Concussion is the most common pathological condition among the consequences of traumatic effects on the skull and brain tissue. This pathology is considered a relatively mild and reversible disorder of brain function, however, insufficient diagnosis of the consequences of injury can cause severe disturbances in its further activity.
In this regard, MRI for concussion, which is performed painlessly and does not pose a risk to the patient’s health, serves as a reliable technique that allows us to fully assess the traumatic consequences.
Physiological manifestations of concussion
Pathology arises, as mentioned earlier, as a result of trauma, which can be of a different nature and affect any part of the patient’s skull. In this case, a lightning-fast increase in intracranial pressure develops, which is considered a direct etiological factor causing further functional disorders - loss of intercellular connections of brain structures, disruption of cellular nutrition, physicochemical transformations.
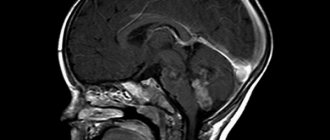
After a concussion, MRI is also performed to identify more serious consequences, including rupture of intracranial vessels and irreversible traumatic changes in areas of the brain. It is this type of research that is most informative regarding morphological and structural changes.
Types of concussion
Contusion has various consequences, based on which the lesion is divided into degrees of severity. When classifying, the clinical picture is also taken into account; symptoms can only be general cerebral or supplemented by focal ones.
Classification:
- The degree is easy. There is no threat to life. A mild form of concussion is characterized by a symptom in the form of loss of consciousness, but the loss of consciousness is short-term. When the victim comes to his senses, he has amnesia, and the fragment of receiving the blow and the circumstances falls out of his memory. There is a headache, sound perception is impaired (there is noise, the interlocutor’s speech sounds muffled or distant). During the initial examination, signs of tachycardia are recorded. Short-term memory is restored after a few days, other symptoms may persist for up to 1 month;
- Degree – average. Consciousness is absent for a long period of time (up to 5 hours). After assessing the neurological status, disturbances are revealed - lethargy, “floating” pupils, disorientation in space. The headache is accompanied by uncontrollable vomiting. The emotional sphere and memory are restored after a few days, other clinical manifestations persist for up to 2 months. As a result of secondary complications from the explosion (mechanical trauma to the skull) and the severity of the damage, after rehabilitation there is a complete or partial restoration of lost functions;
- The degree is difficult. The victim's life is at risk. There is no consciousness - coma for up to 3 weeks or more. Damage to the central nervous system is associated with severe traumatic brain injury (secondary). All organs are damaged - analyzers and vital nerve centers (vascular and respiratory).
A brain contusion often leads to damage to the integrity of blood vessels, resulting in the formation of an accumulation of blood (hematoma) and saturation of surrounding tissues.
Symptoms
The symptoms of a concussion are pronounced and characteristic. In the first minutes after injury, the following clinical picture develops:
- vomit;
- pronounced increase in breathing;
- disturbances in the rhythm of the pulse (slowing or, on the contrary, increasing);
- partial or complete loss of memories of immediate events preceding the injury.
Most often, the patient’s recovery period is not accompanied by deviations from the norm in body temperature and blood pressure, but the following characteristic symptom complex of the rehabilitation period is observed:
- severe, varied headaches;
- dizziness;
- nausea;
- general weakness;
- inhibition of cognitive processes;
- noise in ears;
- sweating
It should be noted that all of the above symptoms are characteristic exclusively for patients of the young and middle age groups, while newborns and elderly people demonstrate a slightly different clinical picture. The fundamental difference here is the absence of a symptom of loss of consciousness.
After injury, young children exhibit frequent regurgitation, weakness and drowsiness, while older people report impaired coordination of movements and disorders of mental activity, including memory. Due to the uncharacteristic clinical picture and the vulnerability of the body, patients in this age group first of all need tomography for a concussion.
How can you spot the signs of a brain contusion?
Sometimes a bruise may form on the opposite side of the impact site. But in any case, its symptoms appear immediately after injury and progress progressively. Symptoms of a brain contusion include:
- Loss of consciousness, which can be of varying duration - several minutes or last for more than one week. If the injury was inflicted without witnesses, then a short loss of consciousness may not be noticed.
- The onset of amnesia is of the retrograde type. People cannot remember events that happened to them before the injury.
- I have a constant headache and dizziness.
- Nausea, which inevitably progresses to vomiting.
