Benedict's syndrome (syn. alternating paralysis syndrome)
The syndrome occurs as a result of a pathological process in the medial-dorsal part of the midbrain at the level of the red nucleus and the cerebellar-rednuclear tract with the preservation of the paramidal fasciculus. The causes of the lesion are thrombosis and hemorrhages in the posterior cerebral artery basin, tumor metastasis.
Clinical signs and symptoms. On the affected side, extrapyramidal hyperkinesis in the limbs and cerebellar ataxia occur. On the side opposite to the localization of the lesion, mild spastic hemiparesis and tremor of the lower extremities develop. Against the background of hemiparesis, increased tendon reflexes are observed.
In addition, there is an increase in overall muscle tone. Eye symptoms are caused by complete or partial paralysis of the oculomotor nerve. Ptosis occurs on the side of the pathological focus. There is a deviation of the eyeball towards the lesion, there may be disturbances in associated eye movements during convergence and the direction of gaze up or down. A differential diagnosis of this syndrome is made with the following syndromes: Claude, Weber-Gubler-Gendrin, Millard-Gubler, Fauville, Nothnagel.
The development of the syndrome is associated with a pathological process located directly in the region of the cerebral peduncles, which occurs as a result of hemorrhages, ischemic cerebral circulation disorders, as well as neoplasms. In addition, the signs of this syndrome may be caused by dislocation compression of the cerebral peduncles by a tumor located at a distance.
Clinical signs and symptoms. Due to damage to the facial and lingual nerves, as well as the pyramidal tract, paralysis of the muscles of the face, tongue and limbs of the central type occurs on the side opposite the pathological focus. Eye symptoms are caused by complete (ophthalmoplegia, ptosis, mydriasis) or partial (damage to only intraocular muscles or individual extraocular muscles ) oculomotor nerve palsy.
Symptoms of paralysis occur on the side of the pathological focus. In case of damage to the extraocular muscles innervated by the oculomotor nerve, the eyeball deviates towards the temple and “looks” towards the pathological focus, “turning away” from the paralyzed limbs. If a pathological process - for example, an aneurysm of the anterior cerebral artery - involves the optic tract or the external geniculate body, homonymous hemianopsia occurs.
Unilateral damage to the ventral part of the pons involving the nucleus or bundle of fibers of the facial nerve, the root of the abducens nerve and the underlying pyramidal tracts leads to the development of this syndrome. The pathological process in this area may be associated with impaired circulation in the paramedian arteries (hemorrhages, thrombosis).
With the development of a tumor of the pons (most often glioma and much less often cancer metastasis, sarcoma, solitary tubercles), a slow gradual development of the syndrome is observed. Clinical signs and symptoms. On the affected side, signs of peripheral paralysis of the facial nerve appear, while central hemiparesis or hemiplegia is observed on the side opposite the lesion.
{module direct4}
Ocular symptoms are caused by damage to the abducens and facial nerves. On the side opposite the pathological focus, signs of damage to the abducens nerve appear - paralysis of the external rectus muscle, convergent paralytic strabismus, diplopia, which intensifies when looking towards the affected muscle. On the contrary, symptoms of damage to the facial nerve are observed on the side of the pathological focus - lagophthalmos, lacrimation.
The pathological process in this syndrome is located at the base of the legs and involves the fibers of the oculomotor nerve. The development of the syndrome is caused by damage to the branches of the posterior cerebral artery - the middle and posterior arteries of the red nucleus, which supply blood to the lower parts of the red nucleus. The most common causes of vascular damage are atherosclerosis and syphilitic endarteritis.
