Tetanus - symptoms and treatment
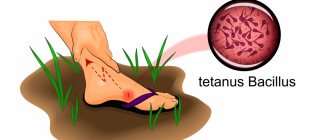
Tetanus , or lockjaw (Greek tetanus - stupor, convulsion) is an acute infectious non-contagious disease caused by the tetanus bacillus (Clostridium tetani). Using a contact transmission mechanism, the bacterium enters the body and releases a toxin that affects the nervous system, leading to hypertonicity of striated muscles and generalized convulsions. It is a preventable disease.
Etiology
Taxonomy:
- domain - bacteria;
- type - Firmicutes;
- class - Clostridia;
- order - Clostridiales;
- family - Clostridiaceae;
- genus - clostridia;
- species - tetanus bacillus (Clostridium tetani).
The disease was first described by Hippocrates, who also gave it its name, although tetanus is also mentioned in the Bible. In the pre-vaccination era, the disease was called “Scourge of War” due to its frequent occurrence in the wounded. The causative agent of the disease was identified in 1883 by the Russian scientist N.D. Monastyrsky. The first morphological description of the bacterium was given by the German physician A. Nikolaier in 1884. In 1890, the Danish physician K. Faber identified tetanus toxin. In 1890, bacteriologists Sh. Kitazato and E. Bering invented anti-tetanus serum. In 1923, the French veterinarian G. Ramon obtained tetanus toxoid, which is used to prevent the disease (formalin is added to the tetanus toxin and kept at high temperature).
Cultural properties. The bacterium is an obligate anaerobe (that is, it lives only in an environment without oxygen). Has fibrinolytic activity (the ability to dissolve blood clots). Releases a toxin during the life of the bacterium (i.e. it is an exotoxin).
Morphological properties . Tetanus bacillus has two morphological forms: vegetative and spore. Does not have capsules. A vegetative cell looks like a stick with rounded ends measuring 4-8 x 0.3-0.8 microns, it is mobile, has up to 20 flagella, Gram stains positive (Gram-positive), and secretes a toxin.
The spore form resembles a drumstick in appearance and is formed under unfavorable environmental conditions (in the presence of oxygen at a temperature not lower than 4 °C). At favorable temperatures, high humidity and the absence of oxygen, spores germinate in the soil with the formation of vegetative cells, and this happens repeatedly, resulting in the accumulation of the pathogen in the external environment.
A vegetative cell grows at temperatures from 14 to 45 °C. In the laboratory, liquid nutrient media are used for cultivation, for example, Kitt-Tarozzi medium or solid nutrient media with the addition of blood (forming a hemolysis zone).
The sensitivity to the negative effects of vegetative and spore forms is different: vegetative cells are low-resistant, spore cells, on the contrary, have very high resistance: they can remain viable when heated to 80 ° C for 4-6 hours, to 90 ° C for 2 hours, when boiled die within 40-50 minutes. Complete decontamination of tetanus spores can be achieved by autoclaving (sterilization with flowing steam) at 130 °C for 20 minutes. When dried, the spores can withstand heating up to 115 °C for 20 minutes. They live in the ground for more than 10 years (this is why contamination of wounds with any soil is dangerous if the person has not been vaccinated); in sea water they can live up to six months. In a 5% phenol solution, spores remain viable for 24 hours, in 1% sublimate - 10-12 hours, in a 10% bleach solution - for 10 minutes.
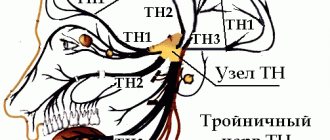
Tetanus toxin is a protein with a high content of amino acids: aspartic acid, isoleucine and lysine. Consists of two fractions: tetanospasmin and tetanohemolysin:
- Tetanospasmin (neurotoxin, protein weighing 150 kDa) causes the main symptom complex of the disease - muscle spasms;
- tetanohemolysin (cardiotoxin) dissolves red blood cells, destroys tissue around the wound, and causes dysfunction of the autonomic nervous system.
A dose equal to 2 ng/kg body weight is considered lethal for humans. It is destroyed at 65 °C, sunlight for 5 minutes, enzymes of the gastrointestinal tract easily break it down [2][5][10][11]. The toxin is not absorbed through the intestinal mucosa, so if swallowed it is not dangerous.
