Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
What is glossopharyngeal neuralgia?
If the cranial nerve is affected by a quarter on one side, and paroxysms of pain appear in the tonsils, soft palate, pharynx and ear, then the patient may have neuralgia of the glossopharyngeal nerve. With this pathology, a violation of the taste perception of the posterior third of the tongue, on the affected side, is detected. Hypersalivation and decreased reflex of the palate and pharynx are also noted. To make a diagnosis, an examination by a neurologist or dentist is required. CT and MRI of the brain are indicated as hardware diagnostic methods. In most cases, treatment is conservative, including:
- Anticonvulsants;
- Analgesics;
- Sleeping pills and sedatives;
- Vitamin therapy;
- Physiotherapy;
- General strengthening procedures.
What is neuralgia
Neuralgia is a lesion of peripheral nerves that causes acute pain.
Medical specialists often encounter neuralgia, since this disease is observed in many people seeking medical help. There are several types of the disease, depending on the location and the causes that cause it, and doctors carry out diagnostics in order to identify the causes and nature of the disease and, based on the diagnosis, prescribe appropriate treatment, without which the patient will have attacks of neuralgia again and again. There can be several causes of neuralgia. Primary neuralgia is damage to the nerves directly; secondary neuralgia is a symptom of other diseases, and to eliminate pain it is necessary to detect and treat the original cause - injury, infection, tumor, etc. In addition to these reasons, neuralgia can be caused by hypothermia, exposure to toxins, stress, inflammatory diseases, osteochondrosis, prolonged physical activity and other reasons. Without treatment, the disease progresses to the neuritic stage, at which the patient develops structural changes in the nerve that reduce its sensitivity. The localization of neuralgia can be very different and its symptoms can often be confused with other diseases, which is why if pain occurs it is very important to consult a doctor in a timely manner.
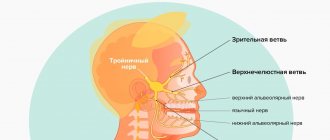
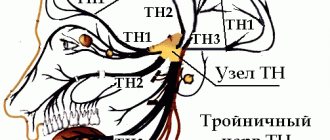
Structure of the glossopharyngeal nerve
N. glossopharyngeus or glossopharyngeus nerve begins in the nuclei of the medulla oblongata. It is based on motor, sensory and autonomic parasympathetic fibers. Moreover, the sensory fibers begin in the sensory nucleus common to the vagus and glossopharyngeal nerves. They innervate the mucous membrane of the pharynx, soft palate, tongue, tonsils, and Eustachian tube. The sensation of taste in the anterior two-thirds of the tongue is provided by taste fibers emerging from the nucleus of the tractus solitarius. The taste fibers of the glossopharyngeal nerve are responsible for the taste sensations of the posterior third of the tongue and epiglottis.
The motor fibers originate in the nucleus ambiguus and innervate the stylopharyngeal muscle, which is necessary for raising the pharynx. Together with the vagus nerve, they form the reflex arcs of the pharyngeal and palatal reflexes.
Parasympathetic fibers originate in the salivary nucleus. Being part of the tympanic and lesser petrosal nuclei, they reach the autonomic ganglion, and with the branch of the trigeminal nerve they regulate salivation of the parotid gland.
Since the pathways and nuclei of the glossopharyngeal and vagus nerves are common, isolated pathology n. Glossopharyngeus. But more often symptoms of combined lesions are observed.
Pathogenesis
There are cases of idiopathic Sicard syndrome. At the same time, it is almost impossible to establish the etiology of the disease. Provoking factors may be:
- Acute or chronic intoxication;
- Otitis;
- Pharyngitis;
- Tonsillitis;
- Sinusitis;
- Atherosclerosis;
- Viral infections incl. flu.
Secondary neuralgia occurs due to:
- Arachnoiditis, encephalitis and other infectious lesions of the posterior cranial fossa.
- TBI.
- Hyperthyroidism.
- Diabetes mellitus.
- Meningiomas, gliomas, medulloblastomas and other intracerebral tumors of the cerebellopontine ganglion.
- Compression and irritation of any part of the glossopharyngeal nerve.
- Nasopharyngeal tumors.
- Intracerebral hematomas;
- Carotid artery aneurysm;
- Hypertrophy of the styloid process.
