Every person has pauses in breathing, even those who confidently deny them - at least once in their life. Are they dangerous? It all depends on the frequency and duration of the phenomenon, as well as on his lifestyle and much more. What to do if you feel like your breathing stops when you fall asleep? How do you know if this is normal or if it’s time to see a doctor? What can and should you do yourself? What can sleep apnea lead to (this is what the phenomenon of stopping breathing during sleep is called) if it is not treated? I will answer these and other questions today.
Good afternoon, dear reader!
Breathing is life, and the slightest problems in respiratory activity can cause a significant deterioration in the quality of life. Sleep apnea is one such phenomenon.
First, let's look at the reasons.
How to cope with anxiety and fear caused by sleep apnea?
One woman told me that it was not the sudden stops in breathing at night that frightened her (she often woke up because of this).
What frightened her most was the state of extreme anxiety and fear, the feeling that her heart was squeezing, as if her chest was being squeezed from several sides.
I am sure that she was not the only one who woke up from respiratory arrest and felt these unpleasant emotions of anxiety and worry.
Such emotions are not only unpleasant, they are also extremely harmful for a person at such a moment. The thing is that anxiety contributes to a strong heartbeat, which, in turn, increases the body’s need for oxygen.
As you understand, a person suffering from sleep apnea should not panic (although sometimes this is extremely difficult). It is iron calm that can facilitate the treatment of sleep apnea.
My online training “How to cope with stress, turning it from a monster into a helper” will help you develop such calmness and increase stress resistance. The training is written in such a way that completing each task will make you look differently at the surrounding reality and finally understand the true reasons for your experiences.
Well, we're a little distracted. Let's return to today's topic - what to do if breathing stops while falling asleep?
How to determine when the body can cope on its own, and when consultation with a specialist is necessary?
Diagnosis and treatment of sleep disorders
Sleep is a vital need for the body, more important than food. In the figurative expression of P. Buast: “A dream is a magic lantern, in the light of which one can see with closed eyes everything that life has in itself that is wonderful.” It is a genetically determined state of the body, characterized by a natural sequential change of certain printing patterns in the form of cycles, phases and stages. The amount of sleep is one of the main components of the concept of “quality of life.” Thus, sleep affects a person’s health and well-being no less than the period of wakefulness. The longest period of wakefulness lasted 18 days, 21 hours and 40 minutes. The record was recorded at a competition for sitting in a rocking chair. The winner paid for his achievement with hallucinations, speech and vision disorders, and memory loss.
The average sleep requirement of an adult is 7–8 hours per day. Albert Einstein wrote: “I spend a third of my life sleeping, and not the worst.” But changes are possible within a fairly wide range (4–10 hours). Sleep plays an important role in metabolic processes (in particular, growth hormone is released during sleep), promotes the processing and storage of information, adapts the body to changes in light (day-night) and restores immunity (by activating T-lymphocytes). Miguel de Cervantes in his novel “Don Quixote” describes the functions of sleep as follows: “...blessed is our Lord, who invented sleep: it is a cloak that covers a traveler in the night, it is food for the hungry, a sip of water for the thirsty, warm for the cold.”
Sleep is a heterogeneous process. It represents a sequence of functional states of the brain - the phase of slow sleep (orthodox sleep, dreamless sleep) and the phase of rapid sleep (paradoxical sleep, sleep with dreams, or REM phase). A normal 8-hour sleep consists of 4-6 wave-like cycles, each lasting about 90 minutes. In general, during the night, the slow-wave sleep phase takes up 75–85% of the total sleep time, and the REM sleep phase takes up only 15–25%.
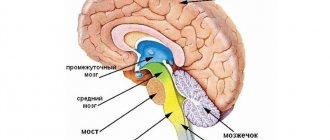
There are 4 stages of slow-wave sleep. The first stage (drowsiness) is characterized by the absence of alpha rhythm on the electroencephalogram (EEG), which is a characteristic sign of human wakefulness. The second stage is characterized by ri (sigma rhythm) with a frequency of 13–16 per second and registration of K-complexes. The third stage is characterized by the appearance on the EEG of slow rhythms in the delta range (delta activity takes up from 20% to 50% of the stage time). At the same time, “sleep spindles” continue to appear quite often. The fourth stage is characterized by registration on the EEG of a high-amplitude slow delta rhythm (delta activity occupies more than 50% of the stage time). The third and fourth stages of slow-wave sleep constitute what is called delta sleep. With slow-wave sleep, there is a decrease in breathing rate and heart rate, muscle relaxation and slow eye movement (the predominance of the parasympathetic nervous system). As slow-wave sleep deepens, the total number of movements of the sleeping person becomes minimal. At this time it is difficult to wake him up. When awakening during slow-wave sleep, a person usually does not remember dreams. The slow-wave sleep phase is maximally represented in the first half of the night. The main function of the slow-wave sleep phase is anabolic.
