Perinatal encephalopathy of newborns is an unclassified non-inflammatory disorder of the nervous system observed during pregnancy or immediately after birth.
The disease is called unclassifiable because encephalopathy is not detected by traditional tests. Even high-tech research does not provide a complete objective picture.
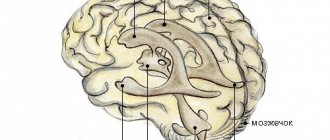
The concept of perinatal encephalopathy (PE) is excluded from the International Classification. Today, encephalopathy is defined as the consequences of damage to the fetal brain. If we adhere to the accuracy of terminology, then encephalopathy can be called a consequence of destructive manifestations that destroy the cerebral cortex.
Causes of perinatal encephalopathy.
Signs of pathology are often vague. To identify the problem, dynamic observation over a long period of time is sometimes required. There is evidence that at the initial appointment with a neurologist, up to 80% of children receive a diagnosis of PPE or “unspecified perinatal encephalopathy.” It is reassuring to know that by the age of one year, most children are cleared of their diagnosis. This can be explained by the lack of clear diagnostic criteria and the mobility of the infant’s neuropsychological structure. Perinatal encephalopathy is an organic and functional disorder of the brain in children during the days of intrauterine development and the first hours of life. The time limits are determined as follows: from the 28th week of pregnancy to the 7th day after birth. In premature babies, the period is extended to 28 days.
The seriousness of the disease and the difficulty of diagnosis are not a death sentence. The main factors that cause the disease still exist:
- Hypoxia is a lack of oxygen and is ischemic in nature. When oxygen supply stops, the blood stops supplying food and fills with carbon dioxide. This compound provokes cell oxidation. As a result, acidosis appears (body oxidation syndrome) - a disorder of the acid-base balance. Its most dangerous consequence is swelling.
Hypoxia can have both destructive and restorative effects. Immediately after the baby leaves the womb, acidosis acts as a means of adaptation to changes in its environment. When its form is prolonged, encephalopathy of newborns manifests itself.
With a complicated birth, asphyxia occurs - oxygen starvation of the children's brain. Then uncompensated acidosis may occur. As a result of a disruption in the blood supply to the brain, the acid-base balance changes (it is measured by pH). If the baby has uncompensated acidosis, the indicator drops below 7.1, which requires immediate resuscitation measures.
- Cranial trauma. It entails post-traumatic encephalopathy. As a result of a difficult birth, the child experiences mental and physical disorders. Depending on the severity of the injury, neonatal encephalopathy can be expressed in different forms.
- Damage to the frontal or temporal lobes of the brain at the time of birth;
- Swelling of the brain, disruption of the blood supply to cells by connecting material: this causes adhesions and scars;
- Autoneurosensitization is a conflict of the immune system: it mistakenly begins to react to its own cells as a foreign object.
- Toxic-metabolic syndrome is the result of the toxic effects of the metabolic activity of unhealthy kidneys and biliary tract in children. Bilirubin encephalopathy (jaundice of newborns), i.e. bilirubin intoxication, is quite widespread. Bilirubin is a neurotoxic poison that leads to damage to the cerebral cortex and subcortical nuclei. Depending on the causes, there are several types of jaundice in newborns: conjugative (low binding capacity of the liver), hemolytic (caused by hemolysis - destruction of red blood cells), obstructive (problems with the outflow of bile), parenchymal.
- Intrauterine infections infect the newborn and provoke inflammatory processes. Infection of the fetus can lead to serious pathology of the nervous system, perinatal encephalopathy, premature birth and even the death of the child.
- Disruption of uteroplacental blood flow (fetoplacental insufficiency) is a failure of blood circulation in the placenta in the late period of gestation. Through this protective shell the fetus is nourished, supplied with oxygen, and hormonal exchange occurs. When the dysfunction is insignificant, the danger is minimal, but with severe fetoplacental insufficiency, hypoxia occurs, followed by encephalopathy.
- Severe chronic or acute illness of the mother also negatively affects the child. Preeclampsia is a complication of the late period of pregnancy, it is called late toxicosis. As a result of the disease, the internal structures of the mother (kidneys, liver, blood circulation) are damaged.
- The threat of termination of pregnancy is fraught with many negative side effects, including the above factors.
Causes
Hypoxic encephalopathy in adults and children occurs for different reasons. It is important to know them in order to take all measures to prevent it.
In adults
Hypoxic ischemic encephalopathy occurs due to a lack of oxygen, which is caused by the following reasons:
- state of suffocation;
- strangulation;
- failure of the respiratory system of any kind;
- drug addiction, overdose;
- pathologies of the circulatory system, leading to its obstruction or rupture;
- cyanide, carbon monoxide - poisoning;
- long stay in a smoky place;
- tracheal injury;
- heart failure;
- diseases leading to paralysis of the muscle tissue of the respiratory system.