Dictionary
Alternating syndromes often accompany unilateral brainstem lesions. Alternating syndromes are characterized by conduction disturbances on the side opposite to the lesion and dysfunction of the cranial nerves on the affected side. Weber syndrome occurs when the nuclei or fibers of the oculomotor nerve are damaged. In this case, symptoms of damage to the third pair of cranial nerves on the side of the lesion, hemiplegia, develop. Weber syndrome is accompanied by simultaneous damage to the corticonuclear tracts of the facial and hypoglossal nerves, which is manifested by central paralysis of the muscles of the tongue and face. In Benedict's syndrome, the lesion is located at the same level as in Weber's syndrome. In this case, the red nucleus and substantia nigra are involved in the pathological process. Clinically, the syndrome is manifested by paralysis of the peripheral oculomotor muscles on the affected side and intentional hemitremor on the opposite side. In the case of a larger lesion, simultaneous damage to the fibers of the medial lemniscus occurs. In this case, clinical manifestations are accompanied by impaired sensitivity on the opposite side (superficial and deep). With this syndrome, coordination of movements is impaired, hemihyperkinesis develops, as well as muscle hypotonia, which is associated with damage to the superior cerebellar peduncle. With Claude's syndrome, coordination of movements is impaired, hemihyperkinesis develops, as well as muscle hypotonia, which is associated with damage to the superior cerebellar peduncle. At the same time, the nucleus of the oculomotor nerve is affected with the development of paralysis of the muscles innervated by it, of a peripheral nature. The cause of Nothnagel syndrome, leading to its occurrence, is simultaneous damage to the nuclei of the third pair of cranial nerves, the superior cerebellar peduncles, the lateral lemniscus, the pyramidal tract, and the corticonuclear tract. Clinically, Nothnagel syndrome is manifested by paresis of peripheral oculomotor muscles, ataxia on the affected side, bilateral hearing loss, paresis of muscles innervated by the facial and hypoglossal nerves of a central nature. Millard-Gubler syndrome occurs when the nuclei or fibers of the facial nerve, as well as the pyramidal tract, are damaged. Clinically, the syndrome is manifested by the development of paralysis of the facial muscles on the side of the peripheral lesion and the development of central hemiplegia on the side opposite to the lesion. Fauvelle's syndrome occurs with lesions more extensive than with Millard-Hubler syndrome. At the same time, the nucleus or fibers of the abducens nerve are affected. Clinically, Fauvelle's syndrome is characterized by the presence of all manifestations of Millard-Gubler syndrome with the addition of paralysis of the abductor muscle of the eye, which is manifested by convergent strabismus, diplopia and failure to bring the eyeball out. Brissot-Sicard syndrome affects the fibers of the pyramidal tract, with simultaneous irritation of the nuclei of the VII pair of cranial nerves. Clinically, the syndrome is manifested by contralateral spastic hemiparesis and spasm of the facial muscles on the side of the lesion of the facial nerve. Raymond-Sestan syndrome develops with simultaneous damage to the pyramidal tract, fibers of the posterior longitudinal fasciculus, medial lemniscus, middle cerebellar peduncle, and the center of gaze located in the pons. Clinically, the syndrome is manifested by ataxia, choreoathetoid hyperkinesis, gaze paresis directed towards the lesion, on the opposite side - hemianesthesia and spastic hemiparesis. Grene's syndrome occurs when the trigeminal nucleus, which is responsible for superficial sensation, is damaged, as well as the spinothalamic tract. The syndrome is manifested by a violation of pain and temperature sensitivity on the face on the affected side, up to its complete loss. Sensory impairment occurs in a segmental manner. On the opposite side, the superficial sensitivity of the trunk and limbs is impaired according to the conductive type. Jackson syndrome develops as a result of damage to the central nervous system in the region of the nucleus of the XII pair of cranial nerves. Clinically, this syndrome is manifested by paralysis of the peripheral tongue muscles on the affected side and central hemiplegia on the side opposite to the lesion. Avellis syndrome is the result of simultaneous damage to the nucleus ambiguus, common to the glossopharyngeal and vagus nerves, or the fibers of these nerves and the fibers of the pyramidal tract. It is noted by paresis of the soft palate, vocal cords, impaired swallowing, speech, phonation, on the side of the lesion. We recommend sanatorium-resort treatment in sanatoriums with a medical profile: treatment of diseases of the nervous system: sanatoriums " Solvychegodsk " ( Arkhangelsk region ), " Yangan-Tau " (Bashkortostan ), " Elton " ( Volgograd region ), " Talgi " ( Dagestan ), " Obolsunovo " ( Ivanovo region ), " Maltinsky " ( Irkutsk region ) " Zvenigorod " ( Moscow region ), Svetlogorsk central military sanatorium ( Kaliningrad region ), " Nizhne-Ivkino " ( Kirov region ), " Seregovo " ( Komi Republic ), sanatorium named after A.P. Borodin ( Kostroma region ), “ Krasnoyarsk Zagorye ” ( Krasnoyarsk Territory ), “ Alatyr ” ( Mordovia ) and many other sanatoriums of the Russian Federation.
Diagnostics and therapy
As a rule, the diagnosis of such a disease is made based on the patient’s medical history and external manifestations. In the case of Zakharchenko syndrome, the result is obvious. In addition to examining and interviewing the patient, the doctor must conduct a number of clinical and instrumental tests to exclude other diseases with similar symptoms, including the following:
- MRI of the brain;
- Doppleroscopy of the cervical spine;
- CT head;
- clinical blood test;
- a series of neurological tests.
Confirming the presence of Jacksonian epilepsy in a patient is extremely difficult, since its clinical picture is similar to other disorders. For example, with the myoclonic form of the disease and hysterical seizures. Therefore, during the diagnosis, the neurologist first examines the patient’s medical history, listens to his complaints, and only then sends him for a full examination of the body.
The patient, in addition to standard tests, needs to undergo electroencephalography. Using this diagnostic method, discharges of epileptic activity are detected. Additionally, MRI of the brain is prescribed to differentiate Jacksonian epilepsy from other pathologies (tumors, abscess, encephalitis).
