MRI myelography of the spine is a study that allows you to obtain images of the subarachnoid space of the spinal cord. The area of interest is a cavity between the arachnoid and pia mater containing fluid (CSF).
Magnetic resonance imaging
The procedure is performed for neurological disorders accompanied by pain, weakness, numbness of the limbs, neck stiffness and other symptoms. Indications for examination are:
- multiple myeloma;
- suspicion of a tumor;
- diagnosis of intervertebral hernias and other manifestations of osteochondrosis;
- suspicion of vascular pathologies;
- identification of damage to nerves and spinal cord membranes;
- the need to study the condition of the spinal canal, etc.
MRI of the cervical, lumbosacral and other parts of the spine with myelography is done for:
- syringomyelia and other developmental anomalies of the area of interest;
- osteochondrosis;
- discogenic myelopathy;
- compression fractures of the spine;
- traumatic spinal cord injuries;
- intra- and extradural tumors in the spinal canal, etc.
MRI with myelography, what is it?
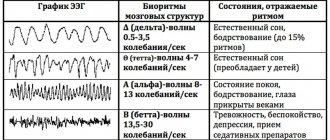
Diagnosis is carried out according to indications as an addition to standard magnetic resonance scanning. MRI of different parts of the spine with myelography involves obtaining T2-weighted images (sequences with gradient or accelerated SE), where the spinal cord with roots is visible against the background of brightly colored fluid.
The described anatomical formations are well visualized by native MRI, but in some cases the addition of a contrast agent may be required. A gadolinium-based drug is injected into a vein.
Indications for contrast:
- suspicion of primary tumors and metastases;
- differentiation of relapse and scar changes after surgery for excision of intervertebral hernias;
- the need to identify the degree of activity of multiple sclerosis;
- more accurate assessment of the condition of the spinal cord, etc.
MRI images of the spine with myelography: hemangioma of the body of the 2nd lumbar vertebra, tumor of the spinal cord region without a cerebrospinal fluid block
Advantages of this type of diagnostics:
- myelography allows us to examine the contours of the spinal cord and nerve roots that are not visualized during x-ray examination;
- Thanks to the study, it is possible to assess the presence and severity of a block in the circulation of cerebrospinal fluid at the level of the pathological process, which directly determines the tactics of treating the patient and the scope of the operation.
In modern diagnostic centers, myelography with three-dimensional reconstruction is performed. The three-dimensional model allows you to examine each part of the spine and identify the smallest pathologies. When conducting contrast-enhanced studies, gadolinium preparations used during the procedure rarely cause side effects and are well tolerated by patients.
Myelography of the spine
Myelography of the spinal column is a method for studying the subarachnoid space and the cerebrospinal fluid tract of the spinal cord. A contrast agent (iodine-containing drug) is injected with a needle through a lumbar puncture into the spinal canal, then a series of real-time radiographic or fluorographic images are taken. In some cases, air may be used instead of a contrast agent (pneumomyelography).
The spinal cord consists of several membranes (soft, arachnoid and hard), the spaces between which are filled with cerebrospinal fluid constantly circulating in the canals. It is on this feature that the study is based. Radiography allows you to track and control the process of filling and spreading the dye, clarify the location and cause of the disturbance in the liquor flow, and diagnose many diseases of the spine, spinal cord and nerve roots.
Indications for the study
Recently, ascending myelography (a water-soluble iodine-containing drug is administered in the lumbar region and its distribution occurs from bottom to top) is performed quite rarely. This is due to the use of more modern non-invasive visual diagnostic methods such as magnetic resonance imaging (MRI) or computed tomography (CT).
Myelography can cause quite unpleasant side effects in patients, so if it is possible to conduct a more gentle study in an adequate time frame, then it is preferred. But in some cases, MRI or CT diagnostics may be contraindicated for the patient (pacemakers, implants, etc.).
Myelography of the spinal column is performed for:
- Detection and treatment of spinal cord tumors.
- Detection and control of treatment of spinal hernia formed in the spinal canal and compressing the spinal cord or nerve roots.
- Diagnosis and control of treatment of spinal neuroma (tumor of the nerve fiber sheath growing from Schwann cells).
- Diagnosis and monitoring of treatment of thoracalgia or neuralgia of the intercostal nerves, other nerve pathologies that cause numbness, impaired reflexes, weakness, paresis or paralysis of the limbs.
- Detecting the causes of cerebrospinal fluid stagnation in the spinal canal.
- Identification and subsequent monitoring of treatment of spinal stenosis or arachnoiditis, which provokes a persistent narrowing of the spinal lumen.
