Causes of arachnoiditis
In most patients with arachnoiditis, the predisposing factor is infectious diseases. In particular, these diseases include chickenpox, influenza, measles, viral meningitis, cytomegalovirus infection, and meningoencephalitis. The disease can also be provoked by chronic intoxication of the body, inflammatory diseases of the paranasal sinuses, and trauma. Arachnoiditis is often diagnosed in patients who experience reactive inflammation of a growing tumor.
Pathology can also occur due to acute or chronic purulent otitis media. In this case, inflammation is provoked by toxins and low-virulent microbes. Researchers also include various complications of purulent otitis (petrositis, labyrinthitis, sinus thrombosis), brain abscess, purulent meningitis and otogenic encephalitis as the causes of the disease.
In neurology, there are also a number of factors that are considered predisposing to the occurrence of the disease. Such factors include intoxication (for example, alcohol), frequent viral diseases, chronic overwork, hard work in an unfavorable climate, and frequent injuries. In 10% of all cases of the disease, it is impossible to establish the exact etiology.
Prevention of arachnoiditis
Arachnoiditis, the symptoms and treatments for which are described above, can be prevented. In order to reduce the likelihood of developing the disease to a minimum, the following recommendations must be followed:
- strengthen the immune system, harden the body;
- to refuse from bad habits;
- Healthy food;
- observe the work and rest schedule;
- If possible, avoid getting into stressful situations;
- walk more, move, play sports;
- promptly treat diseases of a traumatic or infectious nature;
- periodically sanitize foci of chronic infection in the body;
- undergo regular preventive examinations with an ophthalmologist and ENT specialist.
Health to you!
Pathogenesis of arachnoiditis
To understand the nature of the disease, it is necessary to become familiar with the anatomical features of the brain. The arachnoid membrane, which is affected by inflammation during arachnoiditis, is located between the soft and dura mater. Moreover, it is not fused with them, but simply fits tightly. Unlike the pia mater, the arachnoid membrane does not penetrate the cerebral convolutions. Small spaces filled with cerebrospinal fluid are formed under it.
All these spaces connect to the fourth ventricle. Through these spaces there is an outflow of cerebrospinal fluid from the cranial cavity. The mechanism of occurrence of arachnoiditis is as follows: due to the influence of various causes and provoking factors, the body activates the production of antibodies to the arachnoid membrane, which then provokes its inflammation. In patients with arachnoiditis, there is clouding and noticeable thickening of the arachnoid membrane, as well as the appearance of cystic expansions and connective tissue adhesions in it.
What is arachnoiditis?
Arachnoiditis is an inflammation of the middle layer (arachnoid) of the meninges, which is the protective covering surrounding the brain, spinal cord, and nerve roots of the cauda equina.
The meninges (the lining of the spinal canal) are connective tissue composed primarily of collagen and elastin. Damage, trauma, tumor or infection can cause inflammation of the arachnoid layer anywhere.
Arachnoiditis has been known since the 19th century, when its main causes were infections, mainly tuberculosis and syphilis. It has now become known that the dissolution and degeneration of the arachnoid layer is caused by genetic and autoimmune disorders.
Classification of arachnoiditis
- Arachnoiditis of the meninges
- Optico-chiasmatic arachnoiditis
- Arachnoiditis of the posterior cranial fossa
- Arachnoiditis of the spinal cord membranes
This type of disease is also called cerebral. Cerebral arachnoiditis is localized in the posterior cranial fossa, on the convex surface of the brain and its base. The clinical picture of this disease is characterized by regular headaches and impaired circulation of the cerebrospinal fluid. In the most severe cases, the disease is accompanied by convulsive seizures, which can even lead to status epilepticus.
Arachnoiditis of the brain is often located in the central gyri and anterior parts of the cerebral hemisphere. Due to the resulting pressure on the sensory and motor centers, the patient may experience sensitivity and movement disorders. If the cerebral cortex is compressed or a cyst forms in it due to arachnoiditis, the patient may experience epileptic seizures.
