||
| Levodopa | + | +++ | +? | ↑ | ↑ |
| Dopamine receptor agonists | + | ++ | +? | ↓ | ↑ |
| MAO B inhibitor | + | + | +? | ↓ | ↑ |
| Amantadine | + | + | +? | ↓ | ↑ |
| Anticholinergics | — | + | — | ? | ↑ |
In persons under 50 years of age with mild or moderate motor impairment in the absence of severe cognitive impairment, one of the following drugs is prescribed: dopamine receptor agonist, monoamine oxidase type B inhibitor, amantadine. For a milder motor defect, an MAO B inhibitor may be prescribed; for a more severe defect, it is preferable to start with treatment with one of the dopamine receptor agonists. Non-ergoline agonists (eg, pramipexole, ropinirole, rotigotine or pronoran) are preferred over ergoline agonists (bromocriptine, cabergoline) due to their more favorable side effect profile. If one of the dopamine receptor agonists is insufficiently effective or poorly tolerated, another dopamine receptor agonist or a drug from a different pharmacological group can be tried. A combination of a dopamine receptor agonist, MAO type B inhibitor and amantadine is rational, which should be switched to gradually, adding a drug of a new group if the previously prescribed drug did not provide the expected effect.
Anticholinergic drugs (for example, biperiden) are indicated in the presence of severe resting tremor or painful dystonia, provided that neuropsychological functions are preserved. It is advisable to add them to the combination of a dopamine receptor agonist with an MAO B inhibitor and/or amantadine, if in a relatively young patient it did not suppress tremor to the extent necessary to maintain his ability to work.
If these drugs in maximum tolerated doses and their combination do not provide an adequate state of motor functions and social adaptation of patients, levodopa is prescribed in the minimum effective dose [4].
In persons aged 50–70 years with a moderate motor defect and relative preservation of cognitive functions, treatment begins with an MAO type B inhibitor (for mild symptoms of parkinsonism) or one of the dopamine receptor agonists. In the future, it is advisable to gradually switch to a combination of a dopamine receptor agonist, an MAO type B inhibitor and amantadine (provided that it is well tolerated). Anticholinergics should generally not be prescribed to patients over 60 years of age due to the risk of cognitive decline and other side effects. If the combination of the above drugs is insufficiently effective, levodopa is added in the minimum effective dose (200–400 mg per day).
In persons aged 50–70 years with a pronounced motor defect that limits the ability to work and/or the ability to self-care, as well as in the presence of severe cognitive impairment and the need to obtain a quick effect, treatment begins with drugs containing levodopa. If small to moderate doses of levodopa (300–500 mg levodopa per day) do not provide the necessary improvement, a dopamine receptor agonist, amantadine, and an MAO B inhibitor may be added sequentially.
In elderly people (over 70 years of age), especially in the presence of severe cognitive decline and somatic burden, treatment should begin with levodopa. The age limits indicated are relative, and the general principle is rather that the younger the patient, the later levodopa should be administered. In addition, it is not so much the chronological, but the biological age of the patients that plays a decisive role.
Rules for prescribing and side effects of antiparkinsonian drugs
Since we are talking about specific drugs and their combinations, it is important to consider several points:
- clinical course and severity of symptoms;
- the degree of effectiveness of each drug when taken in a particular patient;
- presence or absence of side effects.
If Parkinson's disease began at a relatively young age (before age 50), the first drug to consider is a dopamine receptor antagonist. With late development of the disease (aged 70 years and older), preference should be given to levodopa drugs.
Of course, levodopa should be considered as a kind of “gold standard”, but, unfortunately, it always gives a number of complications in the form of fluctuations in its effect and motor disorders. At first, the patient feels how the effect of the drug ends, and later he experiences “on-off” phenomena. When motor fluctuations appear, patients may experience side effects from the mental, autonomic and sensory spheres. One should also take into account the phenomenon of so-called drug dyskinesia, when a person experiences a series of strange violent movements that he cannot control. As a rule, this phenomenon occurs in the later stages of the disease and marks the peak of the drug's effect.
For severe complications associated with the use of levodopa, it is recommended to resort to methods that stimulate dopamine receptors in the body. We are talking about the introduction of a levodopa-based gel through a gastrostomy tube. Subcutaneous administration of apomorphine is also allowed.
