Serous meningitis is a lesion of the membranes of the brain, which is characterized by a serous inflammatory process. Serous meningitis in children and adults develops when viruses, bacteria or fungi enter the body. In 80% of clinical cases, serous inflammation of the membranes of the brain and spinal cord is caused by viruses. Viral meningitis affects preschool children, schoolchildren and adults. At the Yusupov Hospital, the nature of meningitis is determined using modern laboratory methods for studying cerebrospinal fluid, blood and other biological materials.
To diagnose changes in the brain, innovative research methods are used using the latest equipment from European and American manufacturers. Doctors take an individual approach to the treatment of each patient suffering from serous meningitis and use modern antiviral and antibacterial drugs registered in the Russian Federation. Neurologists take into account the sensitivity of viruses to the drug and the patient’s body’s response to antimicrobial therapy. Rarely, serous viral meningitis is reported in adults.
Causes
Serous viral meningitis is an infectious disease.
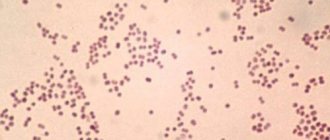
In 75-80% of cases, viral meningitis is caused by enterovirus infection (Coxsackie and ECHO viruses). Less commonly, the cause of serous meningitis is the mumps virus, adenoviruses, Epstein-Barr virus (the causative agent of infectious mononucleosis), cytomegalovirus, herpes and measles viruses. HIV infection can also lead to the development of viral meningitis. Viral meningitis has a seasonal incidence, which depends on the type of pathogen. Most cases of serous meningitis occur in the summer. The mumps virus has a peak incidence in spring and winter. Serous meningitis can be not only viral, but also bacterial (with syphilis, tuberculosis), and sometimes fungal.
Transmission routes
The incubation period for serous viral meningitis is 2-4 days. Depending on the type of pathogen, the following paths take place:
- transmission of serous meningitis pathogens:
- airborne (from coughing, sneezing);
- contact (in the case of direct contact of a child or adult with the skin of a patient or with infected objects);
- water (when swimming in bodies of water contaminated with infectious agents).
The causative agents of serous viral meningitis reach the meninges by hematogenous (through blood vessels), lymphogenous (with lymph flow) or perineural (with cerebrospinal fluid) route. The peak incidence of serous meningitis occurs in the summer. Preschoolers and children of primary school age, as well as persons with immunodeficiency conditions or weakened by other serious illnesses, are most susceptible to the disease.
Symptoms
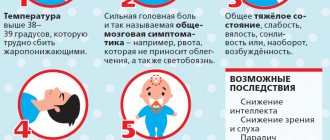
Serous meningitis, as well as inflammation of the meninges of bacterial origin, is characterized by common meningeal symptoms:
- nausea;
- Strong headache;
- temperature increase;
- repeated vomiting.
Distinctive features of serous meningitis of viral origin are the very abrupt onset of the disease.
Consciousness is slightly impaired. When serous meningitis is detected, symptoms in children may be mild. This type of meningitis does not last long and has a favorable outcome. In most cases, there are no complications after serous meningitis. With serous inflammation, cerebral edema develops. The outflow of cerebrospinal fluid is disrupted. Brain swelling provokes an increase in intracranial pressure. Unlike bacterial purulent meningitis, the serous form of inflammation does not lead to massive exudation of neutrophils and brain cells do not die.
From the second or third day of the disease, serous meningitis manifests itself as a pronounced meningeal syndrome. A mandatory sign of serous viral meningitis is fever. Patients' temperature rises to 40 degrees, then after 3-4 days it decreases and after a while it rises again. 2 waves of high temperature are recorded. With mild viral meningitis, this does not always happen.
A painful headache constantly accompanies a patient suffering from viral meningitis. It starts from the temples, intensifies when moving the eyes, from bright light and harsh noise. This type of headache is difficult to control with painkillers.
Children may experience limb cramps and general irritability increases.
They become whiny and capricious. In newborns, the fontanel swells and a “brain” cry appears. Intoxication causes general weakness, malaise, muscle and joint pain. Patients are concerned about nausea, repeated vomiting, and lack of appetite. Abdominal pain and diarrhea appear. Often children, in addition to meningeal symptoms, show signs of acute respiratory viral infection:
- mucous discharge from the nose;
- a sore throat;
- cough.
Skin sensitivity increases.