Acute hypoxic encephalopathy occurs if oxygen does not enter the body for several minutes. This is a severe course of the pathology, which most often ends in death. Isolated cases have been recorded where people survived, but for them it ended in a severe form of serious mental illness.
In newborns
The cause of this condition in a newly born child may be:
- suffocation during childbirth due to weak labor;
- premature labor or with pathological factors such as umbilical cord prolapse;
- diseases of infectious origin in the mother;
- a number of physical factors from dirty air to radiation.
It is asphyxia in infants that is the most common factor leading to HIE. Doctors identify the following risk factors for its occurrence:
- acute hypotension in a woman in labor;
- underdevelopment of the lungs, which leads to a lack of oxygen in the blood;
- difficulties in the functioning of the heart;
- injury to the fetus due to the mother’s narrow pelvis or due to problems with the umbilical cord;
- difficulties in labor, trauma, stress;
- hypoxia;
- birth hemorrhage;
- negligence of medical personnel;
- placental abruption;
- change in the shape of the fetal skull due to pressure;
- birth trauma, uterine rupture;
- low placenta previa.
WE RECOMMEND SEEING: Causes of cystic atrophic changes in the brain
Diagnosis of encephalopathy.
Symptoms in children do not appear immediately. Immediately establishing the level and nature of the problem in the first days after birth can be difficult.
Sometimes natural manifestations of the nervous organization of a newborn are mistaken for symptoms of encephalopathy, in other cases the disease goes unnoticed. Objective conclusions can often be drawn only after six months. According to the rules, a child is examined by a doctor every month in the first half of his life. The doctor examines the baby’s reflexes and determines the quality of his physical development. In a fairly short period of time, it is possible not only to diagnose an anomaly, but also to successfully correct it. Long-term follow-up may be required so that the diagnosis does not give rise to doubts, and the development of a treatment regimen for the disease becomes possible.
The depth of damage to a child’s brain varies. Depending on the severity of the disease, 3 levels of brain destruction with long-term consequences have been established:
- The initial stage of the disease is characterized by a slight slowdown in the motor development of children for more than 2 weeks. In the first degree, fortunately, the brain substances are not affected.
- Deviations of moderate severity are determined by the presence of convulsions when crying, the baby’s motor skills are 8 weeks behind, hyperexcitability, cyanosis with short crying, “marbling” of the skin, twitching of the arms and legs. Muscle hypertonicity develops, adaptation syndromes are revealed. A year later, the disease “offers” new symptoms (when trying to walk, the child leans on his toe). Lack of treatment in the future threatens serious deviations.
- Deep brain damage results in cerebral palsy (CP) and autism. The help of restorative medicine should be resorted to as early as possible.
Causes and stages of hypoxic-ischemic damage
Perinatal damage to the central nervous system in newborns is formed under the influence of unfavorable factors in utero, during childbirth, or during the newborn period. The reasons for these changes may be:
- Disorders of blood flow in the uterus and placenta, bleeding in pregnant women, pathology of the placenta (thrombosis), delayed fetal development;
- Smoking, drinking alcohol, taking certain medications during pregnancy;
- Massive bleeding during childbirth, entanglement of the umbilical cord around the fetal neck, severe bradycardia and hypotension in the baby, birth injuries;
- After childbirth - hypotension in the newborn, congenital heart defects, disseminated intravascular coagulation syndrome, episodes of respiratory arrest, pulmonary dysfunction.
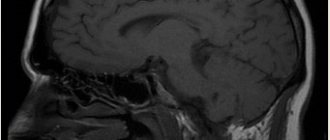
example of hypoxic-ischemic brain damage
The initial point in the development of HIE is a deficiency of oxygen in the arterial blood, which provokes metabolic pathology in the nervous tissue, the death of individual neurons or entire groups of them. The brain becomes extremely sensitive to fluctuations in blood pressure, and hypotension only worsens existing lesions.
Against the background of metabolic disorders, tissue “acidification” occurs (acidosis), edema and swelling of the brain increases, and intracranial pressure increases. These processes provoke widespread necrosis of neurons.
Severe asphyxia also affects the functioning of other internal organs. Thus, systemic hypoxia causes acute renal failure due to necrosis of the tubular epithelium, necrotic changes in the intestinal mucosa, and liver damage.
In full-term infants, post-hypoxic damage is noted mainly in the area of the cortex, subcortical structures, and brain stem; in premature infants, due to the maturation of the nervous tissue and vascular component, periventricular leukomalacia is diagnosed, when necrosis is concentrated mainly around the lateral ventricles of the brain.
Depending on the depth of cerebral ischemia, several degrees of severity of hypoxic encephalopathy are distinguished:
- The first degree is mild - transient disorders of the neurological status, lasting no more than a week.
- HIE of the second degree - lasts longer than 7 days and is manifested by depression or excitation of the central nervous system, convulsive syndrome, temporary increase in intracranial pressure, autonomic dysfunction.
