Methods of functional diagnostics in neurology. Part 1
What methods of functional diagnostics exist, what do they allow you to find out, what are the advantages of these methods, what is an EEG, when is it worth doing an electroencephalogram, says Dmitry Aleksandrovich Ovchinnikov, neurologist, functional diagnostics doctor.
Ovchinnikov Dmitry Alexandrovich Doctor of functional diagnostics.
Hello. My name is Dmitry Aleksandrovich Ovchinnikov. I am a neurologist, functional diagnostics doctor at the Scandinavia clinic. Today we will talk about functional diagnostic methods in neurology. Neurology is a branch of medicine that deals with the diagnosis and treatment of disorders of the nervous system. Functional diagnostics is a very diverse group of methods that are united by one principle. Assessment of not only and not so much the static state of the system, but the functioning and functioning of organs. In this way, functional diagnostic methods compare favorably with other groups of techniques, such as radiation diagnostic methods, where the structure is assessed primarily at each specific point in time, or laboratory diagnostic methods, which evaluate the composition of tissues and fluids, but only at one specific point in time. It becomes clear why functional diagnostics is so important in neurology, because the nervous system is an extremely dynamically changing structure, the main task of which is to respond to external and internal stimuli and change its functioning over time.
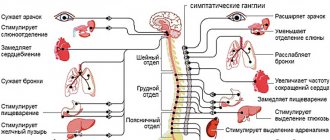
Let's briefly look at the functional diagnostic tools available to neurologists. A large group of functional diagnostic methods are united by their electrophysiological principle. Nerve cells in the course of their work are capable of being excited, changing the polarity of their membranes and generating an action potential. Fixation and registration of this action potential allows a number of functional diagnostic methods to study nerve tissue and draw certain conclusions about the functioning of the nervous system. These methods include electroencephalography, electromyography, evoked potential methods, and a number of other electrophysiological techniques.
One of the electrophysiological methods of functional diagnostics in neurology is electroencephalography, or EEG for short. Electroencephalography is a technique for assessing the bioelectrical activity of the brain. During the study, electrodes are placed on the patient's head to record brain activity in various areas of the brain. Also during the research, functional tests are carried out, such as photostimulation or tests with changes in the gas composition of the blood, followed by stimulation of the brain with hyperoxygenation. The results of measuring this activity are currently processed by a computer and displayed on the monitor in the form of graphs. The doctor is able to perform various types of analysis of this recording so that the conclusions are as comprehensive and profound as possible. The studies are carried out in a shaded room, but do not involve any discomfort. Lasts from 15 to 30 minutes.
There are also methods for long-term recording of electroencephalograms, but they are used less routinely. With some exceptions, an electroencephalogram does not require any preparation, but on the day of the study it is recommended to wash your hair to reduce skin resistance to electric current.
A serious advantage of the electroencephalogram over other research methods is the ability to assess the functioning of the brain over a certain period of time. What no other technique can provide, such as MRI, which allows a very precise and very comprehensive assessment of the structure and anatomy of the brain, but cannot assess its functioning during a specific drive. Or such as computed tomography, which evaluates primarily the bone structure of the skull and the structure of the brain without detailed differentiation. Thus, various types of electroencephalogram are the gold standard in the diagnosis of epilepsy and various epi-syndromes. No other technique currently used in clinical practice is capable of identifying these deviations.
The experience accumulated by the Soviet, Russian and international scientific schools allows the use of EEG not only in the diagnosis of epilepsy. Encelography makes it possible to indirectly judge violations of recoordination, the work of the hypothalamic-pituitary system, the functioning of the brain and cerebral cortex as a whole, and the relationship between the work of the cortex and subcortical structures. Certain changes in the encephalogram can give the doctor the opportunity to judge the functioning of the cognitive component and the exhaustion of the nervous system. Thus, today an electroencephalogram is one of the few methods that allows us to evaluate not only structural changes in the brain, but also changes in its functioning.