Patients react sharply to loud sounds, bright lights, noise, and touch. A patient with meningitis feels much better in a quiet, darkened room. In this case, the child lies on his side in bed, his head is thrown back, his knees are pressed to his stomach, his hands are pressed to his chest. In infants, tension and bulging of the fontanel occurs, Lesage's symptom appears - if the baby is lifted up, holding it under the armpits, he pulls his legs towards his stomach and bends them. With viral serous meningitis, there may be minor disturbances of consciousness (stunning or drowsiness). Sometimes signs of damage to the cranial nerves develop, difficulties with swallowing, double vision, and strabismus appear. Motor activity disorders manifest themselves as partial or complete paralysis.
In patients with serous viral meningitis, the following meningeal signs are determined:
- Kernig's symptom - the inability to straighten a leg bent at a right angle;
- Brudzinski's symptom: lower (when trying to straighten one bent leg, a reflex flexion of the second leg occurs), and upper - when bending the head, involuntary flexion of the lower limb occurs.
- Babinski's symptom - with line irritation of the plantar surface of the foot, dorsal flexion of the first toe is observed.
The duration of serous meningitis is on average 10 days.
Make an appointment
Purulent meningitis: symptoms
The duration of the incubation period for primary purulent meningitis is, on average, from two to five days. The disease has an abrupt onset. Patients experience increased body temperature, which can reach 40°C, intense and worsening headache, severe chills, nausea and repeated vomiting. The appearance of delirium, psychomotor agitation, confusion, and convulsive syndrome may occur.
Purulent meningitis in adults and children is accompanied by specific symptoms (Brudzinsky, Kernig, Guillain, stiff neck), which occur at an early stage of the disease and intensify after 2-3 days. Patients exhibit severe hyperesthesia and decreased abdominal reflexes, while deep reflexes are increased. In some cases, a diffuse hemorrhagic rash appears.
With purulent meningitis, patients experience double vision, strabismus, drooping of the upper eyelid, and anisocoria, which is associated with damage to the oculomotor nerves.
In more rare cases, there is damage to the trigeminal nerve, the development of neuritis of the facial nerve, dysfunction of the vestibulocochlear (progressive development of hearing loss) and optic nerve (decreased visual acuity, loss of visual fields).
If the inflammatory process spreads to brain tissue, patients develop meningoencephalitis.
Diagnostics
The diagnosis of serous viral meningitis can be confirmed or excluded only based on the results of a cerebrospinal fluid examination.
CSF is obtained using lumbar puncture. It is performed at the slightest suspicion of viral meningitis. Contraindications for spinal puncture for serous viral meningitis are:
- infectious-toxic shock.
- signs of brain herniation (a combination of arterial hypertension and bradycardia, increasing focal symptoms, depression of consciousness, impaired pupillary reactions);
- infectious lesions of the skin and soft tissues in the area of the spinal puncture;
- convulsive status.
Cerebrospinal fluid in serous viral meningitis is always clear and colorless.
Its pressure reaches 300 - 400 mm. water Art. In the cerebrospinal fluid, a moderate increase in the number of lymphocytes is determined (from 30 to 800 cells in 1 μl). In the first days of the disease, neutrophils can be detected in the cerebrospinal fluid, and from the second or third day lymphocytes appear. The protein content may be normal or reduced, the level of sugar and chlorides does not change. By slowly releasing 3-6 ml of cerebrospinal fluid during the first puncture, intracranial pressure decreases, so patients experience less headaches and significantly improve well-being. In the peripheral blood there is a reduced number of leukocytes, a slight increase in the content of neutrophils without a significant shift in the leukocyte formula to the left, and a moderate increase in the erythrocyte sedimentation rate. By the beginning of the second week of the disease, the number of eosinophils in the peripheral blood increases.
Expert opinion
Andrey Igorevich Volkov Neurologist, Candidate of Medical Sciences
The viral nature of inflammation of the meninges accounts for 80% of cases. Serous meningitis is most often caused by enteroviruses. The disease is most common in children, but in some cases, viral meningitis also affects adults. The symptoms of serous pathology have no distinctive features compared to other forms.Without prescribing etiotropic therapy, in more than half of cases, meningitis ends in death. The infectious disease quickly becomes severe and complicated. In 10% of cases, death occurs within 1–2 days, even with treatment started.