The REM sleep phase is characterized by a low-amplitude EEG rhythm, and in the frequency range by the presence of both slow and higher-frequency rhythms (alpha and beta rhythms). Characteristic signs of this phase of sleep are the so-called sawtooth discharges with a frequency of 4–6 per second. During REM sleep, physiological functions, on the contrary, are activated (the sympathetic nervous system predominates), which is manifested by increased breathing and heart rate, increased motor activity of the sleeper (the development of a “vegetative storm”). In this case, the movement of the eyeballs becomes rapid (the sleeper is dreaming). If you wake him up 10-15 minutes after the end of rapid eye movements, he will talk about the dream he had. Dreams are figurative representations, often emotionally charged, that arise during sleep and are subjectively perceived as reality.
Dreams are explained by the fact that during sleep, not the entire cortex is inhibited - some of its areas continue to remain excited and create certain sensations. The most important function of dreams is psychological protection. Herodotus wrote: “Usually people see in their dreams what they think about during the day.” The REM sleep phase is maximally present in the morning hours. The main function of the REM sleep phase is to process information and create a behavior program. For example, everyone knows that Dmitry Mendeleev dreamed of the Periodic Table of Chemical Elements (this happened during the REM sleep phase). The periods of sleep and wakefulness in humans alternate with circadian periodicity. The body's circadian period is usually close to 24 hours. The hormone that regulates the body's circadian activity is melatonin, which is produced in the pineal gland.
Almost every person has had an episode of sleep disturbances at least once in their life. According to a number of researchers, up to 45% of the adult population suffers from sleep disorders. At the same time, the number of people with short sleep duration (less than 6 hours) increases with age. A study in California found that people who slept 6 hours or less per night had a higher mortality rate than those who slept 7 to 8 hours. In the United States, direct and indirect costs associated with sleep disorders are estimated at approximately $100 billion annually.
Insomnia (previously called insomnia) is a recurrent disturbance in the initiation, duration, consolidation or quality of sleep that occurs despite the availability of sufficient time and conditions for sleep and is manifested by disturbances of various types of daytime activities. In the figurative expression of O. Muravyova: “Insomnia is contemplation of the stars in the depths of your soul at night.” Most often, insomnia is caused by stress, neuroses, mental, neurological, somatic diseases, pain phenomena, as well as various external unfavorable conditions. The most important clinical signs of insomnia are: complaints of difficulty falling asleep and poor quality of sleep, sleep disturbances at least three times a week for a month, preoccupation with insomnia and its consequences (both at night and during the day) and caused by unsatisfactory duration and/or quality of sleep. sleep, severe illness or impairment of social and occupational functioning.
According to the modern classification, there are situational insomnia (duration up to 1 week), acute insomnia (duration less than 3 weeks) and chronic insomnia (duration more than 3 weeks). Chronicization of insomnia is facilitated by persistent stress, depression, anxiety, prolonged course of the disease that caused insomnia, and long-term use of “long-lived” benzodiazepines. In the clinical picture of insomnia, presomnic, intrasomnic and postsomnic disorders are distinguished:
1. Presomnia disorders:
- difficulty initiating sleep;
- the process of falling asleep can take up to 2 hours or more (normally an average of 10 minutes);
- over a long period of time, pathological “bedtime rituals” may develop, as well as “fear of bed” and fear of “not getting sleep”;
- Patients often ignore falling asleep, and all this time appears to them as continuous wakefulness.
2. Intrasomnic disorders:
- frequent awakenings at night, after which the patient cannot fall asleep for a long time, and sensations of “shallow” sleep;
- awakenings are caused by both external (for example, noise) and internal factors (fearful dreams, increased motor activity, the urge to urinate);
- The threshold for awakening is sharply reduced and the process of falling asleep after an episode of awakening is difficult.
3. Postsomnia disorders;
- disorders that occur in the immediate period after awakening;
- patients are not satisfied with sleep;
- feeling of “being overwhelmed”, non-imperative daytime sleepiness;
- sometimes patients complain of a complete lack of sleep for many nights (the relationship between subjective assessments of sleep and its objective characteristics is ambiguous).
B presents the incidence of insomnia in various neurological diseases.