If you have to resort to intraduodenal administration of the drug, you need to periodically show the patient to the surgeon to avoid typical complications. Subcutaneous administration of apomorphine is a more gentle treatment option, although there are side effects in this case.
Use of extended-release pramipexole in early PD
The development of new dosage forms of antiparkinsonian drugs that provide them with a prolonged release and allow a single dose during the day not only makes treatment more convenient, but also, by improving patient adherence to treatment, increases the long-term effectiveness of therapy. In addition, with a slow release of the drug throughout the day, a more stable concentration in the blood is achieved, which can ensure better tolerability and effective control of disease symptoms throughout the day (both during the day and at night).
A new dosage form of pramipexole with prolonged (controlled) release, which involves a single dose during the day, has been used in European countries and the USA since 2009, and in our country - since 2012. It is a matrix tablet in which the active substance is evenly distributed in a polymer matrix. In the gastrointestinal tract, the matrix absorbs liquid and turns into a gel, which uniformly releases pramipexole over 24 hours. Since pramipexole is highly soluble in a liquid medium, regardless of its pH, the active substance is released from the matrix and absorbed throughout the intestine. The rate of gastric emptying and intestinal motility do not significantly affect the effect of the drug. Absorption parameters also do not depend on whether the drug is taken on an empty stomach or after a meal [2].
When developing a new dosage form, the possibility of a simple, immediate transition from the traditional form of the drug to the new one was taken into account. The condition for this is that equal daily doses of immediate release (taken 3 times a day) and extended release (taken once a day) have the same antiparkinsonian effect. The difference between the new and traditional dosage forms of pramipexole lies only in the rate of release of the active substance. The half-life of pramipexole is the same when using both forms, but controlled release ensures longer maintenance of therapeutic drug concentrations in the blood [5].
The equivalence of equal daily doses of immediate- and extended-release pramipexole has been demonstrated in a number of clinical trials.
It is worth emphasizing the particular convenience of the new dosage form of pramipexole, which can be taken once a day, for patients with early stage PD who continue to work. To avoid side effects, the drug is prescribed by slow titration - according to the same scheme as the immediate-release drug. For this purpose, extended-release pramipexole tablets are available in several strengths: 0.375, 0.75, 1.5, 3 and 4.5 mg. Treatment begins with a dose of 0.375 mg once a day, then, subject to good tolerance, every 7 days they move to the next dose level until the optimal effect is achieved, up to a maximum of 4.5 mg/day (Table 3). After reaching a dose of 1.5 mg/day, it is sometimes advisable to titrate more slowly, since the development of the full therapeutic effect may require several weeks. The recommended dose for maintenance therapy (both in early and in advanced or late stages of the disease) can range from 0.375 to 4.5 mg/day. The most commonly used dose is 3 mg/day.
Table 3. Titration schedule for extended-release pramipexole.
| A week | Dose |
| 1st | 0.375 mg 1 time per day |
| 2nd | 0.75 mg 1 time per day |
| 3rd | 1.5 mg 1 time per day |
| 4th | 2.25 mg 1 time per day |
| 5th | 3 mg 1 time per day |
| 6th | 3.75 mg 1 time per day |
| 7th | 4.5 mg 1 time per day |
Standards of treatment for Parkinson's disease
Treatment for the appearance of motor fluctuations and/or dyskinesias
Reducing the duration of action of drugs containing levodopa.
If the symptoms of parkinsonism increase towards the end of the next dose of a drug containing levodopa, resort to one of the following measures:
- increasing the frequency of administration of a product containing levodopa up to 4–6 times while maintaining the same daily dose or its minimal increase (level of evidence C);
- partial replacement of a standard levodopa-containing preparation with a sustained-release levodopa-containing preparation (level B);
- adding one of the dopamine receptor agonists - pramipexole, piribedil or bromocriptine (level B);
- addition of MAO type B inhibitor selegiline or amantadine (level C);
- addition of the catechol-O-methyltransferase (COMT) inhibitor entacapone or tolcapone (Level A).
If the chosen measure is ineffective, a combination of drugs should be used (level C).
Slow onset or lack of effect of a single dose of a drug containing levodopa.
If individual doses of levodopa taken throughout the day are ineffective, it is recommended:
- taking a drug containing levodopa on an empty stomach (at least 45 minutes before meals) (level C);
- taking levodopa in dissolved form (level C);
- prescribing drugs that enhance gastric motility - for example, domperidone (level C).