At the Yusupov Hospital, neurologists use their entire diagnostic arsenal to identify infectious diseases. The main method for detecting viral meningitis in adults is cerebrospinal fluid analysis. With its help, the pathogen is determined. CT and MRI are highly informative. Their results make it possible to determine the localization of the pathological focus in the brain. Based on the data obtained, etiotropic therapy is selected. Depending on the accompanying symptoms, symptomatic treatment is selected.
Acute serous meningitis
Common causative agents of serous meningitis include enterovirus, mumps virus, lymphocytic choriomeningitis virus, herpes simplex virus type 2, Epstein-Barr virus, tick-borne encephalitis virus. Serous meningitis is characterized by lymphocytic pleocytosis, a moderate increase in protein and normal glucose content in the cerebrospinal fluid, a negative result of bacteriological examination, and a benign course with spontaneous recovery.
Clinically, serous meningitis is manifested by fever, headache, pain when moving the eyeballs, meningeal symptoms (usually stiff neck muscles, less often Kernig and Brudzinski symptoms), photophobia, anorexia, nausea and vomiting, myalgia, and sometimes abdominal pain and diarrhea. Acute uncomplicated viral meningitis is usually not characterized by deep depression of consciousness, persistent symptoms lasting more than 10 days, epileptic seizures, damage to the cranial nerves and other focal neurological symptoms, i.e. signs of damage to brain tissue.
When diagnosing viral meningitis, first of all, one should exclude such pathologies as purulent meningitis (especially untreated), tuberculous, fungal, mycoplasma, parasitic and parameningeal infections, neurosyphilis, leptospirosis, meningeal carcinomatosis, meningitis in non-infectious diseases (sarcoidosis, systemic lupus erythematosus), medicinal meningitis. This is often helped by examining the cerebrospinal fluid. For example, low glucose levels are more common in tuberculosis, fungal and listeria meningitis, neurosarcoidosis or meningeal carcinomatosis and are only rarely found in meningitis caused by mumps virus and lymphocytic choreomeningitis. All patients must undergo a multifaceted blood test (platelet count, liver tests, levels of urea, lipase, amylase, etc.), bacteriological tests of blood, cerebrospinal fluid, urine, feces, nasopharyngeal swabs, serological tests for syphilis and HIV infection, R-graph of the chest. For reliable diagnosis, virological and serological studies are carried out, especially polymerase chain reaction. Retrospectively, the virus can be identified by an increase in the titer of specific antibodies in the serum and cerebrospinal fluid.
Treatment of viral meningitis is symptomatic: bed rest, analgesics, antiemetics (for example, Motilium), detoxification, and sometimes tranquilizers (Seduxen). Corticosteroids are not indicated. Monitoring the sodium content in the blood is necessary - due to the threat of disruption of the release of antidiuretic hormone during hyponatremia. A repeat lumbar puncture is indicated if fever, meningeal symptoms, and headaches do not improve within a few days. If bacterial meningitis cannot be excluded, empirical antibiotic therapy is prescribed. For severe meningitis caused by herpes simplex and herpes zoster viruses, as well as the Epstein-Barr virus, acyclovir can be used.
Forecast. In adults, full recovery often occurs. Some young children may have mental developmental disorders, hearing loss and other disorders. Seizures usually do not occur. Next, we will briefly present information about various viral meningitis.
1) Meningitis caused by the Coxsackie and ECHO viruses (the abbreviation ECHO means: an orphan virus that affects the cells of the human small intestine). Mostly children (under 15 years of age) are affected, more often in the summer-autumn period. The method of infection is fecal-oral. The incubation period is from 2 to 7 days. More than 40 strains are definitely pathogenic. They can cause a number of diseases, including myalgias, spinal cord lesions (similar in clinical manifestations to polio), encephalitis, and some autoimmune complications. Enteroviral diseases often occur in the form of epidemic outbreaks.
Serous meningitis begins acutely, with a sharp rise in temperature, headache, and repeated vomiting. The temperature lasts for about a week. The appearance of patients is typical: the face is hyperemic, the nasolabial triangle is pale. Often there is conjunctivitis, injection of scleral vessels, often pharyngitis, herpetic rashes on the lips and in the nose, herpetic sore throat, maculopapular, vesicular or petechial rash, pleurodynia, myopericarditis. In the blood of many patients, a shift in the leukocyte formula to the left and an increase in ESR to 25–40 mm/h are noted.
