Competition “Bio/Mol/Text”-2020/2021
This work was published in the “Own Work” category of the “Bio/Mol/Text” competition - 2020/2021.
The nomination partner is the Russian Science Foundation.
The general partner of the competition is the annual biotechnology conference BiotechClub, organized by the international innovative biotechnology company BIOCAD.
The sponsor of the competition is SkyGen: a leading distributor of life science products on the Russian market.
Competition sponsor: the largest supplier of equipment, reagents and consumables for biological research and production.
"Book" sponsor of the competition - "Alpina Non-Fiction"
More than 5 million people in the world suffer from various forms of paralysis, the main causes of which are stroke (34%) and spinal cord injury (24%).
Stroke is currently one of the main causes of disability in the population. In Russia, more than 450,000 strokes are registered annually, and 70–80% of stroke survivors become disabled, with approximately 20–30% of them requiring constant outside care.
Over the past 70 years, the number of patients with spinal cord injury has increased 200 times, and in Russia more than 8,000 people suffer such injuries every year. Most often, this leads to the patient’s inability to move independently and provide for their basic needs. As a result of using a wheelchair, physical activity decreases, which provokes the development of a number of diseases: heart disease, osteoporosis, bedsores. Therefore, there is an active search for alternative methods of restoring the ability to move. One of the newest developments in this direction is the neural interface.
Neurointerface (also known as brain-computer interface, BCI) is a system that allows you to transmit brain signals directly to an external device (this can be a wheelchair, exoskeleton, computer, etc.), in fact, control the “power of thought” (Fig. 1) .
In “Biomolecule” you can read in more detail about the history of the development of neurocomputer technologies, as well as about Elon Musk’s modern Neuralink project [1], [2].
Figure 1. BCI operation diagram.
adapted from materials from the Tritriwulansari website
Methods for recording brain signals
The first link in the BCI operation scheme is receiving a signal from the brain. The following methods are used for this:
- electroencephalography (EEG), which records electrical signals from the brain;
- magnetoencephalography (MEG), which records magnetic fields resulting from electrical activity in the brain;
- near-infrared spectrometry (NIRS), which measures the saturation of blood with hemoglobin (the more active a group of neurons, the more it uses oxygen carried by oxyhemoglobin);
- functional magnetic resonance imaging (fMRI), based on measuring blood flow to different areas of the brain (the more active a group of neurons, the greater the blood flow to it).
Nowadays, EEG is most often used in BCIs to obtain information about the electrical activity of the brain, since it has a high temporal resolution (electrodes allow one to read the immediate activity of individual parts of the brain), is relatively cheap, portable and does not pose a risk to users. EEG-based BCIs consist of a set of sensors that detect EEG signals from different areas of the brain. However, the quality of EEG signals is degraded because the signal travels through the scalp, skull, and many other layers, which creates noise.
To reduce noise and improve recording quality, they resort to invasive methods - implanting a set of microelectrodes inside the skull [3]. This implies significant health risks, which is why they are rarely used in experimental practice. There are two invasive approaches to BCI research: electrocorticography (ECoG), in which electrodes are placed on the surface of the cerebral cortex, and intracortical recording of neural activity, in which sensors are implanted into the cortex (Fig. 2). Such solutions are currently used extremely rarely, only in exceptional cases: either when the patient is already undergoing brain surgery, or when this is the only chance to regain the ability to interact with the outside world.
Figure 2. Electrode layout for EEG, ECoG and intracortical microelectrodes.
adapted from [3]
Non-invasive stimulation could harm brain tumors
Santarnecchi et al. / Science, 2019
One session of transcranial electrical stimulation of the brain reduced the intensity of blood circulation in a brain tumor by a third. According to scientists, poor circulation should deprive cancer cells of oxygen and TES thus prevents tumor growth or may even shrink it. The study was published in Science Advances
.
Transcranial electrical stimulation (TES) is a non-invasive method in which a weak direct current, imperceptible to the patient, is applied to the brain. Previously, there had been tests of the effects of electric current on various tumors in humans and mice, and they showed good results: after exposure to electric current, cancerous tumors received less oxygen, and a test on mice even led to partial necrosis of the malignant formation. But all of these experiments used electrodes that were placed directly into the tumor or into the surrounding tissue - that is, invasive methods were used.