Unpredictable fluctuations in the effect of a single dose of products containing levodopa throughout the day (on-off syndrome).
If episodes of sudden worsening of parkinsonian symptoms occur during the next dose of levodopa, the following should be done:
- assess the adequacy of levodopa doses (excessively small doses do not provide a full long-term effect) (level C);
- increase the single dose of levodopa, extending the interval between doses of the drug to 4–5 hours (level C);
- add one of the dopamine receptor agonists (level B);
- take a product containing levodopa 45–60 minutes before meals, limit protein intake during the day, prescribe drugs that enhance gastrointestinal motility (domperidone) (level C);
- in case of prolonged switching off, take the drug levodopa in dissolved form (level C).
In addition, measures similar to those recommended are indicated if the onset is delayed or there is no effect of a single dose of a drug containing levodopa.
Violent movements at the height of a single dose of a drug containing levodopa (peak dose dyskinesia).
If, at the height of the action of the levodopa drug, violent movements appear that limit the patient’s life activity, the following actions should be taken:
- add amantadine (level A);
- reduce the single dose of levodopa, compensating for this by increasing the number of doses, adding or increasing the dose of a dopamine receptor agonist (level C);
- reduce the dose or discontinue selegiline, a COMT inhibitor and anticholinergic agent (Level C);
- partially replace the standard levodopa-containing drug with a sustained-release drug (this may increase the duration of violent movements, which requires discontinuation of the sustained-release drug) (level C);
- add clonazepam (level C);
- add clozapine (in most severe cases) (level C).
Violent movements at the beginning and end of a single dose of a drug containing levodopa (biphasic dyskinesias).
For biphasic dyskinesias, the following measures should be taken:
- increase the single dose of levodopa, if necessary, reducing the number of doses (the next dose should be taken no earlier than the full cycle of dyskinesias is completed) (level C);
- add one of the dopamine receptor agonists, maintaining or reducing the dose of levodopa (level C);
- discontinue sustained-release levodopa-containing product (Level C).
Dystonia caused by the cessation of the next dose of a drug containing levodopa.
For painful dystonia caused by stopping the action of the next dose of a drug containing levodopa, the following measures are necessary:
- increasing the number of doses containing levodopa (level C);
- addition of a sustained-release levodopa-containing agent or partial replacement of the standard agent with a sustained-release agent (Level B);
- adding one of the dopamine receptor agonists (level B);
- taking a product containing levodopa in dissolved form (level B);
- additional administration of an anticholinergic drug (in the absence of cognitive impairment), baclofen, clonazepam, tizanidine, lithium, or injection of botulinum toxin into the muscles involved in hyperkinesis (level C).
If, despite the correction of the regimen for taking antiparkinsonian drugs, involuntary movements or instability of the effect of drugs containing levodopa persist, which significantly limit the patient’s life activity (reduce the ability to work or the ability to self-care), a consultation with a neurosurgeon specializing in stereotactic neurosurgery is indicated to decide on the advisability of neurosurgical intervention .
Treatment of sleep disorders
When awakenings caused by increased symptoms of parkinsonism at night (nocturnal akinesia), resort to one of the following measures:
- increasing the evening dose of a product containing levodopa (level B);
- replacing the standard levodopa drug with a sustained-release agent in the evening (level C);
- administration of a dopamine receptor agonist immediately before bedtime (level C).
For nocturnal akathisia, reduce the evening dose of a drug containing levodopa (level C), and if this measure is insufficient, then clonazepam is prescribed at night (level C). If these measures are ineffective, zolpidem 10-20 mg at night (level C), an antidepressant with a sedative effect (trazodone - 75-150 mg, amitriptyline - 25-50 mg or mirtazapine - 15-30 mg) (level C) are additionally prescribed.
Treatment of PD patients with cognitive impairment
Deterioration of cognitive functions requires, first of all, optimization of antiparkinsonian therapy to ensure an adequate level of motor functions. The main antiparkinsonian drug in patients with severe cognitive impairment should be drugs containing levodopa, which are less likely to cause side effects in this category of patients (level C). The use of anticholinergic drugs is contraindicated due to the high risk of deterioration of mental functions and the development of psychotic disorders (level B).