Meningeal symptoms appear on the 2nd–3rd day of illness. Lymphocytic pleocytosis (in the first hours it may be neutrophilic), increased protein levels, and normal glucose levels are found in the cerebrospinal fluid. The virus can be isolated from feces, less often from cerebrospinal fluid, nasopharynx. The titer of antiviral antibodies in serum and blood increases when studying paired samples.
The course of enteroviral meningitis is favorable and ends with recovery. Within 2 weeks - 1 month, however, there may be relapses (10–40% of cases): deterioration of the general condition, rise in temperature, increased headache, and sometimes vomiting. Inflammatory changes in the cerebrospinal fluid are again detected.
2) Meningitis caused by the mumps virus . Mostly children of preschool and school age are affected; boys are 3 times more likely than girls. Infection, hypothetically, occurs through airborne droplets. Most often they get sick in late autumn or early spring. The incubation period lasts about 3 weeks. Within 10 days after the onset of mumps symptoms, the patient is a source of infection.
Inflammation and swelling of the salivary glands are most often accompanied by meningeal symptoms on the 3rd–5th day (this can happen a month later, or earlier - before the glands become swollen). Mumps meningitis sometimes develops without clinical manifestations of mumps. It is believed that the early forms of mumps meningitis occur during the introduction of the virus from the blood into the central nervous system; the later forms are based on a neuroallergic process. From the blood, the virus can spread to other organs, causing, for example, pancreatitis or orchitis.
Mumps meningitis develops acutely with a rise in body temperature to 39–40°C, severe headache, and repeated vomiting. Meningeal symptoms are moderate. There may be meningism without meningitis, asymptomatic meningitis. Young children develop general weakness, drowsiness, adynamia, less often - agitation, delirium, hallucinations, rarely - confusion and depression of consciousness, generalized epileptic seizures.
In the diagnosis of the disease, a prominent place belongs to the study of cerebrospinal fluid. Pleocytosis (hundreds, sometimes thousands of cells) is detected in the cerebrospinal fluid; in the first days of the disease, lymphocytes predominate, there may also be neutrophils, and subsequently - exclusively lymphocytes. The amount of protein is slightly increased, sometimes normal, glucose is not changed, in 10% of patients it is moderately reduced. During recovery, the cerebrospinal fluid is sanitized within 2 weeks, less often - over a longer period. Clinical symptoms disappear on the 7th–10th day. In 1–5% of cases, signs of brain tissue damage are detected. Complications include pancreatitis (15%) and especially orchitis (in boys over 10 years of age). Pancreatitis is characterized by pain most often in the upper left quadrant of the abdomen, radiating to the back, and repeated vomiting; orchitis - pain and swelling of one of the testicles, hyperemia and swelling of the scrotum, increased body temperature. By the 10th–12th day, these symptoms disappear, but in some cases, orchitis leads to infertility.
The nature of meningitis can be determined most quickly by the fluorescent antibody method; more time is required for the hemagglutination inhibition reaction. Treatment is symptomatic; for orchitis, local treatment is prescribed; for pancreatitis, traditional treatment regimens are used.
3) Acute lymphocytic choriomeningitis . A rare neuroinfection, its reservoir is gray house mice. Infection occurs through the oral route. Mostly people aged 20–35 years are affected. The course of the disease is benign. The etiology of meningitis is determined by isolating the virus from the blood and cerebrospinal fluid, the neutralization reaction and complement fixation, and in urgent cases - by the method of fluorescent antibodies.
4) Meningitis due to herpetic infection . The causative agent is herpes simplex virus type 2 (HSV-2), as well as varicella zoster and herpes zoster viruses. HSV-2 is the causative agent of genital herpes. Aseptic meningitis occurs in 16% of cases against the background of vesicular rashes in the genital area, as well as complaints of difficult and painful urination, radicular pain in the lower back, paresthesia and anesthesia in the anogenital area. Lymphocytic pleocytosis is detected in the cerebrospinal fluid.
Meningitis caused by the herpes zoster virus is manifested by a body temperature of up to 38–39°C and relatively mild meningeal symptoms. Confusion, depression of consciousness and cerebrospinal fluid syndrome occur extremely rarely; meningitis is often asymptomatic. Treatment with acyclovir (5 mg/kg IV drip 3 times a day for 5 days) is indicated.