Indications for an encephalogram at the moment are loss of consciousness of any origin, functional disorders of the nervous system, such as neurotic, psychological, emotional, psychosomatic complaints of patients. Assessment of the consequences of traumatic brain injuries, assessment of the consequences of neuroinfections. Theoretically, we can evaluate the functioning of the hypothalamic-pituitary system and its impact on brain function. Previously, electroencelography was used to assess changes in the structural properties of nervous tissue to search for focal changes, such as tumors and hematomas. However, at the moment, MRI copes much better with these tasks.
In addition to the indications described above, it is advisable to conduct electroencelography when there are changes in brain function caused by vascular disorders, disorders caused by chronic changes in cerebral blood flow.
Publication date: 04/10/17
Instrumental studies in the diagnosis of dizziness
A feeling of imaginary rotation or movement of surrounding objects or the patient himself - in practice, the term “dizziness” is often interpreted much more broadly and also implies feelings of instability and spatial disorientation, which are usually called “non-systemic dizziness”.
We present to your attention some features of instrumental methods for diagnosing dizziness:
Differential diagnostic algorithm for dizziness:
- Determining the presence of dizziness
- Determining the type of dizziness
- Finding out the causes and circumstances of dizziness
- Identifying neurological or related causes of dizziness
- Depending on the identified symptoms in some patients - instrumental examination
Currently, many patients suffering from peripheral vestibular vertigo or psychogenic vertigo are mistakenly diagnosed with cerebrovascular disease, vertebrobasilar insufficiency, vertebral artery syndrome, cervical osteochondrosis, etc. Often, the existing diseases are not diagnosed and their effective treatment is not carried out.
Instrumental studies
Instrumental studies for dizziness are not always necessary. In 60-70% of cases, the diagnosis can be made based on questioning with an analysis of complaints and medical history, as well as somatic, neurological and neurovestibular examinations.
Neuroimaging methods - CT and MRI
Always necessary when detecting central vertigo. With their help, diagnose cerebral infarction, cerebral hemorrhage, MS, anomalies of the craniovertebral junction, tumors of the brain stem, cerebellopontine angle and many other diseases manifested by dizziness. However, modern high-resolution CT and MRI systems create images of not only the brain, but also the pyramid of the temporal bone and formations of the peripheral vestibular system, which makes it possible to identify schwannomas located in the internal auditory canal, as well as cholesteatoma. MRI can detect neurovascular compression of the vestibular-cochlear nerve - the cause of vestibular paroxysmia (a rare disease manifested by paroxysmal vertigo).
Cardiac research
Consultation with a cardiologist, ECG, Holter ECG monitoring, echocardiography, and other studies are indicated if cardiogenic origin of dizziness is suspected.
X-ray of the cervical spine
When examining a patient with dizziness, it is of little information and should not be used in the absence of obvious indications, for example, the development of dizziness after a neck injury. In most middle-aged and elderly patients, radiography reveals degenerative-dystrophic changes (spondylosis, osteochondrosis), which in most cases are not associated with the development of dizziness.
Electronystagmography
Allows you to quantitatively assess the movements of the eye phenomena and, thereby, diagnose various forms of nystagmus at rest and during stress tests (for example, caloric and rotational). In this study, two electrodes are placed near each eye in the vertical and horizontal planes to record the movements of the eyeballs.
Videooculography
Currently used more often than electronystagmography. Movements of the eyeballs are recorded using infrared video cameras built into special glasses. The results of the video recording are processed and analyzed by a computer program, which allows you to get a complete picture of the movement of the eyeballs and nystagmus. The method significantly increases the sensitivity of the study of nystagmus, as well as positional tests and other methods of neurovestibular research.
Caloric test
It consists of alternating exposure of the peripheral part of the vestibular analyzer to different temperatures by irrigating each external auditory canal with cold (30° C) and hot (40° C) water or air. Cold exposure depresses the vestibular apparatus, hot influence stimulates it. Normally, cold water irrigation causes contralateral caloric nystagmus, and hot water irrigation causes ipsilateral caloric nystagmus. The absence or weakening of caloric nystagmus during caloric stimulation of one ear is characteristic of diseases of the peripheral vestibular apparatus.
Rotational test (Barany test)
It has been used relatively rarely in recent years because it is less informative than the caloric test and is less well tolerated by the patient.