- Detection of inflammation of the arachnoid membrane of the spinal cord or infections affecting soft tissues and/or vertebral bodies and cartilage joints (intervertebral discs).
- Detection of compression or pathologies in the development of blood vessels entwining the spinal cord or cerebral lumen.
- Determining the severity of traumatic injuries to the spinal cord or nerve processes.
Preparation and performance of myelography
The study of the liquor pathways requires some preparation. Eight hours before the procedure, you should refrain from eating, liquid intake should also be limited, and not drink at all two hours before it. You should inform the doctor about medications taken the day before, possible allergic reactions, pacemakers, prostheses or implants located in the body, stop smoking or limit it as much as possible. Women should notify their doctors about the possibility of pregnancy or the presence of an intrauterine device.
Immediately before the myelography, the patient will need to remove clothes (in return he will be offered a special medical gown), jewelry and other metal objects. In the preparation room, he will be placed face down on the couch, with the head of the table usually slightly lowered. To insert the needle into the spinal space, the patient may be asked to turn on his side or sit up.
The puncture site (lumbar region, in some cases cervical region) is disinfected and anesthetized with a local anesthetic, then a needle is inserted. The appearance of drops of cerebrospinal fluid at its end will indicate correct needle insertion. If necessary, the manipulation nurse can take a sample of the fluid for additional research. If the advancement of the tip is difficult, then the needle is slightly returned and the next attempt is made with a slight change in the angle of injection. A contrast agent is then injected and the patient lies down on his stomach again.
The spread of contrast throughout the subarachnoid space is recorded with a fluorograph, outlining the contours of the spinal cord and adjacent nerve roots. It is advisable to remain completely still while taking x-rays to avoid image blur.
In some cases, to clarify the indications, immediately after the completion of myelography and while the contrast fluid is still in the spinal column, the patient may undergo CT diagnostics. On average, the liquor examination procedure takes 30-60 minutes, with an additional CT examination plus another 15-20 minutes.
Sensations expected during myelography and after the study
When a local anesthetic is administered, the patient will feel a slight prick in the lumbar region. When the needle is inserted into the intervertebral space, a feeling of slight pressure or slight nagging pain will appear. During the administration of a contrast agent, the following effects may occur:
- short-term burning sensation at the injection site when the solution is administered;
- feeling of spreading warmth;
- slight dizziness or headache, a feeling of pressure in the back of the head;
- redness or a slight tingling sensation of the skin;
- salty or metallic taste in the mouth, nausea, and much less often vomiting.
After completing the diagnostic procedure, the patient is transferred to a ward, where he needs to lie down for 3-4 hours with the head of the bed slightly elevated or a high pillow. In order to remove the contrast agent from the body as quickly as possible, increased fluid intake is recommended. For two to three days after the procedure, it is advisable to refrain from vigorous physical activity, sports, and sudden bending.
As a rule, the patient feels quite well the next day, but if nausea, headache, dizziness or numbness of the extremities does not go away for several days, and is accompanied by a deterioration in health and fever, you should immediately consult a doctor. This may be a sign of the onset of inflammatory processes.
Benefits and risks of diagnosis
Advantages:
- CSF examination is considered a fairly safe and painless method;
- the introduction of contrast agents makes it possible for the radiologist to examine the outlines of the spinal cord and nerve roots, which is not always possible with conventional radiography;
- The procedure performed leaves absolutely no effects of radiation exposure in the patient’s body.
Risks:
- the introduction of additional fluid into the subarachnoid space can cause headaches and increased intracranial pressure, which normalizes only after some time;
- damage to soft tissues (muscular, nervous, circulatory, cartilage) during needle insertion into the spinal column;
- the occurrence of allergic reactions (rashes, redness of the skin, difficulty breathing) after the administration of a contrast agent;
- the occurrence of inflammatory processes in the membranes of the spinal cord at the injection site;
- progression of the development of malignant tumors after receiving a dose of radiation.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
What does MRI of the spine with myelography show?
Diagnostics helps in detecting:
- liquor blocks at the level of the pathological process in the spinal canal;
- intervertebral disc diseases;
- dystrophic and degenerative changes in the musculoskeletal system (spondylopathies);
- spinal cord lesions (myelopathy);
- arachnoiditis (inflammation of the arachnoid membrane);
- spinal canal stenosis;
- cystic formations;
- cerebrospinal fluid fistulas accompanied by leakage of cerebrospinal fluid;
- developmental anomalies, etc.
Using myelography, it is possible to establish pathology and determine the dynamics of the process.