In addition, if cognitive functions deteriorate, the following is necessary:
- identification and correction of concomitant diseases that can worsen mental status (intercurrent infections, hypothyroidism, somatic diseases, etc.);
- withdrawal of drugs that can increase cognitive impairment (including drugs with anticholinergic effects, benzodiazepines, etc.);
- after consultation with a psychiatrist, correction of affective disorders with antidepressants that do not have anticholinergic or sedative effects, preferably with selective serotonin reuptake inhibitors with a stimulating effect, in particular citalopram, sertraline or fluoxetine (regular clinical monitoring is necessary due to the possible deterioration of motor functions) .
To improve cognitive functions in PD patients with dementia, the following can be used:
- central cholinesterase inhibitors: rivastigmine, 3–12 mg/day in 2 divided doses (level A), galantamine, 8–24 mg/day in 2 divided doses (level C);
- NMDA-glutamate receptor blocker memantine, 10–30 mg in 1–2 doses (level C).
Consultation with a psychiatrist and observation of patients with mental disorders are indicated for the development of severe psychotic disorders (depression, psychopathic-like disorders, hallucinosis, paranoid syndrome, delirium).
In case of visual hallucinations against the background of clear consciousness, preservation of orientation and criticism, a planned correction of antiparkinsonian therapy is carried out (level B). First, reduce the dose or discontinue the recently prescribed or least effective drug (level B), often in the following order: anticholinergic - selegiline - amantadine - dopamine receptor agonist - COMT inhibitor (level C).
If hallucinations persist, the dose of the drug containing levodopa should be reduced to the minimum effective level that provides the required level of motor activity (level B). If this measure is ineffective or it is impossible to reduce the dose of a drug containing levodopa due to an increase in the motor defect, clozapine is prescribed at a dose of 6.25 to 50 mg at night (level B); after regression of hallucinosis, the drug is gradually discontinued over 2–3 weeks (level C). During the entire period of treatment with clozapine, it is necessary to examine the content of leukocytes in the blood once a week. If their level decreases below 3 thousand/µl, the drug should be discontinued.
If clozapine is ineffective or intolerable, quetiapine, 25–200 mg/day (level C), a cholinesterase inhibitor (level C), may be prescribed instead.
When visual hallucinations are combined with delusional disorders or when they occur against the background of confusion with the development of delirium, it is necessary, in addition to the above measures, the following:
- organize constant monitoring of the patient;
- identify provoking factors - infection, trauma, somatic and cerebrovascular diseases, etc. - and begin their treatment;
- reduce the dose or gradually discontinue medications, the use of which could cause psychotic disorders (anticholinergics, selegiline, amantadine, dopamine receptor agonist, COMT inhibitor);
- reduce the dose of levodopa to the minimum effective level and ensure control over its regular use;
- arrange a consultation with a psychiatrist and consider hospitalization in a psychosomatic department.
Long-acting benzodiazepines (diazepam, chlordiazepoxide, etc.), which can cause confusion, should be avoided at night.
Treatment of akinetic crisis
Akinetic crisis is a sudden persistent increase in hypokinesia and rigidity with the development of immobility and disturbances of bulbar functions (dysarthria and dysphagia), occurring spontaneously or associated with cessation of use, a reduction in the dose of drugs containing levodopa, impaired absorption in the gastrointestinal tract, or the development of intercurrent infection.
Treatment is carried out in a hospital setting. The causes of the akinetic crisis are being investigated (cessation of taking or reducing the dose of antiparkinsonian drugs, gastrointestinal disease causing malabsorption of levodopa drugs, intercurrent infection, cerebrovascular disease, decompensation of somatic disease).
Drug therapy is prescribed individually based on medical history and daily examination of the patient. Dysphagia requires the insertion of a nasogastric tube for feeding and medication administration. A set of measures to prevent bedsores is indicated, primarily turning in bed every 2 hours, regular treatment of bone protrusions with camphor alcohol, and the use of anti-bedsore mattresses.
If an akinetic crisis occurs as a result of sudden cessation of taking a drug containing levodopa, it should be re-prescribed at a lower dose (50-100 mg 3-4 times a day), then gradually increase the dose every 3 days until the effect is achieved (but not more than than up to 700–800 mg levodopa per day) (level C).