- Overgrowth of osteophytes of the jugular foramen.
- Ossification of the styloid ligament.
In some cases, pathology may be the first symptom of cancer of the larynx or pharynx.
Causes
Isolated pathology of the glossopharyngeal nerve is less common than the phenomena of bulbar and pseudobulbar palsy (damage to the nuclei of the IX, X and XII cranial nerves). Neuralgia of the glossopharyngeal nerve can be primary or secondary.
Primary neuralgia is caused by the following factors:
- infectious processes of the pharynx (pharyngitis), ear (otitis), pharyngeal tonsils (tonsillitis), oral cavity (stomatitis);
- nerve damage by viruses, including influenza;
- acute or chronic intoxication;
- lack of oxygen (hypoxia) due to atherosclerotic changes in blood vessels.
Secondary neuralgia occurs when the nucleus of the glossopharyngeal nerve, located in the posterior cranial fossa, is damaged. Inflammation of nervous tissue is provoked by the following diseases and pathological conditions:
- arachnoiditis (inflammation of the choroid);
- encephalitis (inflammation of the brain), including after a tick bite;
- mechanical damage due to traumatic brain injury;
- metabolic disorders in diabetes mellitus and hyperthyroidism.
Secondary nerve damage is observed in brain tumors, regardless of their malignancy; compression of the glossopharyngeal nerve occurs in any part of the pathway. According to oncologists, neuralgia of the glossopharyngeal nerve may be the first manifestation of cancer of the pharynx or larynx.
Symptomatic picture
Clinical signs include painful paroxysms lasting from a few seconds to three minutes. A sharp acute pain originates at the root of the tongue and instantly spreads to the tonsils, soft palate, ear and pharynx. May radiate to the eye, neck and lower jaw. Pain can be triggered by coughing, chewing food, its temperature, yawning, swallowing and even talking. During paroxysm, dry mouth is noted, immediately after hypersalivation. But dryness is not a mandatory sign of diagnosis, because the secretory insufficiency of the parotid gland can be compensated by the remaining salivary glands.
Paresis of the levator pharyngeal muscle does not cause swallowing disorders. But difficulties in chewing and swallowing associated with impaired proprioceptive sensitivity, which is responsible for the position of the tongue, may be noted by patients.
The disease has a wave-like course, worsening in autumn and winter.
3. Symptoms and diagnosis
The clinical picture of glossopharyngeal neuralgia in most sources is compared with neuralgia of the facial and trigeminal nerves; as a rule, a careful and evidence-based differential diagnosis is necessary.
Neuralgia of the glossopharyngeal nerve is manifested by paroxysmal pain in the area of the tonsils and the root of the tongue, with various irradiations (to the upper palate, ears, eyes, jaws, larynx, etc.).
This kind of paroxysm lasts from several seconds to several minutes and is often accompanied by a feeling of a dry throat, and ends with increased salivation (hypersalivation). During a painful attack, taste sensitivity is distorted (any food seems bitter), and pharyngeal reflexes are weakened.
Glossopharyngeal neuralgia can occur as alternating remissions and exacerbations, but usually progresses over time - painful paroxysms become more frequent, longer and more painful.
The diagnosis is established clinically, through a careful study of symptoms, examination of reflexes, and examination of the anamnesis. Instrumental methods (primarily MRI) are prescribed mainly to exclude or confirm malignant tumors, hyperplasias, vascular aneurysms, etc.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnostic methods
The diagnosis is made by a neurologist, who, if necessary, can involve an otolaryngologist and dentist. During the examination, the doctor determines analgesia, that is, the absence of pain sensitivity at the base of the tongue, upper parts of the pharynx, and tonsils. Taste sensitivity is also studied, for which a taste solution is applied to symmetrical areas of the tongue. The diagnosis is confirmed by isolated unilateral taste disorder in the posterior third of the tongue. Bilateral disruption is typical for diseases of the oral mucosa, such as chronic stomatitis.
The pharyngeal reflex needs to be checked. To do this, touch the back wall of the throat with a paper tube, which provokes a swallowing movement and occasionally a cough. Normally, touching the soft palate should be accompanied by a lifting of the palate and uvula. Sicard syndrome is characterized by the absence of reflexes on one side. But a similar symptomatic picture can occur with damage to the vagus nerve. If the pharynx and pharynx are strewn with herpetic rashes, the doctor can diagnose ganglionitis of the ganglionitis of the glossopharyngeal nerve nodes, which differs in almost identical n. Glossopharyngeus clinical picture.