There are restrictions on the use of the procedure. Contraindications include:
- the presence of metal structures and electronic devices in the patient’s body;
- pregnancy (1st trimester - for native MRI, the entire gestation period - for studies with contrast);
- intolerance to amplifier components (a standard scan can be performed).
When is myelography required?
The examination of the spine using the method under consideration can be carried out when:
- compression fractures;
- myelopathy of discogenic type;
- osteochondrosis of the spine in a severe stage;
- any spinal cord injuries;
- arachnoiditis (inflammatory process);
- infectious diseases of the spinal canal or processes.
In addition, as a diagnostic procedure, myelography is performed in case of suspected damage to the nerve roots of the spine, progression of malignant tumors, or problems in the functioning of the spinal vessels.
Preparing for MRI with myelography
No special measures are required before the procedure, but several nuances must be taken into account:
- the patient should inform the clinic staff about recent or active diseases or medications taken;
- the patient must warn the staff about the presence of allergies to medications, bronchial asthma;
- women should inform the radiologist about existing or suspected pregnancy;
- During lactation, preparation involves expressing and storing breast milk for two feedings.
Extramedullary tumor of the spinal cord on MRI (indicated by an arrow) of the thoracic region
Decoding the results
Myelography with an iodine-containing drug is interpreted by a doctor with the appropriate qualifications, usually a radiologist. Based on the results of decoding, a conclusion is drawn up, which is given to the patient and with which he can go to the attending physician.
Advantages and disadvantages of the procedure
The advantages of the procedure are that it allows you to quickly identify problems that neither CT nor MRI without contrast would reveal. You can examine not only the spine, but also the spinal cord and nerve roots, which are almost impossible to see with other studies. As a result of the procedure, no traces of radiation remain in the body.
The disadvantages are that the administration of contrast does not give the most pleasant sensations: there is often a salty taste in the mouth, redness of the facial skin, a feeling of heat or burning, dizziness or headaches. Nausea or even vomiting may occur after contrast administration is stopped. Also, the procedure is not possible in all cases, since there are contraindications.
How does an MRI of the spine with myelography work?
Before the procedure, the patient takes off clothes, jewelry, accessories that contain metal, and leaves personal items in the wardrobe.
A magnetic tomograph is a structure made of a pipe with a field generator and sensors and a movable table. The subject lies on his back on a conveyor, his limbs and torso are secured with straps. A series of photographs are taken of the area of interest. If reinforcement is necessary, the drug is injected into the vein and the manipulations are repeated. During contrast, the patient does not experience pain; in rare cases, the following is observed:
- feeling of warmth in the body;
- flushed face;
- slight dizziness;
- nausea.
The described phenomena usually go away on their own after the procedure is completed.
Intravenous contrast is preferable due to its low morbidity and obtaining additional information for a number of pathologies (tumors, inflammation, etc.).
Depending on the number of anatomical areas examined, the procedure lasts 30-60 minutes. It is important that the patient remains still during the scan. In case of pain syndrome, it is necessary to discuss in advance with your doctor the issue of taking an analgesic.
To quickly remove the contrast agent, an increased drinking regime is observed. Drinking large amounts of fluid helps get rid of excess drug.
What should you expect during and after the study?
When a local anesthetic is injected under the skin, the patient feels a prick, and when the needle is inserted into the spinal space, a slight pressure sensation appears. In some cases, needle insertion is accompanied by severe pain.
During the examination, when tilting the table at different angles, the doctor asks the patient to lie as still as possible. Slipping off the table is prevented by securing straps or a footrest. The need to be face down on the table is a certain inconvenience, but this does not last long. In rare cases, when the table is tilted, the patient experiences difficulty breathing or swallowing. It is important to communicate this to the radiologist, who will adjust the table to a more comfortable position.
After the administration of contrast, headache, nausea, or a feeling of a rush of blood to the skin occasionally occur. Seizures are also possible, but they are extremely rare with the use of modern contrast materials.
After completing the study, the patient is transferred to a ward, where a doctor or nurse monitors his condition and vital signs for a couple of hours. In some departments, the patient remains for 4 hours in a lying position with the head end of the bed elevated to 30-45°. To facilitate the removal of contrast material from the body and prevent headaches during this period, an enhanced drinking regimen is recommended. After myelography, intense physical activity and bending are contraindicated for 1-2 days.
A rise in temperature above 37.5°C, severe nausea or vomiting, severe headaches that last more than 24 hours, stiff neck and numbness in the legs should be reported to your doctor immediately. It is also important to notify the doctor if there is a problem with urination or defecation.