If an akinetic crisis occurs as a result of a dose reduction, then it should be increased by 100 mg every 3 days until the effect is achieved (but not more than 700–800 mg of levodopa per day) (level C).
For dysphagia (but with normal gastrointestinal function), levodopa drugs are administered in dissolved form through a tube.
As an additional remedy, especially in case of impaired swallowing and absorption of drugs in the gastrointestinal tract, amantadine sulfate is prescribed - 200 mg/500 ml IV drip at a rate of 60 drops per 1 min 1-2 times a day for 5-10 days (level C) followed by a mandatory transition to oral amantadine (100–200 mg 3 times a day).
In case of dehydration, in order to achieve euvolemia, saline solution, Ringer's solution, 0.45% sodium chloride solution and 5% glucose solution, albumin solution, Reopoliglucin (level C) are administered.
To prevent thrombosis of the deep veins of the leg and thromboembolic complications, the administration of direct anticoagulants (Heparin, 2.5–5 thousand units subcutaneously 2 times a day or Fraxiparine 0.3 ml subcutaneously 2 times a day) is indicated until the resolution of the akinetic crisis (level C).
Until swallowing is restored, nutrition is administered through a nasogastric tube. If the function of the gastrointestinal tract is impaired, parenteral nutrition is performed.
If respiratory failure, acute heart failure and severe dysphagia occur, creating a threat of aspiration, the patient is transferred to the intensive care unit, where intubation is performed, and, if necessary, artificial ventilation. Rehabilitation, including therapeutic exercises and massage, is carried out after the crisis has stopped and the condition has stabilized.
For questions regarding literature, please contact the editor.
O. S. Levin,
Doctor of Medical Sciences, Professor RMAPO, Center for Extrapyramidal Diseases, Moscow
Continued. For the beginning, see: Attending Physician. 2007. No. 8
Medicines that have not been proven to be effective in PD
In clinical practice, medications are widely used whose effectiveness in PD has not been proven and which, therefore, cannot be recommended for use in this disease. First of all, these include the so-called nootropic, neurometabolic and vasoactive drugs. It is possible that some of these drugs have some therapeutic effect, but before recommending a specific drug, an adequate assessment of its effectiveness should be carried out. Specialists involved in the treatment of PD are well aware that a certain proportion of patients respond well to placebo, and this effect is not durable. Accordingly, the costs of such treatment turn out to be meaningless.
Literature
- Golubev V.L., Levin Ya.I., Vein A.M. Parkinson's disease and parkinsonism syndrome. M.: MEDpress-inform, 1999.
- Levin O.S., Fedorova N.V., Smolentseva I.G. Dopamine receptor agonists in the treatment of Parkinson's disease. Rus. honey. magazine 2000; 15–16: 643–646.
- Levin O.S., Fedorova N.V. Parkinson's disease. M.: MEDpress-inform, 2011.
- Patient management protocol. Parkinson's disease. Problem standardization in healthcare. 2005; 3: 74–166.
- Chwieduk CM, Curran MP Pramipexole extended release in Parkinson's disease. CNS Drugs 2010; 24: 327–336.
- Grosset KA, Bone, Grosset DG Suboptimal medication adherence in Parkinson's disease. Mov. Discord. 2005; 20: 1502–1507.
- Hauser R., Salin L., Koester J. Double-blind evaluation of pramipexole extended-release (ER) in early Parkinson's disease. Neurology 2009; 72(11 Suppl. 3):A412–413.
- Kvernmo T., Härtter S., Bürger E. A review of the receptor-binding and pharmacokinetic properties of dopamine agonists. Clin. Therap. 2006; 28:1065–1078.
- Mizuno Y., Yamamoto M., Kuno S. et al. Efficacy of Pramipexole Extended Release (ER) and switching from Pramipexole Immediate Release (IR) to ER in Japanese advanced Parkinson's disease (PD) patients. In: XVIII WFN World Congress on Parkinson's Disease and Related Disorders: Miami Beach, 2009: Poster 2.192.
- Möller JC, Oertel WH Pramipexole in the treatment of Parkinson's disease: new developments. Expert Rev. Neurother. 2005; 5:581–586.
- Poewe W., Rascol O., Barone P. et al. Pramipexole extended-release in early Parkinson's disease. Neurology 2011; 77:759–766.