Complications of herpes zoster include lesions of the eyeballs, postherpetic neuralgia, cranial nerve palsies, myelitis, meningoencephalitis, as well as contralateral hemiparesis associated with ophthalmic herpes. Hemiparesis occurs due to vascular damage (granulomatous angiitis of the meningeal and cerebral arteries, most often the middle cerebral artery and its branches) and cerebral infarction. Infarction of the cerebellum and occipital lobe with ophthalmic herpes and infarction of the brain stem with cervical localization of herpes have been described. Hemiparesis occurs between 1 week and 6 months after the onset of the disease. Half of these patients experience depression and confusion. Rarely, hemiparesis is accompanied by hemianesthesia, hemianopsia, and cerebellar symptoms. The diagnosis of cerebral infarction is verified using CT or MRI.
5) Meningitis in infectious mononucleosis . Caused by the Epstein-Barr virus, it occurs mainly in children and young people and manifests itself in damage to the lymph nodes, liver, spleen and skin. Involvement of the central nervous system with symptoms of meningitis and encephalitis is noted in 1–5% of cases. Crucial in diagnosis is the detection of leukocytosis in the blood with an increase in the number of lymphocytes and the appearance of abnormal mononuclear cells (atypical lymphocytes). Treatment is symptomatic.
6) Meningitis in cat scratch disease . The causative agent is Bartonella henselae. In 60% of cases, people aged 5–21 years are affected. 3–10 days after the scratch, general infectious symptoms appear, and after 2 weeks regional lymphadenopathy appears. Damage to the nervous system is detected 1–6 weeks after the onset of adenopathy and occurs in the form of serous meningitis, encephalitis, radiculopathy, myelopathy, and neuroretinitis. Moderate lymphocytic pleocytosis and increased protein content are detected in the cerebrospinal fluid. In severe cases of the disease, confusion and depression of consciousness, seizures are observed; lesions of the cranial nerves, aphasia, hemiparesis, and ataxia are less common. The acute period lasts 1–2 weeks, over 1–6 months there is a gradual restoration of impaired functions, in 90% it is complete. Cognitive impairment and seizures persist for a long time. Treatment uses erythromycin or doxycycline, sometimes in combination with rifampicin; the effectiveness of antibacterial therapy is considered unproven.
7) Benign recurrent serous meningitis of Mollare .
Etiology – hypothetically, herpes simplex type 2, epidermoid cysts, histoplasmosis. The disease occurs at any age, manifesting itself in spontaneous and short (1-3 days) attacks of nervous and mental disorders for 2-5 years. During an attack, rigidity of the neck muscles, Kernig's and Brudzinski's symptoms are detected. There may be transient neurological symptoms (seizures, diplopia, dysarthria, anisocoria, pathological foot signs, etc.), confusion and depression of consciousness. Fever is moderate, but sometimes reaches 40°C. Lymphocytic pleocytosis is detected in the cerebrospinal fluid (in the early stages of the disease it can be neutrophilic), a slight increase in protein, and normal glucose levels. Mollare's meningitis is differentiated from recurrent bacterial, viral and fungal meningitis and sarcoidosis, echinococcal (hydatid) cyst, intracranial tumors, Behçet and Vogt-Koyanagi-Harada syndromes (in the latter two cases, severe lesions of the skin and eyes are observed). Relapses of Mollaret's meningitis are treated with colchicine, glucocorticoids or non-steroidal anti-inflammatory drugs. The prognosis is favorable. Il progetto Icon che vede l'incontro tra Disaronno e la hogan outlet grande moda italiana arriva al suo quarto anno e lo fa outlet hogan online con una nuova limited edition esclusiva. Dopo aver hogan outlet vestito la sua iconica bottiglia con creazioni hogan outletfirmate da Moschino, Versace e Cavalli, il liquore italiano hogan outlet “Il Paisley, emblema dell'Albero della Vita e shogan outletinuosa palmetta del disegno cachemire da cui fiorisce la tradizionehogan outlet Etro, non rappresenta soltanto la Palma da dattero sac longchamp pas cher che forniva cibo e riparo, ma anche un collegamento sac longchamp pas cher iconografico tra Oriente ed Occidente attraverso golden goose outlet saldi le sue migrazioni culturali, dalle stampe indianegolden goose outlet saldi ai ricami celtici. ” ha detto Veronica Etro. “La nuovapjs pas cher bottiglia Disaronno Limited Edition si veste e sinike tn pas cher colora di paisley, esplorando i valori tradizionali legati all'arte del disegno realizzato a mano, come un tradizione e