Sleep and dementia
Currently, there are 46,772,524 elderly people living in Russia. Among geriatric problems, sleep disorders are the most important. According to a number of epidemiological studies, from 25% to 48% of people over 65 years of age experience a variety of sleep disorders. The main manifestations of sleep disturbance in older people are persistent complaints of insomnia, constant difficulties falling asleep, shallow and intermittent sleep, the presence of vivid, multiple dreams (often painful content), early awakenings, a feeling of anxious restlessness upon awakening, difficulty or inability to fall asleep again and lack of sensation. rest from sleep. Moreover, among the forms of insomnia, presomnia disorders account for 70%, intrasomnia disorders - 60.3%, and post-somnia disorders - 32.1%. With aging, the total duration of sleep decreases, the duration of the superficial stages increases, as well as the time of falling asleep and being awake within sleep. As a result, older adults take longer to fall asleep and reach the restful stage of deep sleep. With such a sleep structure, there may be complaints like “I didn’t sleep a wink all night.” If such people are accidentally awakened, they may not fall asleep for a long time. The age-related increase in time spent awake during the night and the deterioration in the quality of nighttime sleep respectively cause daytime sleepiness and the need for sleep during the day.
Of particular interest is sleep disturbance in patients with dementia. Dementia is understood as a diffuse impairment of mental functions as a result of organic brain damage, manifested by primary disorders of thinking and memory and secondary emotional and behavioral disorders. In patients with dementia, sleep disorders are caused by a disturbance in the circadian rhythm in the form of sleep inversion with wakefulness at night and drowsiness during the day. Disruption of the circadian rhythm is accompanied by disorientation, restless behavior, fussiness, “getting ready for the road,” tying knots from bed linen, taking things out of closets, etc., i.e., manifestations of behavioral disorders. However, sleep disturbance itself can cause dementia. Thus, researchers from the University of Washington have identified a connection between sleep and dementia. As a result of experiments, it turned out that during sleep the concentration of amyloid protein decreases. According to scientists, the content of amyloid protein may be associated with brain activity, which is higher during wakefulness. It is most dangerous in middle age, when plaque in the brain has already begun to form, but symptoms of the disease will not appear until several years later, so scientists recommend that people get more sleep, especially in middle age.
Sleep and depression
Depression (from Latin? - suppression) is characterized by a pathologically low mood (hypotymia) with a negative, pessimistic assessment of oneself, one’s position in the surrounding reality and one’s future. In the figurative expression of Miguel de Cervantes: “Sleep is the best medicine for waking troubles.” Sleep disorders are an obligatory symptom of depression, which is explained by general neurochemical processes. Thus, disruption of the mediation of serotonin and melatonin, on the one hand, plays a crucial role in the development of depression, and on the other, is of great importance in the organization of sleep. Features of sleep disorders in depression are sleep disturbances, which reach 100% of cases (manifest in the form of insomnia and inversion of the sleep-wake cycle), they can precede the appearance of affective disorders themselves (be the only symptom of depression) and persist after the disappearance of clinical signs of depressive states . Often in depression, the relationship between subjective assessments of sleep and its objective characteristics is ambiguous. Quite often, patients complain of a complete lack of sleep for many nights. However, upon objective examination, sleep is not only present, but its duration exceeds 5 hours (distorted sleep perception, or “sleep agnosia”). Depression is associated with a risk of suicide. Of the approximately 1 million suicides committed annually, up to 50% occur in patients suffering from depression. In Russia, the number of suicides is 36–38 cases per 100 thousand population (in the world the same figure is 14.5). The critical level of suicide rate, established by WHO, is 20 per 100 thousand people. Chronic sleep problems increase the risk of suicide by 2.6 times. This conclusion was reached by American scientists from the University of Michigan. The greatest danger is faced by those who wake up much earlier than the alarm clock.
Sleep and stroke
Stroke (translated from Latin as “stroke”) is one of the most severe forms of vascular lesions of the brain. According to Ya.?I.?Levin et al. (2008), 45% of strokes develop in the morning, 32% during the day, and 23% during night sleep. Moreover, the first few hours after waking up are especially dangerous in terms of stroke. The most severe sleep disorders are caused by hemorrhagic strokes and the maximum proximity of the lesion to the median structures. In the formation of structural changes in sleep, in addition to the main cause (stroke), a large contribution is also made by the initial feature of the regulation of the sleep-wake cycle. Sleep disturbances in cerebral stroke manifest themselves in the form of insomnia, disruption of the sleep-wake cycle, and sleep breathing disorders such as sleep apnea syndrome. Insomnia in patients who have suffered a stroke is characterized by changes in sleep duration, frequent night awakenings and lack of satisfaction with night sleep, which primarily affects the quality of life. As the results of our studies showed (S.?P.?Markin et al., 2009), in stroke patients suffering from insomnia, the index of general mental well-being was only 43.5 ± 4.0 points (with a maximum value of 110 points) , which corresponds to 39.6% of the norm.
Speaking about the ability of the brain to recover after a stroke, it is necessary to note the role of plasticity. Plasticity is the ability of nervous tissue to change its structural and functional organization under the influence of endogenous and exogenous factors. In itself, acute brain damage is a powerful factor that activates plasticity processes. However, the morphological and functional outcome also largely depends on the severity of sleep disorders. So, according to Ya.?I.?Levin et al. (2008), changes in sleep structure in the acute period of stroke have important prognostic significance. It has been proven that the survival rate of patients in whom all stages of sleep are represented is 89%. In the absence of the ability to identify sleep stages, the fatal outcome is 100%. As a result, during the rehabilitation treatment of patients who have suffered a stroke, it is necessary to pay great attention to sleep disturbances.