Emiliano Santarnecchi from Harvard Medical School and scientists from the University of Siena conducted a similar experiment, but using TES - electrodes were simply placed on the surface of the head. To participate in the experiment, scientists selected 18 volunteers with glioblastoma or brain metastases that appeared from tumors in other parts of the body. In all volunteers, the tumors were not located very deep so that the current could affect them. True, out of the 18 initial patients, only eight were able to undergo electrical stimulation, because the condition of the remaining selected patients quickly deteriorated and they required urgent surgery.
Volunteers were given a weak current of 4 milliamps through their brains for 20 minutes. In this case, the patients were in an MRI, and scientists first scanned their brains before the procedure, and then after. The results showed that in the case of glioblastoma, blood flow through the tumor was reduced by 26 percent, and in patients with metastases - by 45 percent. However, no changes occurred in healthy brain tissue. After the procedure, the subjects reported that their health did not change in any way, only some felt a slight tingling sensation, which occurs after TES.
It is impossible to say exactly why electrical stimulation reduces blood flow in tumors. As the authors of the article write, the current causes electrolysis, which causes the walls of blood vessels to shrink. It is possible that tumor vessels are more susceptible because they have some differences from healthy vessels, such as the absence of smooth muscle in the walls. The network of vessels in tumors is denser than in healthy tissues, so the current probably passes through them better, which explains why EFT works on tumors but not on normal tissues.
Scientists believe that EFT could be used together with chemotherapy to fight cancer more effectively, but further research is needed to prove the effectiveness of the therapy. Another study showed that electrical stimulation increases the permeability of membranes to drugs, so when combined with chemotherapy, the treatment effect should be greater.
In addition to reducing blood flow to tumors, electrical stimulation of the brain has other beneficial effects, such as reducing symptoms of depression.
Maxim Pechorin
Sensorimotor rhythm and motor cortex
As we have already said, the purpose of a BCI is to capture the user's intention by recording their brain activity. When recording brain activity using EEG, we get a graphical representation of a complex oscillatory electrical process, in which we can identify a number of specific rhythms that differ in amplitude and frequency: alpha, beta, delta, mu and others. Now we are interested in the mu rhythm, since it is on its basis that the neural interfaces used in neurorehabilitation of movements work.
The mu rhythm, or sensorimotor rhythm (SMR), has a frequency of 8–13 Hz and is recorded over the motor area of the cerebral cortex, located in the posterior part of the precentral gyrus (Fig. 3). Suppression of the mu rhythm occurs when a person performs a movement or imagines performing a movement—this is called event-related desynchronization (ERD). This occurs because neurons that previously fired synchronously acquire individual firing patterns that are different from each other. In this case, a person can train in imagining movements, and over time, the suppression of the mu rhythm becomes more and more pronounced, which is used when learning to control a BCI.
The motor cortex is characterized by a topical organization. This means that each section of the cortex corresponds to a specific area of the body that it controls. Figure 3 shows Penfield's homunculus, whose body parts are proportional to the brain areas in which they are represented. As can be seen from the figure, the representations of the upper and lower extremities are located far enough from each other, making it possible for the neural interface to separately recognize the movements of the arms and legs.
Figure 3. Somatosensory and motor homunculus.
adapted from materials from the BioNinja website
Note that the representation of the lower extremities in the motor cortex is much smaller than that of the upper extremities. This is easily explained by the presence of fine motor skills of the hands: the brain needs to control many individual muscles of the fingers. The legs, on the other hand, have fewer muscles to control and are larger. In addition, it is clear that the representation of the lower extremities falls into the interhemispheric fissure, which makes it difficult to recognize EEG signals generated by imagining the movements of different groups of leg muscles. Therefore, the use of BCIs for the legs causes certain difficulties, and most of the existing scientific works on neurorehabilitation using BCIs are devoted specifically to the upper extremities, since it is easier to work with their imagination. In the laboratory of movement physiology of the Institute of Physiology named after. I.P. Pavlov RAS, where the author works, conducts research aimed at studying the processes of rehabilitation of the lower extremities, as well as the possibility of using transcutaneous electrical stimulation of the spinal cord (TESCS) and special practices that help increase the efficiency of BCI control [4].