Epidemiology
The pathogen is widespread, but is more common in hot and humid regions. Tetanus bacillus can be found in soil, street dust, gardens (including vegetables), orchards, meadows, and on objects contaminated with soil and feces (wire, nails, etc.). Normally, the bacterium lives in the intestines of herbivores, and can even be detected in the human intestines (up to 40% of cases), without causing any harm to him. From animal and human feces, tetanus enters the soil, where it accumulates (mainly in the form of spores).
WHO estimates that approximately 34,000 newborns died from tetanus in 2015 [12]. This is a 96% decrease from 1988, when 787,000 newborns died from tetanus in the first month of life. In 2021, the disease claimed the lives of 30,848 newborns [13]. There are no reliable data on adults; according to some estimates [14][15], about 300,000 people die annually in the world (mainly in the Asian, African and Latin American regions).
The incidence in the Russian Federation over the past 20 years has averaged 40 people annually [16].
The mechanism of infection of tetanus is contact, through any wound surface. The entrance gates are damaged skin and mucous membranes: abrasions, wounds (including surgical wounds), splinters, burns, frostbite, etc. In deep wounds, in the absence of oxygen, spores turn into vegetative cells producing tetanus toxin, and this is much more common than with superficial wounds.
In developed countries, among unvaccinated people who do not seek medical help, up to 98% of cases of infection occur through microtrauma, mainly of the lower extremities. In case of injuries, childbirth, criminal abortions, puncture of the leg with a nail, etc., infections are less common; in such cases, people, as a rule, immediately seek medical help.
In countries with a low level of medical development, on the contrary, morbidity as a result of more serious injuries predominates, since the majority do not go to medical institutions. It is important to note that almost 100% of cases occur in people who have not been vaccinated and have not sought medical attention.
Factors predisposing to the occurrence of the disease:
- warm climate;
- regions with developed livestock farming;
- “bare foot disease” - injuries (especially with crushing tissue) and microtraumas of the feet: scratches, splinters, abrasions with soil contamination);
- poor sanitary and hygienic conditions;
- inaccessibility of medical care, insufficient treatment of wounds;
- refusal to vaccinate, ignoring revaccination deadlines;
- insect bites that damage the integrity of the skin (for example, bites of large beetles, etc.);
- chronic ulcers and skin lesions;
- intravenous drug administration;
- severe immunodeficiency.
The seasonality of the disease is highly pronounced: in temperate and cold climates - from late April to October; in hot countries where there is no real winter, the incidence is year-round. People most often get sick are males, agricultural and livestock workers, and summer residents. In countries with developed medicine, adults are most often affected. In lagging countries, newborn morbidity may prevail: if births are performed by people with dirty hands and on dirty surfaces, if unsterile instruments and materials are used when cutting and processing the umbilical cord; if pregnant women do not receive the normal course of immunization against tetanus.
A patient with tetanus is not dangerous to others, i.e. it cannot be infected from a person. A person who has recovered from the disease does not develop natural immunity (it is either very weak or absent).
The mortality rate for tetanus reaches 40% (even with timely treatment); tetanus is especially dangerous for people over 65 years of age [1][4][8][11].
Symptoms of tetanus in humans and photos
There are 4 periods during the disease:
- Incubation.
- Start.
- The height of
- Recovery.
In the photo the man has tetanus
On average, the incubation period lasts about 2 weeks. The start time for this classification is 2 days. During this period, the main symptoms of tetanus are: pain at the site of penetration of clostridia. The wound in this place, as a rule, has already healed. Then trismus appears - a spasm of the masticatory muscles. The jaws are clenched convulsively, so that not all patients can open their mouths.
During the height of the disease, symptoms of skeletal muscle irritation appear. Muscle hypertonicity is accompanied by severe pain. Extensor reflexes predominate, which is manifested by stiffness of the neck muscles, throwing the head back, hyperextension of the spine (opisthonus), and straightening of the limbs. Hypertonicity of the muscles involved in breathing leads to hypoxia.