If the first signs occur, you must immediately contact a medical facility. Where victims will immediately undergo all necessary examinations and diagnostics (including MRI) and begin qualified treatment. Otherwise, complications may arise, which are expressed in the following:
- Consciousness changes. Traumatized people begin to make rude jokes and treat friends and family with indifference. If the injury was inflicted on the temporal lobes, the victims may become aggressive.
- Loss of vision for some time, split silhouettes, photophobia.
- The pupils dilate.
- Speech becomes unclear and patients have difficulty speaking.
- Hearing decreases.
- The breathing rhythm changes and blood pressure rises.
- A person ceases to feel some parts of the body and involuntarily urinates.
- Fluid mixed with blood may be discharged from the nose and ears.
- Paralysis and coma.
Treatment for brain contusions varies. It depends on the severity of the injury. The more severe it is, the longer the treatment. But if a person who has received one or another head injury is taken to the hospital on time, the greater his chances of a faster recovery.
Does an MRI show a concussion?
Since a concussion is usually not accompanied by morphological disorders, conducting research is most important in order to exclude the development of complications. It is worth conducting an MRI in case of a concussion first of all to exclude a dangerous pathology - brain contusion. Doctors recommend resorting to this technique in case of danger of intracranial hemorrhages, severe traumatic brain injuries and ischemic conditions. Due to the fact that the magnetic resonance imaging technique is extremely informative, it is always useful to conduct an MRI if the patient has hit his head.
The examination will take about 15 minutes, during which the patient remains under the influence of the electromagnetic field of the tomograph - it is completely safe and painless. At this time, the doctor receives three-dimensional images of the skull bones and brain tissue.
The feasibility of MRI for head injuries has been confirmed by leading world research and is explained by the information content of this modern diagnostic method.
What is cerebral contusion
The term contusion, or translated from Latin bruise, is used in the medical lexicon to describe a special type of brain damage. The condition is always accompanied by a loss of consciousness; the duration depends on the strength of the impact on the brain matter and the severity of the damage.
More often it occurs as a result of a pressure surge after an explosion. The effect of a shock wave on the brain is compared to a sudden powerful blow to the head. But with a concussion, there is no mechanical impact on the skull; if there are injuries to the head, then they are already of a secondary and tertiary nature (a fall after a wave, exposure to fragments from an explosive).
Contusions of the brain and eyes are also often diagnosed as a combined pathology. But the eyeball, unlike the brain, is affected by a mechanical factor (impact) or a secondary contusion occurs. That is, the impact occurs when the whole body is shaken, for example during a fall.
In the medical literature there is still no clear opinion in which cases to diagnose a concussion instead of a bruise. The only thing scientists agreed on was that these were completely different brain injuries. But all internal lesions: bruises, concussions are the result of a blow, direct or indirect, and they belong to a closed craniocerebral injury.
Despite several levels of brain protection from various damages (skull, membranes, cerebrospinal fluid), it remains extremely vulnerable. So what is the difference between a concussion and a bruise? In the first case, the brain is subjected to direct physical or mechanical impact, after which the damage to the brain substance is not narrowly localized - scattered, organic disorders do not occur.
With concussion, the force of the wave moving through the air has incredible strength and speed. The action of this force has a narrow focus in relation to the brain, that is, a certain area of damage. But there is also a general effect - after the shock wave, a brain shake occurs. An internal bruise after a contusion occurs on an inert frame; the force of the impact leads to a displacement of structures and the development of pathological symptoms.
Loss of consciousness, unlike a concussion, is longer lasting, and the clinical picture is more serious. But it is worth noting that contusion as an independent diagnosis occurs in 20–30% of cases. In other cases, it is a combined diagnosis (bruise together with a concussion) or concussion.
Contusion (bruise) of the brain
Contusion (bruise) of the brain is a severe form of brain damage, which differs from concussion by macroscopically detectable damage to the brain matter of varying degrees (from small areas of blood soaking of the brain matter to crushing and necrosis of parts of the brain). Most often, the foci of bruise are localized at the site of impact and counter-impact. This type of injury combines both reversible and irreversible morphological changes caused by damage and death of individual areas of the brain.