How to Imagine Movement Effectively
The following features of movement imagination are known that increase its effectiveness:
- Kinesthetic (paying attention to sensations from muscles and joints) representation, rather than visual [5];
- First person presentation rather than third person [6];
- Imagination of movements after an actual action [7];
- Using feedback (when a person is shown how well he is doing a task) [8]. Feedback in the form of virtual reality showed high efficiency: when imagining leg movements, the avatar controlled by the subject goes forward, and when imagining stops, it stops. The subject’s task is to go forward and stop at certain points in virtual space [9–12];
- Simultaneous viewing of a video in which the corresponding movement is performed helps to enhance desynchronization of the mu rhythm due to the work of mirror neurons [13];
- The use of meditative practices, in particular, mindfulness meditation [14].
In addition, we have shown that the effectiveness of motor imagery depends on a person’s personal characteristics [15].
For the experiment, 44 people with a dominant right hand were recruited. All of them were tested using the Cattell questionnaire, which identifies 16 basic individual characteristics. Next, the subjects controlled the BCI based on the imagination of hand movements. It turned out that when imagining the movements of the right hand, expressive, sensitive extroverts were more successful, while when imagining the movements of the left hand, practical, reserved, skeptical and not very sociable people were more successful.
We hypothesize that this can be explained by different levels of dopamine in the right and left hemispheres, as well as differences in the way information about movements is encoded [16]. You can read more about this in the article published by the author and colleagues in the journal “Proceedings of the Academy of Sciences” [15]. Knowledge of the personal psychological parameters of a BCI user can help in the development of individual training and preparation methods before operating neural interfaces.
Why is it necessary to imagine movements and work with neural interfaces? How can this help people with movement disorders? Let's look at these questions using the example of the two most common causes of movement disorders - stroke and spinal cord injury.
What is TES
American and European scientists began to actively study the effect of transcranial brain stimulation on human cognitive abilities relatively recently - and have already received encouraging results. There are many types of TES, but the general idea is this: neurons in the human brain in the area responsible for specific functions are activated by a small external current without surgically invading the body.
The most popular types of such stimulation are placing the patient’s head in an alternating magnetic field created by a special installation (TMS), or placing electrodes on the head, which are supplied with a small and almost imperceptible direct current of 1–2 mA (tDCS). And if a magnetic installation requires a place in a specialized clinic and a lot of money to purchase, then for electrical stimulation of the brain with low currents, several electrodes, salt water and a battery are enough.
Answer questions about love, pass electricity through the brain: 6 experiments in which you can take part
In the United States, transcranial stimulation devices are considered an experimental technology and are not approved by the FDA (Food and Drug Administration), but the laboratory results are causing great interest and optimism among scientists. TES shows positive results on people whose brain functions are impaired in one way or another - patients with severe depression who are not helped by medications, patients after stroke and brain injury, people with drug and alcohol addictions. In experiments on healthy people, the result varies depending on the area where the electrodes are installed: TES temporarily improves memory, empathy, mathematical calculations, reduces anxiety, increases attentiveness and concentration, and one of the latest studies showed improved creativity. But there are also plenty of other studies where no significant results were obtained.
Wired magazine, in its article “Read this before zapping your brain,” pointed out the main problems of studying TES: experiments rarely use groups receiving placebo therapy, since it is quite difficult to emulate the presence of current, and the groups of participants are too small. In addition, the human brain is very complex and individual; in right-handers and left-handers the brain is zoned differently. The brains of children and adolescents under 20 years of age are also in the process of developing neural connections, so the results obtained are unstable, and the topic needs more serious study.
Scientists do not share the enthusiasm of the autodidacts, view home treatment with concern and issue special statements to stop the uncontrolled use of TES at home. In response, skeptics joke: “Since I overclock my brain without additional cooling, if it overheats, will it simply turn off - or will it immediately burn out?”
© SebbyMeister/T&P
Mechanisms of neuroplasticity
During a stroke, an acute disruption of the blood supply to the brain occurs (either as a result of blockage of a vessel by a blood clot - ischemic stroke, or as a result of hemorrhage - hemorrhagic). Since, along with the blood, everything that they need for life ceases to flow to the neurons, the areas of the brain where blood circulation has stopped die off. And if these are areas responsible for motor activity - for example, the motor cortex, then the patient experiences hemiparesis, decreased muscle strength on one side of the body, or hemiplegia, complete paralysis of half the body.