Computer dynamic posturography
Examines the balance of a standing subject by recording position, deviations and other characteristics of the projection of the general center of gravity onto the plane of support. The dynamic posturography system consists of a platform and booth designed to assess both motor and sensory components of balance. It is also often used as a rehabilitation system.
Electrocochleography
The method of studying the evoked potential of the cochlea is used to diagnose Meniere's disease and perilymphatic fistula. Electrocochleography provides registration of the electrical activity of the cochlea and auditory nerve that occurs in the interval 1–10 ms after the presentation of a sound stimulus. It includes presynaptic receptor activity, which includes the microphone potential and summation potential (SP), as well as postsynaptic activity, represented by the action potential (AP) of the auditory nerve. In clinical practice, the assessment of SP and PD is of primary importance, and the SP/PD amplitude ratio of more than 0.35 - 0.5 indicates endolymphatic hydrops - the pathophysiological basis of Meniere's disease.
Pure-tone threshold audiometry
Determination of auditory sensitivity to sounds of different frequencies. The perception of sounds up to 25 dB is considered normal. Depending on the degree of hearing loss, hearing loss is classified into mild (hearing threshold increased to 40 dB), moderate (up to 55 dB), severe (up to 90 dB). For differential diagnosis of sensorineural and conductive hearing loss, the auditory threshold for air and bone conduction of sound is compared. Conductive hearing loss involves normal bone sound conduction but impaired air conduction. Conductive hearing loss can be caused by damage to the outer or middle ear (cerumen plug, otosclerosis). Sensorineural hearing loss is characterized by simultaneous impairment of bone and air conduction. Sensorineural hearing loss can be caused by damage to the cochlea or vestibulocochlear nerve.
Duplex ultrasound scanning of the brachiocephalic arteries
It plays an important role in the diagnosis of CVD, but as a rule does not allow us to establish the cause of dizziness.
Neurology examination methods in the clinic
Ultrasound Dopplerography of extracranial vessels - study of the condition of the carotid and vertebral arteries. Provides information important for diagnosis and treatment in case of cerebrovascular insufficiency, various types of headaches, dizziness (especially associated with turning the head) or instability when walking, attacks of falls and/or loss of consciousness.
Transcranial Doppler ultrasound is a method for studying blood flow in the vessels of the brain. Used in diagnosing the condition of cerebral vessels, the presence of vascular anomalies, impaired outflow of venous blood from the cranial cavity, identifying indirect signs of increased intracranial pressure
Doppler ultrasound of peripheral vessels is a study of blood flow in the peripheral vessels of the arms and legs. The study is informative for complaints of pain in the extremities during exercise and lameness, chilliness in the arms and legs, changes in the color of the skin of the arms and legs. Helps in the diagnosis of obliterating diseases of the vessels of the extremities, venous pathology (varicose and post-thrombophlebitis diseases, incompetence of venous valves).
Doppler ultrasound of the ocular vessels allows one to assess the degree and nature of blood flow disturbances in the fundus due to blockage of the arteries of the eye, hypertension, and diabetes mellitus.
Ultrasound diagnosis of vascular diseases using duplex scanning is a fast, highly informative, absolutely safe, non-invasive research method. Duplex scanning is a method that combines the capabilities of visualizing vascular structures in real time with the characteristics of blood flow in a given vessel under study. This technology in some cases can exceed the accuracy of X-ray contrast angiography.
M-Echo (Echoencephalography) - ultrasound encephalography, a method of studying the brain using ultrasound. It is based on the property of ultrasound to be reflected from the boundaries of media (structural formations of the brain) of different densities. The main diagnostic criterion is the deviation of the median echo, or M-echo, which is the reflection of ultrasound from the midline structures of the brain (epiphysis, 3rd ventricle, transparent septum, interhemispheric fissure). Normally, the M-echo, recorded as a peak on an ultrasound encephalogram, coincides with the midline of the head. The use of echoencephalography is effective in recognizing and localizing so-called volumetric intracranial pathological processes (tumors, abscesses, hematomas, parasitic cysts, etc.).