A contusion (contusion) of the brain is characterized by focal symptoms - paralysis, speech impairment, hearing, vision, etc. Loss of consciousness usually occurs immediately after injury; the duration of the period of impaired consciousness depends on the severity of the brain contusion. Sometimes loss of consciousness does not occur immediately after the injury and gradually deepens, reaching the degree of stupor or coma due to the deterioration of the general condition of the affected person or the development of complications in the brain (cerebral hypertension, edema - swelling, hematoma, pneumocephalus). A comatose state reflects the highest severity of brain injury (especially its brain stem) and can be expressed to varying degrees. Along with impaired consciousness and focal symptoms, brain contusion is characterized by blood in the cerebrospinal fluid and skull fractures. When making a diagnosis, three (3) degrees of brain contusion are distinguished - mild, moderate and severe.
A mild cerebral contusion is characterized by a short loss (20–25 minutes) or some stupor of consciousness, a satisfactory general condition, and the presence of focal symptoms of damage to the nervous system. The period of severity of general cerebral symptoms lasts no more than 2–3 days, and focal symptoms (minor paresis of the limbs or reflex asymmetry) last up to 2–3 weeks. Such disorders are often found in people admitted to the hospital in a state of severe alcohol intoxication. Brain contusion should also include cases where there is a skull fracture (crack, depression).
Moderate brain contusions are characterized in the acute period of injury, primarily by pronounced cerebral symptoms. Loss of consciousness often lasts 1–3 hours, followed by somnolence or stupor. When consciousness clears, distinct focal symptoms are revealed in the form of paresis or paralysis of the limbs, speech and hearing disorders, and narrowing of visual fields. These symptoms suggest the localization of the contusion in a certain lobe of the brain or in its basal parts, both at the site of injury and on the opposite side (like a counter-impact).
Severe brain contusion is characterized by a prolonged loss of consciousness, which in favorable cases turns into a drowsy (somnolent) state, and in severe cases - stupor, deepening the coma. In case of severe brain contusion, not only the cortical areas of the brain on its convex side are affected, but also the basal sections, as well as subcortical formations or various areas of the brain stem (diencephalic, mesencephalic-bulbar, etc.). In these cases, there are violations of vital functions - breathing, cardiovascular, swallowing, adaptation-trophic, metabolism. These disorders may occur immediately after the injury or develop some time after it. Lesions of the subcortical and stem parts of the brain often manifest themselves in rather characteristic symptom complexes, mainly diencephalic and mesencephalobulbar.
Clinical manifestations. Loss of consciousness after injury lasts up to 1–2 hours, in severe cases - more than a day. In the initial period after injury, verbal contact is possible (may be difficult). Headache. Tinnitus. Vomiting soon after injury, sometimes repeated. Involuntary loss of urine. Motor (psychomotor) agitation or, conversely, retardation. Cramps. Slow heart rate (bradycardia).
First aid. Place the victim on a stretcher on his side or face down, placing a soft mat under his head. Cold on the head. Remove vomit from the mouth with a finger wrapped in a handkerchief or gauze pad. For headaches, take painkillers (the use of drugs is contraindicated). Careful transportation on a stretcher in a lateral or face down position (to prevent aspiration of vomit and mucus) to the neurosurgical (surgical, trauma) department. It is possible to carry the affected person in the arms: by one person using the “hands in front of you” or “on the shoulder” method; by two bearers - according to the “one after another” method (if the victim is unconscious) or “locked” from 2, 3, 4 hands.
Sources: Closed injuries of the central nervous system // Nervous diseases: Textbook / Edited by A. Akimov. – L., 1982; Injuries of the skull and brain // Military field surgery / Edited by P.G. Bryusova, E.A. Nechaeva. – M., 1996.
What brain diseases are visible on MRI?
A set of symptoms for which magnetic resonance imaging of the head is prescribed:
- Decreased breathing;
- Vomiting reflex;
- Loss of vision, speech;
- Unsteadiness of gait due to damage to the cerebellum;
- Twitching pupils;
- Strabismus;
- Lack of swallowing reflex;
- Difficulty in excreting feces;
- Periodic loss of consciousness;
- Frequent headaches.
The described clinical manifestations may be a consequence of brain contusion, traumatic brain injury, stroke, or severe head impacts.
The advent of MRI scanning made it possible to diagnose pathological changes in multiple sclerosis (destruction of the myelin sheaths of the nerves). After a bruise, headaches appear at a late stage, when pronounced microcirculation disorders occur. Contacts at the sites of destruction of nerve fibers cause a “short circuit” with subsequent neurological symptoms. Extensive disruption of nerve innervation is accompanied by vasoconstriction. Abnormal microcirculation provokes headaches, muscle disorders, visual and auditory disorders.