The restoration of motor function is carried out mainly due to the mechanisms of neuroplasticity - the ability of the brain to change under the influence of experience: to establish new connections between neurons, destroy old and unnecessary ones, and restore those lost after damage. These processes involve not only neurons, but also neuroglial cells, as well as the vascular system [17]. The activity of synapses and their number also change [18]. To activate these mechanisms, motor rehabilitation is used in medicine. However, in patients with paralysis or a high degree of paresis, the implementation of real movements is impossible, so they resort to training with a BCI based on the imagination of movements. When imagining movements, the same areas of the brain are activated that are also involved in preparing a real action and in its execution, as a result of which such neurorehabilitation becomes real [19].
Thanks to such rehabilitation training, neurons around the damaged area undergo restructuring: the volume of gray matter in the motor zone of the brain increases, and neighboring areas take on lost functions [20]. The motor areas of the undamaged hemisphere are also involved in this process.
The effectiveness of these exercises can be increased through the use of biofeedback - visual or tactile - when the patient sees on a monitor screen how well he is completing a task (imagining the movement of a limb), or when he feels vibration from a special device when he successfully completes a task.
There are also systems that provide motor feedback: for example, when a person imagines moving his right leg, setting it in motion with a special mechanism. The Biokin system (Kosima LLC), developed under the leadership of Yu.P. Gerasimenko, works on this principle. (Institute of Physiology named after I.P. Pavlov RAS) (Fig. 4) [21]. It includes feedback, functional electrical stimulation (FES) and transcutaneous electrical stimulation of the spinal cord (TESCS), which makes it a highly effective tool in the field of neurorehabilitation of the lower extremities [22].
Figure 4. Biokine. A complex for neurorehabilitation of the lower extremities, based on the use of a BCI with feedback, FES (functional electrical stimulation) and tESCS (transcutaneous electrical stimulation of the spinal cord).
Biokin website
Such systems make it possible to close the sensorimotor loop: from the efferent (outgoing) signal of motor activity sent by the brain to the afferent (incoming) signal of sensory feedback (Fig. 5) [23].
Figure 5. Neuroplasticity induced by motor imagery-based BCI use. When the motor areas of the cortex are damaged, real movement becomes impossible, so to activate the processes of neuroplasticity, only the possibility of imagining movements remains. The use of a BCI with visual and tactile feedback enhances these processes.
adapted from [23]
This rehabilitation mechanism can be explained by the concept of Hebbian plasticity: with the simultaneous activation of two neurons connected to each other, their synaptic interaction increases, which leads to more reliable contact between them (Fig. 6). If we assume that signal transmission from the motor cortex to the limb muscles has been disrupted due to stroke or injury, then simultaneous activation of the sensory and motor cortices may enhance previously inactive connections between neurons through plasticity and thus lead to restoration of motor function of the limbs [ 24].
Figure 6. Hebbian plasticity mechanism. Strengthening the synaptic interaction between two neurons occurs due to repeated stimulation of the postsynaptic cell by the presynaptic cell.
adapted from ""
Figure 7. Formation of new neural connections in the area of spinal cord injury (SCI).
adapted from [25]
When restoring motor function after spinal cord injury, the same mechanisms of neuroplasticity are involved. With such damage, some of the nerve fibers, including motor ones, are interrupted, which causes paralysis of the limbs, while some retain their integrity. Due to this, during neurorehabilitation, it is possible to activate neuroplasticity processes: intact fibers form synaptic connections with motor neurons (motoneurons), which, in turn, transmit a signal to the muscles (Fig. 7) [25].
To increase the effectiveness of neurorehabilitation using BCIs, functional electrical muscle stimulation (FES) is often additionally used. It provides contraction of a muscle at the moment when the user imagines a movement involving this muscle (Fig. [26]. This leads to increased neuroplasticity via the Hebbian mechanism: there is a simultaneous activation of the motor areas of the brain, which transmit signals to the motor neurons of the spinal cord, and sensory neurons, activated by a muscle contracting under the influence of FES, which closes the sensorimotor loop.