- A severe form of hypoxic-ischemic injury is a disorder of consciousness (stupor, coma), convulsions, manifestations of cerebral edema with brain stem symptoms and disruption of the functioning of vital organs.
What should alert parents?
The peculiarity of encephalopathy is the need for the earliest possible start of stabilization and elimination of neurological defects of the fetus.
Emerging syndromes can be stopped and corrected during pregnancy and infancy, but qualified assistance from a neurologist is required.
Particular responsibility falls on parents. One of the features of the child’s behavior or well-being should cause concern:
- sleep disorders;
- muscle hypertonicity;
- poor coordination;
- lethargy of the hands;
- does not turn over;
- legs are not involved in crawling;
- does not sit down or stand up;
- improper crawling;
- increased excitability to various stimuli (frequently cries);
- depressed appearance in the waking phase;
- delayed motor development syndrome (cannot pick up a toy);
- can only do pull-ups with his right arm;
- spitting up like a fountain after eating;
- tremor – fine muscle trembling;
- body weight slowly increases;
Such symptoms force you to go to the clinic. Important preventive measures should not be neglected, even if the child seems to be healthy.
What is important to do in time:
- Thorough examination by a neurologist at the age of 4 weeks.
- Regular monthly examination by a pediatrician, and if necessary, treatment of the disease.
- Do a neurosonography test - NSG (establishes movement disorder syndrome).
If the presence of cerebral palsy or epilepsy has already been established, it is necessary to begin treatment as quickly as possible to prevent further pathology.
Osteopathy in the correction of neonatal encephalopathy.
Organic disorders of brain development in infants must be identified and treated immediately.
Due to neural disorders, diseases of the child’s internal organs occur. The damaged network begins to control the entire body. The opposite effect also occurs: normalization of the kidneys, liver, and lungs affects neural connections. Therefore, when stabilizing the brain, it is necessary to take into account the overall picture of the body’s development and look for options for complex treatment.
Osteotherapy is one of the branches of restorative medicine. A person is considered as a single holistic scheme. The basic principles of the technique were proclaimed more than 30 years ago. Over several decades, new approaches have been developed, management methods have been found, and practical experience has been acquired. Medications are used with great caution or are not used at all. Treatment occurs through the mobilization of all elements included in recovery. The advantage of this area of medicine is that drugs are practically not used. The child activates his internal reserves. Complex treatment is the basis of the theory.
The following osteopathic directions have been identified:
craniosacral
structural
visceral
fascial
1. Craniosacral method of treatment.
The craniosacral (cranium-skull, sacrum-sacrum) pathway is based on the theory that the bones of the skull are movable (previously it was believed that only the lower jaw was movable). The dynamics of their movement are imperceptible and strictly obey the impulses of the brain. If the body as a whole and the main control center are functioning normally, then the rhythm of movement of the elements of the skull is clear and correct. Failure of brain impulses against the background of encephalopathy indicates deviations from the norm. The study of the rhythmic movement of children's cranial areas is used not only for diagnosing and identifying nervous destruction, but also for the reverse process. Through the systematization of impulses, it is possible to influence the damaged area. This method is especially effective in eliminating the consequences of encephalopathy.
Treatment of areas of the brain eliminates the symptoms of the disease, normalizes intracranial pressure in children and can lead to restoration of the affected areas.
2. Structural method.
The musculoskeletal system of the newborn was chosen as the object of structural impact.
Bone and cartilage substances influence the function of the spinal cord. Neuronal fibers and veins connected to the spine are also integrated into the overall circuit. Treatment of the limbs, neck, and spine helps to normalize certain damaged areas of the brain affected by pathology (perinatal encephalopathy).
The structural theory in encephalopathy operates on measures affecting the bones and is rarely used to get rid of problems of fetal formation and their influence.
3. Fascial method.
Fascial therapy examines soft tissues, mucous membranes, and bloodstreams. Treatment of encephalopathy is based on the development of neural connections between individual parts of the body. The fascial method eliminates vegetative-visceral disorders of the brain of children and their consequence - hyperexcitability. Treatment of encephalopathy with fascial techniques involves correcting muscle dystonia if there are signs of increased muscle tone.
4. Visceral method for the correction of encephalopathy.
Visceral therapy uses the ability of internal structures to interact and influence each other. Thus, bilirubin encephalopathy requires synchronization of liver function.
Cerebral ischemia syndrome associated with hypoxia manifests itself in abnormal activity of the heart and lungs. Treatment is complex (minimal use of drugs).
Further observation
Patients are discharged from the hospital only after completing a full course of physical therapy and a comprehensive assessment of neuropsychic development. Most often, after discharge, patients do not require specific care, but regular examinations in the clinic are mandatory, especially for children.
If the illness was severe, the child will be observed in a special center, where he will be assisted by a neuropsychological development doctor.
Treatment for seizures depends on central nervous system symptoms and test results. They are prescribed only with a slight deviation from the norm or even within its limits. Phenobarbital is removed gradually, but it is usually taken after discharge for at least 3 months.