Up
Interpretation of an MRI image of the spine with myelography
Myelograms are interpreted by a radiologist. After studying the images of the spine, the specialist forms a conclusion with detailed information about the detected changes. The final diagnosis is made by the clinician based on medical history, magnetic resonance imaging results and other research methods.
A radiologist examines MRI images.
In St. Petersburg, examination of any part of the spine with additional myelography using an expert-class Siemens Symphony 1.5 T device can be performed at the Magnit clinic. Sign up for an MRI using the number!
Contraindications for
It is impossible to undergo myelography in the following cases:
- state of fever;
- diseases of the kidneys, heart, liver in the stage of decompensation;
- severe arthritis;
- pregnancy;
- previous spinal surgeries;
- anatomical features or defects that prevent the introduction of a substance into the subarachnoid cavity;
- infectious processes on the skin in the place where contrast needs to be administered;
- inability to maintain one position during the procedure.
The final decision should be made by the doctor, since sometimes it happens that the possible risk is less than the benefit of the x-ray procedure.
MR 3D myelography description
Modern magnetic resonance imaging scanners allow a three-dimensional (3D) reconstruction of the examination area. Using this function of the software application, it is easier to describe the images, but you should know the normal anatomical features of the structure of the spinal segment.
Scheme of contrast cisternography of the brain (a) and MR myelography of the spinal cord (b). Such tomograms could be obtained at the beginning of the use of magnetic resonance imaging in medicine. Technology gradually improved. Contrast intravenous MRI of the spine with 3D modeling began to be used somewhat later.
Sagittal sections from MRI of the spine. Studies were performed on a patient with stenosis at levels C3-C6 before surgery to install stents. 3D reconstruction allowed for high-quality surgical treatment.
Progress of the procedure
Before the milography, the patient needs to undress, remove all jewelry and dentures. He is given a special medical shirt. During the procedure, the patient most often lies on his stomach on the X-ray table. But depending on the purpose and location of the examination, he can sit or lie on his side. The doctor disinfects the skin at the puncture site and numbs it with an anesthetic. Most often, the puncture is done in the lumbosacral region between the disc and the vertebra. The needle is inserted slowly, under constant x-ray control. After administering the contrast agent, the doctor removes the needle and disinfects the skin again.
The patient remains in a stationary position, and the table beneath him is slowly tilted, which allows the injected substance to spread into the cavity of the spinal canal. Sometimes the patient also needs to turn from side to side so that the entire cavity is filled. Using a fluoroscope, the doctor tracks the spread of the contrast agent, noting where it has been slowed down. Next, X-rays or computer images of the spine are taken. It is best for the patient to turn on his side. It is very important to remain completely still during the procedure. Taking into account the time required to analyze the results obtained, the entire procedure takes from half an hour to an hour. Sometimes a re-examination may be required after a few hours.
Technique
The patient lies on his stomach. At the puncture site, the skin is disinfected and numbed with local anesthetic. Depending on the puncture site, when the needle is inserted, the patient can sit, lie on his side or on his stomach. The needle moves deeper under the control of a fluoroscope, and after introducing the contrast material, it is removed and the skin is disinfected again. The patient remains face down on the table.
The doctor slowly tilts the table to spread the contrast agent throughout the subarachnoid space.
To take X-rays, the patient turns on his side and must remain as still as possible during the X-ray to reduce the likelihood of image blur.
You must wait some time after the procedure for the doctor to analyze the resulting images. In general, myelography takes 30-60 minutes.
The video shows the procedure:
When the anesthetic is administered, the patient feels a prick, and when the needle is inserted into the canal, a slight pressure is felt.
Rules for the patient
To avoid discomfort during the procedure, as well as complications after it, it is very important to know the features of myelography and the rules for its implementation. Painful sensations rarely occur, but if the patient is afraid of pain, it is better to tell the doctor about it. In this case, he will be given a sedative to help him calm down. During the procedure, you must follow all the doctor’s recommendations and warn him about all side effects and discomfort.
After myelography, the most important thing is to quickly remove the contrast agent from the body. To do this, you need to drink as much fluid as possible, and after 2-3 days start doing certain exercises that would increase blood flow and metabolic processes.
Myelography of the spine is one of the most reliable methods for examining it. With its help, the doctor can examine the condition of all tissues, see pathologies of its structure, disturbances in the functioning of even the smallest vessels and nerves.
How to prepare for myelography
Before the study, the doctor will ask the patient in detail about the medications he is taking. Danger for the subject during myelography is represented by such groups of drugs as hypoglycemic (in particular, metformin), blood thinners (for example, warfarin), anticonvulsants and antidepressants. A few days before diagnosis, these medications should be stopped and replaced with other drugs of similar effect recommended by the doctor.