It provides contraction of a muscle at the moment when the user imagines a movement involving this muscle (Fig. [26]. This leads to increased neuroplasticity via the Hebbian mechanism: there is a simultaneous activation of the motor areas of the brain, which transmit signals to the motor neurons of the spinal cord, and sensory neurons, activated by a muscle contracting under the influence of FES, which closes the sensorimotor loop.
Figure 8. IMC-FES system. When imagining movements, a signal from the motor cortex is processed by a computer (PC) and transmitted to a functional electrical stimulation (FES) device, which causes contraction of the corresponding muscle. The signal from the muscle is then transmitted to the sensory cortex, providing feedback.
adapted from [26]
1.Electromagnetic stimulation
In modern therapy of neuropathologies and motor disorders, electromagnetic stimulation
finds wide application. In a number of clinical situations, this method has no equal in effectiveness and safety. The validity and effectiveness of this type of functional neurosurgery has been statistically confirmed. The essence of the technique is the constant or systematic impact on the nerve centers of electromagnetic pulses of a certain frequency and amplitude. The effectiveness of this effect has been proven, primarily for parkinsonism, dystonia, uncontrolled spasms and other disorders of muscle tone.
There are different forms of functional muscle pathology
: dystonia, uncontrolled movements, poor coordination, tremors, loss of the ability to walk and perform precise movements. In each specific case, diagnostics is aimed at identifying as accurately as possible the area of the brain that causes dysfunction. To do this, the patient’s electroencephalogram is carefully studied, which gives an idea of the required location of the electrode (localization and depth).
A must read! Help with treatment and hospitalization!
Electrostimulation of the spinal cord
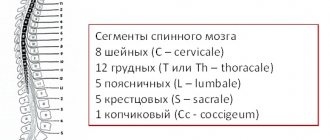
In recent years, electrical stimulation (ESS) has shown great effectiveness in neurorehabilitation after spinal cord injury. The spinal cord has two thickenings: in the neck and lumbar region, which corresponds to the place where the roots of motor neurons of the upper and lower extremities exit from them. In the lumbar enlargement of the spinal cord there are specialized neural networks that ensure the automatic process of stepping (stepping movement generators, GSM). In other words, if you apply electrodes that deliver a current of a certain amplitude and frequency to the dura mater of the spinal cord at the site of the lumbar enlargement, you can induce involuntary walking movements even in people with paraplegia [27]. However, this method requires surgery, so there is a risk of developing postoperative complications.
Currently, transcutaneous electrical stimulation of the spinal cord (TESCS) is considered the safest and most painless. In video 1 (Edgerton Lab, University of California) you can see how involuntary stepping movements of the legs are caused when the patient is in a relaxed position, with his legs suspended on a swing frame [28].
Video 1. Involuntary walking during transcutaneous electrical stimulation of the spinal cord.
Edgerton Lab, University of California
When using TECS, the question of the correct location of the stimulating electrodes arises. If, when installing invasive electrodes during surgery, the segments and roots of the spinal cord are clearly visible, then when installing cutaneous electrodes, it may be difficult to find the desired area. This problem is solved by applying single impulses to the electrode and recording reflex muscle responses - after all, each segment of the spinal cord corresponds to strictly defined muscle groups.
There is also the problem of insufficient amplitude of the impulses sent - due to degenerative processes in the case of spinal cord damage, a large amplitude of stimulation is required to obtain the desired response. However, this can result in burns. Our laboratory has created an optimal device for non-invasive electrical stimulation of the spinal cord [29].
In addition, a system was developed that detects the phases of the walking cycle online and stimulates the spinal cord according to these phases [30]. While walking, different muscles tense at different moments, and joints bend at certain angles, which can be recorded with special devices - accelerometers and gyroscopes. Both legs move in a coordinated manner, and based on the position of one leg, the position of the other can be predicted. The principle of operation of the system is as follows: for a patient with hemiparesis, motion sensors are applied to the healthy leg, which transmit a signal to the TECS device. It, in turn, stimulates at certain points in time groups of spinal cord motor neurons responsible for the movement of the flexor and extensor muscles of the leg, which helps normalize walking and restore movement of the affected limb.