If you suspect Jacksonian epilepsy, a person should consult a neurologist. He will listen to the patient's complaints and then refer him for examinations. People are required to undergo echoencephalography, MRI and CT scans, as well as blood tests. Based on the results of the research, it will be approximately clear what exactly we are dealing with.
For a complete cure, it is recommended to perform neurosurgical intervention, the purpose of which is to remove the pathological focus. If the restoration of nerve tissue is successful, then the symptoms will gradually subside. In this case, you will have to carry out maintenance therapy in order to achieve recovery faster.
If characteristic symptoms appear, a person must immediately consult a doctor and undergo an examination. Even with the help of medications, you can significantly improve your well-being. With the correct selection of medications, the manifestations of the disease will not only not intensify, but will also be significantly weakened.
Nothnagel syndrome (syn. quadrigeminal syndrome)
The syndrome occurs with extensive lesions of the midbrain involving the roof, tegmentum and partly the base of the brain - the quadrigeminal plate is affected; red nuclei or superior cerebellar peduncles, nuclei of the oculomotor nerves, medial geniculate bodies, central gray matter in the circumference of the aqueduct of Sylvius.
The main cause of the pathological process is pituitary tumors. Clinical signs and symptoms. At the onset of the disease, signs of cerebellar damage appear: ataxia, intention tremor, choreiform or athetoid hyperkinesis; There is a decrease in hearing on both sides or only on the side opposite to the localization of the lesion.
https://www.youtube.com/watch?v=ytoSdJfFgpg
In some cases, spastic paresis of the limbs develops. Due to bilateral pyramidal lesions, central paresis of the facial and hypoglossal nerves occurs. Eye symptoms are caused by damage to the oculomotor nerves. Bilateral ophthalmoplegia, mydriasis, and ptosis are observed. In the case of a unilateral lesion, the symptoms are more pronounced on the side opposite the lesion.
Wallenberg (–Zakharchenko) syndrome
One of the alternating medullary syndromes of the brainstem. It was first described by the German physician Adolf Wallenberg in 1895. (Wallenberg A. Acute Bulbäraffection (Embolie der Art. cerebellar. post. inf. sinistr.?) // Archiv für Psychiatrie und Nervenkrankheiten. – 1895. – Bd.27. – S.504-540). Domestic neurologist M.A. Zakharchenko in 1911 described several clinical variants of the syndrome. Occurs with lesions of the posterolateral part of the tegmentum of the medulla oblongata. In this case, the process involves the double nucleus (IX, X nerves), the nucleus of the spinal tract (V nerve), sympathetic fibers from the ciliospinal center of Budge, the medial lemniscus, the inferior cerebellar peduncle (cordite body), the vestibular nuclei (VIII nerve) and other structures . The classic version of the syndrome is described in detail below.
Transverse section of the brain stem at the level of the medulla oblongata. The affected area in classic Wallenberg-Zakharchenko syndrome is shaded (source: www.medsch.wisc.edu/anatomy/bs97/text/bs/contents.htm, in its own modification)
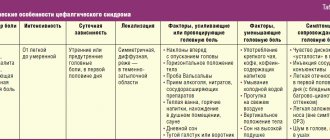
Substrate of lesion and clinical symptoms:
| Structure involved | Ipsilateral | Contralateral |
| Nuclei of IX and X pairs of cranial nerves | Peripheral paresis of the muscles of the pharynx, soft palate and vocal cord (clinically – dysphagia, complete in the first hours; sometimes dysarthria, dysphonia). | |
| Nucleus of the spinal tract of the trigeminal nerve (V pair) | Dissociated hemianesthesia (analgesia, thermoanesthesia) on the face according to the “onion” type, most often in the outer Zölder zone* | |
| Connections between the Budge ciliospinal center and the hypothalamus | Bernard-Horner syndrome:
| |
| Inferior cerebellar peduncle (corpus filamentum) | Cerebellar symptoms: intention tremor, hemiatonia, hemiasynergia, lateropulsion, nystagmus. | |
| Medial loop | Dissociated hemihypesthesia of superficial sensitivity |
* Can be observed on both sides, less often - sensitivity on the face is not impaired.
The syndrome develops acutely, less often – subacutely. The first symptoms are vomiting, dizziness, nystagmus, staggering and even falling towards the affected side. As a rule, patients report severe headache on the affected side.
Among the variants of Wallenberg-Zakharchenko syndrome, the addition of disorders of vital functions (involvement of the reticular formation), damage to the VI and VII, XII nerves, cross paralysis, etc. is noted. Opalski's syndrome is considered separately when ischemia spreads below the level of the pyramidal decussation with the addition of ipsilateral hemiplegia to the lateral bulbar syndrome (Opalski A. Un nouveau syndrome sous-bulbaire: syndrome partiel de l'artère vertébro-spinale postérieur // Paris. Med., 1946. - Vol.1 – P.214-220).
The most common cause of the syndrome is thrombosis of the posterior inferior cerebellar artery (a branch of the vertebral artery) and circulatory failure in the vertebrobasilar region.