This type of arachnoiditis is localized mainly in the chiasmal region. Frequent causes of this form of arachnoiditis are tonsillitis, malaria, syphilis, infectious diseases of the paranasal sinuses, and traumatic brain injuries. This type of arachnoiditis is characterized by the formation of adhesions in the area of the intracranial part of the optic nerves and the chiasm. In the most difficult cases, a scar may form around the chiasm.
As a rule, the disease provokes vision problems in the patient. In this case, the degree of decrease in the patient’s vision can vary from its minimal decrease to blindness. In most cases of optochiasmatic arachnoiditis, patients experience optic nerve atrophy. Visual symptoms are often severe, while hypertension symptoms are moderate.
It is the most common type of cerebral arachnoiditis. The severity of the symptoms of the disease depends on the location and nature of the inflammatory process, as well as its combination with hydrocephalus. The formation of cysts and adhesions usually leads to the closure of the openings of the cerebral ventricles, which provokes an increase in intracranial pressure. If intracranial pressure does not increase and is normal, the disease can last a long time.
The acute form of the pathology is characterized by all the symptoms of high intracranial pressure: nausea, dizziness, vomiting, bradycardia, severe headache localized in the back of the head. With a less acute course of the disease, signs of damage to the posterior cranial fossa become most pronounced. Patients may also experience symptoms such as unsteady gait and spontaneous nystagmus.
This is a spinal form of arachnoiditis, which occurs mainly due to purulent abscesses and furunculosis. Symptoms of the disease are similar to those of an extramedullary tumor: patients experience motor and sensory disorders, as well as radicular syndrome (limited mobility, parasthesia, trophic changes, pain in the heart, lower back and stomach, neck and limbs).
Spinal arachnoiditis is localized mainly at the level of the lumbar and thoracic segments, as well as on the posterior surface of the spinal cord. Typically, arachnoiditis of the spinal cord membranes is chronic.
Symptoms of arachnoiditis
The first symptoms of the disease appear long after the exposure of the body to the provoking factor that caused its appearance. During this time, autoimmune processes occur in the patient's body.
The duration of this interval is directly related to which factor affected the body. For example, after a patient has had the flu, the first symptoms of arachnoiditis appear after a long period of time - from three to twelve months. After a traumatic brain injury, this period is reduced to 1-2 hours. At first, the patient is concerned about the symptoms characteristic of asthenia: sleep disturbance, weakness, fatigue, irritability. However, over time, more severe focal and cerebral symptoms of arachnoiditis may appear.
Diagnostics
Diagnosis of arachnoiditis is often difficult due to the late presentation of patients. If a significant period of time has passed since the infection, it is not always possible to establish a connection between the infectious lesion and the symptoms that appear several months later. Diagnostic methods:
- Pneumoencephalography. X-ray examination of brain tissue with a contrast agent in the form of gas - carbon dioxide, oxygen, nitric oxide.
- Echoencephaloscopy. Ultrasound examination aimed at identifying extensive pathological processes in brain tissue.
- Electroencephalography. Method for studying bioelectrical activity of the brain.
- Rheoencephalography. Rheographic method for studying the circulatory system of the brain.
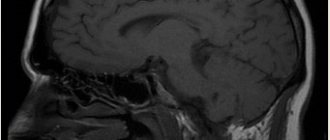
- MRI, CT. Shows the degree of thickening of the meninges and the presence of adhesions.
- Cerebrospinal fluid examination.
Analysis of a lumbar puncture sample shows a slight increase in cerebrospinal fluid pressure and a moderate increase in the concentration of lymphocytes in it. Based on the results of the examination, conservative or surgical treatment of arachnoiditis is carried out.
General cerebral symptoms of arachnoiditis
The cerebral complex of symptoms of cerebral arachnoiditis is characterized by liquor-hypertension syndrome. Most patients complain of a sharp headache, which is most active in the morning and can be aggravated by coughing, physical activity and straining. The consequences of increased intracranial pressure include such disorders as pain when moving the eyes, vomiting, nausea, and a feeling of strong pressure on the eyes.
Many patients turn to a neurologist with complaints such as decreased hearing, tinnitus, and attacks of dizziness. Therefore, during diagnosis, the doctor should exclude various ear diseases such as labyrinthitis, chronic otitis, cochlear neuritis, adhesive otitis. It is also possible that symptoms characteristic of vegetative-vascular dystonia may appear.