Symptoms of tetanus in humans:
- spasm of the masticatory muscles (difficulty opening the mouth);
- spasms of the facial muscles (a “sardonic” smile appears, the lips are stretched, their corners are lowered, the forehead is wrinkled);
- Due to spasm of the pharyngeal muscles, swallowing is impaired;
- convulsions that cover all the muscles of the body in a downward direction (a person arches, standing on his heels and the back of his head - opisthotonus). Painful cramps occur even with minor irritation;
- seizures occur in response to any irritating factor (light, sound, noise).
At an early stage, tetanus has symptoms similar to many diseases, for example, gingivitis and inflammation of the mandibular joints. Indeed, during the development of tetanus bacillus in the body, the masticatory muscles are in constant tension and sometimes twitch. Gradually, the infection begins to resemble epilepsy and a severe hysterical attack.
The action of the pathogen, as we have already noted, occurs extremely quickly; moreover, the first symptoms of tetanus in humans are observed within a few hours from the moment it enters the body.
The waste products of infection are not absorbed through the mucous membrane, which determines their absolute safety when swallowed; in addition, exposure to ultraviolet radiation and heating leads to a very rapid death of pathogens.
It is worth noting that the most dangerous period of tetanus is considered to be from the 10th to the 14th day of the disease. It is at this time that the patient experiences rapid metabolism, metabolic acidosis and increased sweating. A cough begins and it is sometimes very difficult for the patient to clear his throat. In addition to all this, convulsive attacks may occur during coughing and swallowing.
Diagnosis of tetanus
The presence of a contaminated wound and three typical symptoms in the clinical picture confirm the presence of tetanus. An important diagnostic element at an early stage is the collection of anamnesis, which allows one to determine the nature and time of injury, obtain data on the presence of vaccination, signs of infection, and begin treatment in a timely manner.
Laboratory tests are of secondary importance in making a diagnosis. At the initial stage, no changes occur in the cerebrospinal fluid, the toxin is not detected in the blood, and the presence of antitoxic antibodies indicates that the patient has a history of vaccination against tetanus.
In addition, this diagnostic method is rarely used due to the length of wait for results. , histological studies of damaged tissues, microscopy of smears are still .
When making a diagnosis in the early stages, it is very important to differentiate tetanus from gingivitis, periostitis, inflammation of the mandibular joints . At later stages, the clinical manifestations of tetanus become more pronounced, but it is worth special attention to separate them from epileptic seizures, strychnine poisoning, meningitis, encephalitis, the consequences of traumatic brain injury, and hysteria in women .
In newborns, the manifestations of tetanus should be distinguished from the consequences of birth trauma and meningitis. When at this age doubts arise when making a diagnosis, they resort to laboratory tests of cerebrospinal fluid puncture. In older children, tetanus should be distinguished from hysteria and rabies.
To correctly determine the disease, you should contact medical institutions, since in most cases a qualified specialist does not have any difficulties diagnosing tetanus.
Treatment of tetanus in humans
Treatment of tetanus should only be carried out in a hospital setting. The main goal is to neutralize and remove the toxin from the body as quickly as possible.
The wound through which the infection occurred is injected with anti-tetanus serum, then it is opened wide and a thorough surgical treatment is carried out. The faster treatment with anti-tetanus serum is carried out, the easier the symptoms of tetanus are tolerated and the fewer consequences the disease has for the body.
Subsequently, preparations containing proteolytic enzymes (Chymotrypsin, Trypsin, etc.) are usually used to heal the wound.
The course of treatment for tetanus includes:
- combating tetanus pathogens in the area of the primary lesion (opening the wound, removing dead skin, sanitation and aeration);
- administration of antitetanus serum; relief of severe cramps;
- maintaining the vital functions of all body systems;
- prevention of complications;
- complete nutrition, rich in vitamins and microelements to strengthen the immune system.
It is desirable that the patient be treated in a separate room, which will eliminate the negative impact of emerging external stimuli on him.
In addition, it is important to have a permanent post for systematic monitoring of the patient’s general condition. If it is not possible to take food on your own, it is administered through the use of a probe.
If a person has had tetanus, he does not develop long-term immunity, and he can become infected with this disease again.