Advances in modern neurorehabilitation
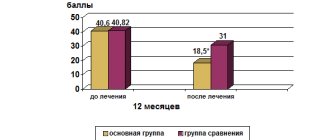
The largest study in the field of neurorehabilitation using a BCI based on motor imagery is the work of Donati et al., published in Nature in 2021 [31]. This study involved eight people with paraplegia caused by spinal cord injury. A special rehabilitation system was developed for them, including six stages of increasing complexity, and about 255 (!) sessions were conducted with each patient during the year.
The first stage included a deep immersion in a virtual reality environment, during which the subject controlled the movement of his avatar (computer character), imagining the movement of the lower limbs in a sitting position. Then the patient did the same, only in a standing position, leaning on a special table. During the third stage, training took place on a treadmill: the subject walked using a device that supports body weight (Lokomat). At the fourth stage, the legs moved in the air, and not on the treadmill. In the fifth stage, the patient trained on a treadmill using a robotic limb support system controlled by a BCI. And at the final stage, the subject walked in an exoskeleton controlled by a BCI: the exoskeleton took a step when the person imagined the movement of the corresponding leg. During all trainings, subjects received tactile feedback - a vibration that was applied to the forearm when a virtual or robotic leg on the same side touched the ground. You can see the experiment diagram in Figure 9, and the rehabilitation process itself in Video 2.
Figure 9. Scheme of the experiment, which includes six stages: 1 - BCI + virtual reality (VR) in a sitting position; 2 — BCI + VR in a standing position; 3 — walking on a treadmill while supporting body weight; 4 - movement of legs in the air; 5 — walking on a treadmill using a robotic system controlled by a BCI; 6 — walking in an exoskeleton controlled by a BCI. Designations: EEG - electroencephalography; EMG - electromyography, which records muscle activity; Tact. - tactile feedback.
[31]
Video 2. The process of conducting the experiment.
[31]
After 12 months of training using this system, all eight patients had improved tactile sensation scores and regained free control of key muscles of the lower extremities. As a result, noticeable progress was seen in their ability to walk. Many patients were able to walk with the help of assistive devices. In addition, all patients showed a significant increase in emotional stability and assessment of quality of life, as well as a decrease in the level of depression and an increase in self-esteem. The condition of the skin and the function of the digestive system have improved, which is apparently associated with the normalization of the activity of the sympathetic and parasympathetic systems. The fact is that along the spine there are nodes of the autonomic nervous system, which regulates the functioning of the internal organs. They are damaged when the spinal cord is injured, which causes disruption of the digestive system, which in turn affects the condition of the skin through the release of signaling molecules, including pro-inflammatory ones [32], [33].
Neurological recovery was associated with plasticity mechanisms at both the spinal cord and sensorimotor cortical levels. Cortical and spinal plasticity alters neural connections in the surviving region of the spinal cord through motor and sensory connections (Figure 10).
Figure 10. Plasticity of the spinal cord (SC) and cerebral cortex through motor (red) and sensory (blue) connections.
adapted from [31]
Indications for TES therapy of the brain
- the need to relieve spondylogenic pain, headaches, post-traumatic pain, postoperative pain, pain syndrome due to pathology of internal organs, fibromyalgia, deforming arthrosis, neuritis, neuralgia, i.e. pain syndromes of various etiologies;
- if it is necessary to normalize the psychosomatic status - treatment of mental, neurological pathology, chronic fatigue or reactive anxiety, depression, during post-stress rehabilitation, to increase working capacity, including in healthy people;
- for hypertension, hypotension, neurocirculatory dystonia, for pain relief, improvement of hemodynamics and rapid healing of tissue damaged during acute but not complicated myocardial infarction;
- sensorineural hearing loss, for vasomotor and allergic rhinitis, recurrent nosebleeds, to stimulate postoperative healing and other ENT pathologies;
- for the treatment of hepatitis, duodenal and gastric ulcers, gastritis, duodenitis, toxic hepatosis, alcohol syndrome, GERD, irritable bowel syndrome and other gastrointestinal pathologies;
- in the treatment of drug addicts to relieve withdrawal symptoms, eliminate cravings for drugs and alcohol, and post-withdrawal affective disorders;
- in obstetrics and gynecology – toxicosis of the first half of pregnancy, treatment of premenstrual syndrome, to stimulate ovulation, for pain relief during childbirth;
- treatment of ophthalmological, dermatological, endocrine, urological diseases;
- in the treatment of burns;
- in sports medicine.