Patients with arachnoiditis occasionally experience liquorodynamic crises - attacks of headache accompanied by vomiting, nausea and dizziness. Rare crises are considered attacks with a frequency of no more than 1-2 times per month, average - 3-4 times, frequent - more than 4 times. Depending on the severity of symptoms during a crisis, its mild, moderate and severe forms are distinguished. The latter can last about two days.
Focal symptoms of arachnoiditis
Focal signs of the disease occur depending on its location. Convexital arachnoiditis is characterized by mild to moderate disturbances in sensitivity and motor skills of the limbs. More than 35% of patients with this form of arachnoiditis experience epileptic seizures. After the attack ends, the patient experiences a neurological deficit for some time.
Basilar arachnoiditis, which is localized in the optic-chiasmatic region, occurs with serious impairments of attention and memory, as well as a decrease in mental abilities. In addition, patients with this form of pathology complain of a significant decrease in visual acuity and other visual disturbances. In rare cases, opticochiasmatic arachnoiditis is accompanied by inflammation of the pituitary gland, which provokes endocrine-metabolic syndrome, the symptoms of which are similar to those of a pituitary adenoma.
Arachnoiditis of the posterior cranial fossa is characterized by a very severe course. As a rule, patients show signs of facial neuritis and trigeminal neuralgia. Focal manifestations of arachnoiditis also include various cerebellar disorders: cerebellar ataxia, loss of coordination, nystagmus.
Clinic of cerebral arachnoiditis
The disease develops acutely and quickly becomes chronic. Symptoms characterizing arachnoiditis can be divided into general cerebral and focal:
General cerebral symptoms are common to many neurological diseases
These include dizziness, general weakness, sleep disturbances, irritability, distracted attention and memory impairment. The main general cerebral symptom that is observed with inflammation of the arachnoid membrane is headache of varying severity.
Particularly severe headache attacks occur in the morning and may be accompanied by nausea and vomiting. Focal symptoms appear depending on the area of brain damage. With the convexital type, symptoms of cortical irritation and loss of some motor functions predominate. The leading manifestation is considered to be generalized and Jacksonian epileptic seizures. The development of pathology in the area of the base of the skull disrupts the functions of the nerves passing in this area. Decreased visual acuity and other disturbances in visual function indicate an inflammatory process in the area of the optic chiasm. A lesion near the cerebral peduncles manifests itself as symptoms of a disorder of the pyramidal system and oculomotor nerves.
Arachnoiditis near the cerebellopontine angle, in addition to headaches in the occipital region, is manifested by tinnitus, dizziness and, in rare cases, vomiting. When walking, the patient staggers, and the body tilts towards the affected side. The gait becomes ataxic in nature, dilatation of the veins of the fundus and horizontal nystagmus develop, in some cases pyramidal symptoms begin. Symptoms of damage to the trigeminal, abducens, facial and auditory nerves are common.
The development of arachnoiditis of the occipital cistern is an acutely developing process. The clinical picture includes fever, pain in the back of the head and neck, increased tendon reflexes, meningeal and pyramidal symptoms.
Diagnosis of arachnoiditis
Diagnosis of arachnoiditis involves a comprehensive assessment by a neurologist of the characteristics of the course of the disease and its clinical signs. One of the important stages of diagnosis is the collection of anamnesis, during which the neurologist pays attention to the nature and development of neurological symptoms, recent traumatic brain injuries of the patient and infections he has suffered. A study of the neurological status is also carried out, which makes it possible to detect mnestic and psycho-emotional disorders, as well as neurological deficits.
Since arachnoiditis is characterized by visual and auditory disturbances, a neurologist may need to consult an ophthalmologist and otolaryngologist for differential diagnosis. An otolaryngologist checks the degree and type of hearing loss using threshold audiometry. The degree of damage to the auditory analyzer can be determined using the study of auditory evoked potentials, electrocochleography and acoustic impedancemetry.