The patient should inform the doctor in detail about all allergy episodes he has had. Allergy to iodine and barium is of particular importance, since many contrast agents are based on these microelements.
The doctor must also know about all the patient's chronic diseases. Firstly, for some of them, myelography is completely contraindicated, and secondly, knowing about these diseases, specialists conducting the study can anticipate the development of certain complications and in a timely manner, and most importantly, respond adequately to them.
It is extremely important for women to notify their doctor if they may or may be pregnant because X-rays may have negative effects on the health and development of the fetus.
2-3 days before the study, the patient should exclude from his diet foods that cause fermentation and increased gas formation in the intestines (cabbage, baked goods, etc.) - the presence of a large amount of gas in it can “blur” the picture during the study. On the contrary, the amount of fluid consumed should be increased. It is not recommended to eat any food 8 hours before myelography, but you should still drink if you feel thirsty.
Before the puncture, susceptible patients may be prescribed sedatives; in addition, all subjects are given a cleansing enema.
During the examination, the patient removes some or all of his clothing and puts on a special hospital gown. It also removes glasses, jewelry, dentures, watches and other objects that may distort the image.
Hemorrhage without myelography: MRI provides quality and contraindications
During operation, MRI scanners are accompanied by a strong magnetic field, so any metal objects in the human body begin to move under the influence of radiation. Because of these features, some patients are contraindicated for MR myelography or other MRI procedures.
Magnetic resonance imaging cannot be performed on the following categories of patients:
• With the presence of pacemakers, pacemakers; • Electrocochlear devices, neurostimulators; • Postoperative clamps of aneurysms; • Orthopedic joint prostheses; • Sternal suture wire; • Third trimester of pregnancy; • Patients with claustrophobia.
Scanning creates a lot of noise. To suppress it, headphones are recommended for a person. Pleasant music can relax the patient, but in case of neurological disorders or fear of closed spaces, it is advisable to give the person a sedative before the examination.
Indications for scanning are:
- pain in the back, in the lower extremities, of varying severity, unilateral or bilateral
- sensory disturbances (paresthesia, numbness) or motor disturbances in the legs (up to paresis/paralysis)
- previous spinal injury
- search for metastases or primary cancerous node
- upcoming or previous surgery
- presence of signs of neurological impairment of other organs (for example, breathing problems, vision problems, heat intolerance)
How MRI of the lumbosacral region will help the doctor
Only a radiologist or a functional diagnostics specialist can interpret the MRI results. To do this, images are compared over time to track changes in condition, or compared with an image of a healthy spine to identify possible pathologies.
MRI of the lumbosacral spine makes it possible to detect a number of serious diseases and determine the course of treatment. The procedure can be carried out as needed. The images obtained during the diagnosis clearly show the bones, cartilage tissue (highlighted in dark color) and the spinal cord (light color).
This allows the doctor:
- identify defects, injuries and pathologies of the vertebrae;
- detect inflammatory processes or neoplasms;
- find out the size and nature of traumatic injuries;
- examine the condition of blood vessels and nerve tissues in the spine;
- identify osteochondrosis, inflammation of the spinal membranes on an MRI image;
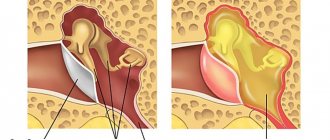
- find out whether the patient has a hernia, which on T-2 weighted images looks like a protrusion with structures, namely the intervertebral disc, muscles, longitudinal ligaments.
What is myelography: MRI contrast of the spinal cord
MR myelography is a research method based on the study of about 14 types of various biochemical information (differences in the structure of water and fat tissue) without the use of radiation exposure, but requiring invasive injection of contrast into the subarachnoid space.
Magnetic tomography visualizes the membranes of the spinal cord and brain well without contrast, but a contrast agent is added to identify the cause of compression. Using magnetic resonance angiography (MRA), it is possible to visualize the state of the blood supply to the veins and arteries.
MR myelography allows you to identify malignant and benign brain tumors that may cause compression of brain tissue. The study has broad potential for diagnosing pathology of soft tissue structures.
MR angiography allows one to detect vascular abnormalities with a high degree of certainty. Used to assess the condition of veins and arteries. The study determines the state of blood flow, which changes in the presence of malignant and benign neoplasms.
In the images, areas of demyelination are marked as foci of signal with increased intensity. The shape of such a section is oval or rugged. If 4 similar fragments are detected, verification of the diagnosis is beyond doubt.