To establish the root cause of symptomatic neuritis, neuroimaging diagnostics is needed:
- MRI or CT scan of the brain;
- Electroencephalogram;
- Echo-EG;
- Ophthalmoscopy with consultation with an ophthalmologist.
It is necessary to distinguish between neuralgia of the glossopharyngeal nerve and diseases that cause painful paroxysms of the face and head. These include:
- Neuralgia of the ear ganglion;
- Trigeminal neuralgia;
- Oppenheimer's syndrome;
- Glossalgia;
- Ganglionitis of the pterygopalatine ganglion;
- Retropharyngeal abscess;
- Tumors of the pharynx.
Treatment
Trigeminal neuralgia should be treated with anticonvulsants. The most commonly used is carbamazepine (Finlepsin). When starting therapy, you can additionally prescribe non-steroidal anti-inflammatory drugs. It is also necessary to use neuroprotective therapy with B vitamins, PP, and use vasoactive drugs (for example, trental).
In some cases, the attack is stopped by lubricating the “trigger points” (root of the tongue, tonsils, etc.) with a solution of local anesthetic. In many cases, physical therapy is an additional treatment option. In case of long-term ineffective conservative treatment, neuroma, which requires surgical treatment, should be excluded.
Therapy
To treat neuralgia of the glossopharyngeal nerve, conservative therapy is prescribed. The only exception is if the underlying cause is tumors and hypertrophy of the styloid process, leading to compression of the nerve. In these cases, surgery is indicated.
To relieve pain, a 10% solution of cocaine is prescribed, which is applied to the root of the tongue and pharynx. This allows you to eliminate paroxysms for 6-7 hours. If this remedy turns out to be ineffective, a 1-2% novocaine solution is injected into the root of the tongue. Non-narcotic analgesics and anticonvulsants are also prescribed internally. If the pain syndrome is pronounced, it is advisable to prescribe sedatives, hypnotics, antipsychotic medications and antidepressants. AFT, multivitamin complexes and FiBS are used as general strengthening agents.
Among the physiotherapeutic procedures that have proven effectiveness are:
- SMT on the area of the larynx and tonsils;
- Diadynamic therapy;
- Galvanization.
Glossalgia - symptoms and treatment
The complaints that patients make are varied. At the same time, they allow one to make a diagnosis quite accurately. With glossalgia, patients usually complain of a burning sensation, tingling and tingling in the tongue area.
Unpleasant sensations can occur either periodically or be permanent. In some cases, patients compare the unpleasant sensations with sensations like eating spicy food . Because of this, some patients note the impossibility of long conversations , as increased fatigue develops.
A large number of patients complain of excessive dryness in the mouth and a small amount of saliva.
During stressful situations, various kinds of anxiety, as well as severe fatigue, the symptoms of glossalgia progress. The burning sensation and pain intensify, and therefore the psychological state of such patients worsens. They become very irritable and whiny. While eating, patients feel relief, discomfort disappears or becomes less pronounced.
Burning and tingling sensations are most pronounced on the lateral surfaces and on the tip of the tongue ; in rare cases, glossalgia appears on the back and root of the tongue. The pain is diffuse. If there is no treatment, the symptoms of glossalgia may disappear and then appear, but in another area of the tongue. This disease also has a tendency to disappear completely on its own.
There are no visible changes in the mucous membrane of the tongue, as well as in the oral cavity, with glossalgia. In some patients, slight swelling of the tongue due to the enlargement of some papillae, as well as a coating, usually white, sometimes yellow , which occurs due to insufficient saliva secretion. In old age, varicose veins of the tongue , which is manifested by a slight enlargement of the tongue and its cyanosis.
As a rule, the neurological status of such patients is impaired. Signs of depression , apathy and fatigue may be present . In contrast, patients may be overly active, agitated, anxious and very suspicious .
Most of these patients suffer from nosophobia, a phobic anxiety disorder manifested by an irrational fear of developing life-threatening diseases. During the conversation, it becomes clear that in addition to glossalgia, the patient has other neurotic conditions - sleep disturbances, fatigue, stool disorders [4][6][8].