Instrumental techniques such as skull radiography, electroencephalography and echo-encephalography are not considered sufficiently effective in diagnosing arachnoiditis, since they provide limited information about the presence of the disease in the patient. However, with their help you can detect some symptoms of pathology. For example, cranial radiography detects symptoms of prolonged intracranial hypertension, echo-encephalography detects hydrocephalus, and electroencephalography detects epileptic activity.
More information about the disease can be collected using MRI and CT scans of the brain. Both of these studies are used to identify morphological changes in the brain (atrophic changes, the presence of adhesions and cysts) and the nature of hydrocephalus. These techniques are also used to exclude tumors, hematomas and brain abscess. The doctor obtains accurate information about intracranial pressure by performing a lumbar puncture.
Methods for diagnosing the disease
To make a correct diagnosis, the following measures are necessary:
- thorough questioning of the patient to identify the fact of previous infectious diseases, injuries, operations using spinal anesthesia;
- neurological examination to identify disorders of sensitivity, motor function, visual impairment, hearing, and vestibular apparatus;
- X-ray examination of the skull bones is carried out to identify changes characteristic of traumatic brain injury, as well as expansion of the cerebrospinal fluid cavities of the brain (ventricles);
- Ultrasound examination of the brain allows one to establish the fact of increased intracranial pressure;
- computer (magnetic resonance) imaging is performed to assess the degree of cystic lesions of the arachnoid membrane, the substance of the brain, determine the size of the cavities (ventricles), and also to exclude a tumor;
- electroencephalography (EEG) – registration and interpretation of electrical signals from the brain, carried out to identify signs of epilepsy;
- an examination by an ophthalmologist is necessary to assess visual acuity, visual fields, and the fundus picture;
- an examination by an ENT doctor is carried out to determine hearing acuity, the function of the vestibular apparatus, to exclude an infectious process in the outer, middle, inner ear, and paranasal cavities;
- examination by a psychiatrist is necessary to identify disturbances in thought processes, symptoms of personality changes;
Differential diagnosis is carried out with the following diseases:
- tumor of the central nervous system;
- multiple sclerosis;
- optic neuritis;
- neurosarcoidosis;
- idiopathic epilepsy;
- neurosis and neurasthenia;
Treatment of arachnoiditis
The main goal of drug treatment for arachnoiditis is to eliminate the source of infection using antibiotics. The use of antihistamines and desensitizing medications (diazolin, histaglobulin, diphenhydramine, suprastin, pipolfen, tavegil, calcium chloride) is indicated. Drug therapy also involves improving metabolism and local circulation, as well as normalizing intracranial pressure.
Patients who experience increased intracranial pressure are advised to take diuretics and decongestants (furosemide, mannitol, glycerin, diacarb). To eliminate convulsive syndrome, antiepileptic medications (carbamazepine, finlepsin, keppra) are used. According to indications, the doctor may prescribe drugs from the following drug groups:
- absorbable (rumalon, lidase, pyrogenal);
- antiallergic (loratadine, tavegil, diazolin);
- neuroprotectors and metabolites (mildronate, nootropil, ginkgo biloba);
- psychotropics (tranquilizers, antidepressants, sedatives).
Surgical intervention
If drug treatment does not produce the desired results, the patient experiences occlusive hydrocephalus or progressive vision loss, the doctor decides on surgical intervention. During the operation, adhesions are separated and cysts are removed. To reduce the manifestations of hydrocephalus, shunt operations are prescribed.
The prognosis for the patient is often favorable. Only arachnoiditis of the posterior cranial fossa, which is almost always accompanied by occlusive hydrocephalus, can pose a great danger. With frequent relapses of the disease, epileptic seizures and its optico-chiasmatic form, the labor prognosis for the patient may worsen.
Prognosis for arachnoiditis
In most cases, patients with arachnoiditis receive the third disability group. However, if they have severe visual impairment and frequent epileptic seizures, they may be assigned a second disability group. The first disability group includes patients with opticochiasmatic arachnoiditis, which caused complete blindness. Work in transport, at heights, near fire, in noisy rooms, in unfavorable climatic conditions, and with toxic substances is contraindicated for patients with arachnoiditis.