contemporaneamente della sperimentazione, per pjs pas cher ricercare soluzioni nuove ed originali.”La sac goyard pas cher limited edition Disaronno Wears Etro, acquistabile a partire da ottobre, sostiene la charity Fashion 4 Development, patrocinata dalle Nazioni Unite e piumini moncler outlet a cui anche quest'anno ILLVA Saronno devolverà barbour paris pas cher parte del Ricavato delle vendite, offrendo un barbour paris pas cher contributo tangibile allo sviluppo di numerosi interventi umanitari in Africa. L'evento di presentazione della nuova edizione limitata si è tenuto ieri sera agolden goose outlet saldi Milano presso la boutique Etro in Via Monte golden goose outlet saldi Napoleone, dove Veronica Etro e Augusto golden goose outlet saldi Cara Delevingne has succeeded where many have failed in making the transition from full-time supermodel to professional actress, and now a documentary entitled The Cara Project, will explore just how she has done it. The program, which has been acquired by golden goose outlet saldi Revolver Entertainment, will be released piumini moncler outlet on DVD in the coming months, reports Variety, as well as being offered for sale to broadcasters at Mipcom and AFM next month. Details of the contents are scarce, piumini moncler outlet Delevingne's meteoric rise to fame saw her become piumini moncler outlet the most sought-after catwalk and campaign modelsac longchamp pas cher of her generation, walking for every major sac longchamp pas cher fashion house and amassing over 36 million sac longchamp pas cher Instagram followers in the process. Her hogan outlet filmography – given that her first film of note hogan outlet came out in 2015 – is no less impressive. Shehogan outlet has Paper Towns, Pan, Kids In Love and Suicide Squad already under her belt, and has London Fields, Tulip Feverand
Treatment
Treatment of serous meningitis is aimed at preventing or limiting the formation of irreversible brain damage. Doctors do not use antibacterial drugs in the treatment of serous meningitis of viral origin. Means aimed at destroying infectious agents include:
- recombinant α-interferon (Viferon in suppositories);
- inducers of endogenous interferon (cycloferon, neovir);
- RNase;
- intravenous immunoglobulins (intraglobin f at a dose of 3 ml/kg per day), which are prescribed from the second to the fifth day of the disease or in severe condition of the patient.
In severe cases of the pathological process, glucocorticoids are used: prednisolone or dexazone during the first 2-3 days of the disease.
Antibiotics are prescribed only for the development of bacterial complications of serous viral meningitis. For serous meningitis caused by the herpes virus or Epstein-Barr virus, acyclovir is prescribed. Infants and immunocompromised patients need nonspecific and specific antiviral therapy. They are given intravenous immunoglobulin. To reduce intracranial pressure, diuretics are prescribed - furosemide, Lasix, acetazolamide. For severe cerebral edema, the starting drug is mannitol. In order to reduce the manifestations of intoxication, infusion therapy is carried out. The volume of intravenous fluid administered is 2/3 of the child’s physiological need for water. It must strictly correspond to the amount of fluid removed. A 10% glucose solution, rheopolyglucin, albumin, and plasma are used. Colloidal and crystalloid solutions are administered.
At temperatures above 38 C, antipyretics are used - ibuprofen, paracetamol. Anticonvulsants include seduxen (Relanium), GHB (sodium hydroxybutyrate 20%). For persistent disturbance of consciousness, intractable repeated convulsions, central hyperthermia (increased temperature) and arterial hypertension, sodium thiopental is administered intravenously.
The use of barbiturates requires the patient to be placed on artificial ventilation. It is carried out at the Yusupov Hospital using expert-class ventilators. All patients with serous meningitis are shown early administration of drugs that improve the metabolism of cells of the central nervous system. Neurologists use piracetam, nootropil, picamilon. Nootropics are first administered intravenously and then patients take them orally.
Ascorbic acid and riboxin help reduce brain energy deficiency and improve tissue metabolism during meningitis. In severe cases of the disease, antioxidants (cytochrome, cytomol) are prescribed. Medicines that improve cerebral circulation are prescribed to all patients from the first day of treatment. The drugs of choice are Cavinton (Vinpocetine) and dipyridamole (Curantyl). The most effective is the combined use of vasoactive and neurometabolic drugs (instenon and actovegin).
How does necrosis manifest itself?
If we talk about the first symptoms of necrosis, they are presented in the form of numbness and lack of sensitivity. In such a situation, you must immediately visit an experienced and qualified doctor at a medical center. In addition, the skin becomes pale. This happens because blood circulation is impaired. Over time, the skin will acquire a bluish tint, then turn black or dark green. In the presence of necrosis in the lower extremity, a person notices rapid fatigue while walking, a feeling of coldness, cramps appear, as well as lameness, as a result of which non-healing trophic ulcers will form, which will necrotize over time.
Due to the fact that the respiratory and central nervous systems, kidneys, and liver cease to function normally, blood circulation is disrupted, and a person’s general condition of the entire body deteriorates. In addition, the immune system decreases, as concomitant blood diseases, anemia appear, and metabolic processes are disrupted, the body is depleted, hypovitaminosis and fatigue are observed.
Consequences
Serous meningitis can have various consequences.
When the first symptoms of this disease appear, it is important to seek medical help promptly. The best thing to do is call an ambulance. Treatment of serous meningitis must necessarily take place in a hospital setting. Self-medication is unacceptable. The sooner adequate medical care is provided, the greater the chance that the consequences of the disease will never appear or will be minimal.
In cases where the patient delays treatment for too long, the following complications may occur:
- blindness;
- deafness;
- brain disorders;
- dysfunction of the speech apparatus;
- delay in psychomotor development.
In medical practice, in the advanced stage of serous meningitis, in the absence of treatment, paralysis, coma and death occurred. But this is rather an exception to the rule. In most cases, serous meningitis is not as serious as, for example, tuberculosis.
Even with favorable treatment and prognosis, the patient may experience headaches for a long time. If after a course of therapy pain persists for more than 2 months, you should definitely consult a doctor. If necessary, repeated examination is possible.
Prevention
During outbreaks of serous meningitis, it is not advisable for adolescents and young children to swim in open water.
You should always drink specially purified or boiled water, observe personal hygiene rules, wash your hands thoroughly with soap after using the toilet and before eating. It is also necessary to wash vegetables and fruits before eating, and if possible, pour boiling water over them. It is worth paying attention to any viral disease in children: acute respiratory viral infection, influenza, chickenpox, measles, mumps. The child’s contact with rodents and ticks should be minimized as much as possible, since they are considered carriers of viruses. To prevent measles, mumps, and rubella, infectious disease specialists recommend routine vaccinations for children. Meningitis caused by the influenza virus is prevented by seasonal specific vaccination.
If a viral infection proceeds atypically, the temperature does not decrease when taking therapeutic doses of antipyretic drugs, vomiting occurs, which does not bring relief, call an ambulance and call the Yusupov Hospital. The neurology clinic admits patients with meningeal symptoms 24 hours a day, 7 days a week. Doctors will determine the cause of meningitis and provide adequate treatment for the disease.
Make an appointment
Prevention of serous meningitis
How to protect yourself and your loved ones from infection with serous meningitis?
- Swim only in strictly permitted areas, especially for children. Since open bodies of water can be a source of infection.
- Drink only purified and boiled water
- Wash your hands thoroughly and observe personal hygiene rules.
- Thoroughly wash and pour boiling water over vegetables and fruits.
- Strengthen your body and lead a healthy lifestyle.
- Try to avoid contact with people who have meningitis. Some types of meningitis are spread through respiratory droplets such as kissing, coughing, sneezing, or sharing personal hygiene items such as a toothbrush or towel. If there are people with meningitis in your family, try to isolate them from other family members;
- After close contact with someone with meningitis, be sure to consult a doctor. Depending on the proximity of the exposure and the type of meningitis, you will need to take an antibiotic to prevent the disease;
- Be especially careful when traveling to potentially hazardous areas. Some types of meningitis are carried by animals and insects, so try to stay as far away from them as possible, and remember to use insect repellent.
- the body of both a child and an adult, from possible severe consequences in the form of meningitis.
Follow the schedule of preventive vaccinations, for example, the MMR trivaccine (measles, mumps, rubella). Vaccination helps prevent many diseases that can lead to meningitis. Most often, vaccinations against meningitis are given to children at an early age.