Sleep and pain
The International Association for the Study of Pain defines it as an unpleasant sensory and emotional state caused by actual or potential tissue damage. In the United States, according to a telephone survey of the population over 18 years of age, it was found that about 94 million people complain of night pain. The results of one study showed that the pain-sleep relationship is bidirectional (the patient is in a vicious circle: increasing pain leads to insomnia, and insomnia in turn increases pain). Moreover, in 55% of cases at night people are bothered by headaches (primarily migraines).
Migraine is considered a chronic disease caused by hereditarily determined dysfunction of vasomotor regulation, manifested by relatively stereotypical paroxysmal attacks of severe headache. The inheritance of a certain neurochemical defect (insufficient metabolism of brain monoamines, especially serotonin) plays an important role in the occurrence of migraine. The comorbidity of migraine and sleep disorders is explained, first of all, by common pathogenetic mechanisms: serotonin is involved in the formation of the sleep-wake cycle and is one of the most important neurotransmitters of pain (the level of which varies depending on the phase of the migraine attack). Migraine in the sleep-wake cycle is more severe, accompanied by autonomic disorders during sleep (with elements of panic attacks), increased motor activity during sleep, high levels of anxiety and depression, as well as a significant decrease in quality of life. At the same time, the most important provoking factor in the development of sleep migraines is lack of night sleep.
Sleep and parkinsonism
Parkinsonism comprises three groups of diseases (McDowel et al., 1998): Parkinson's disease (idiopathic parkinsonism), symptomatic parkinsonism and parkinsonism plus. Parkinsonism formula P = G ± P ± T ± PN/NH, where P is parkinsonism, G is hypokinesia, P is rigidity, T is tremor, PN is postural instability, NH is gait disturbance. However, recently more attention has been paid to the so-called non-motor manifestations of Parkinson's disease, namely autonomic disorders, affective (anxiety), psychotic disorders (nightmares, hallucinations, illusions and psychomotor agitation during sleep), as well as sleep disorders. Sleep disorders in parkinsonism are divided into “nonspecific”, which are manifested by insomnia (more than 60%), inversion of the sleep-wake cycle (daytime sleepiness in 30%) and sleep apnea syndrome, as well as “specific” (as a result of a defect in dopamine systems and complications of therapy) in the form of motor disorders at night (hypokinesia, muscle rigidity, restless legs syndrome, myoclonus, behavioral disorders in the REM sleep phase (15–19%)).
Diagnosis of sleep disorders
Diagnostic measures for insomnia should include an assessment of a person’s individual chronobiological stereotype, his professional activity, a certain clinical picture, the results of a psychological study (Spielberger test (anxiety assessment), CES-D scale (depression assessment), a subjective sleep assessment questionnaire (somnology center of the Ministry of Health of the Russian Federation) , a questionnaire for screening sleep apnea syndrome), the results of a polysomnographic study and support for insomnia.
Polysomnography is a method of parallel recording of various physiological indicators during sleep. In this case, the electroencephalogram, electrooculogram and electromyogram are of greatest importance. The combined assessment of these three indicators allows us to determine at any time what stage of sleep the patient is in. Based on the results of the sleep recording, a hypnogram () is constructed.
Analysis of the hypnogram makes it possible to determine whether the patient’s sleep indicators correspond to the normative ones and what specific phenomena occur during sleep and may be the cause of its disturbance.
Modern approaches to the treatment of insomnia
Currently, in the treatment of insomnia, both non-medicinal (sleep hygiene, psychotherapy, physiotherapy, phototherapy, encephalophonia) and medicinal treatment methods are used. At the same time, it is very important to maintain sleep hygiene, which includes the need to go to bed and get up at the same time, eliminate daytime naps (especially in the afternoon), do not drink tea or coffee at night, reduce stressful situations, mental stress (especially in evening time), organize physical activity in the evening (but no later than 3 hours before bedtime) and regularly use water procedures before bedtime. Galibert wrote: “Taking worries into bed with you means sleeping with a bundle on your back.”
Currently, there are three generations of hypnotics: an ethanolamine derivative (Donormil), benzodiazepines and non-benzodiazepine hypnotics (a derivative of cyclopyrrolones and imidazopyridine). The basic principles of drug therapy are the administration of low effective doses, selection of a drug with optimal pharmacokinetic properties, intermittent therapy (2-3 times a week), short-term use of drugs (3-4 weeks) and gradual withdrawal of hypnotics.
Donormil (doxylamine) (H1-histamine receptor antagonist) is widely used in the treatment of insomnia. A feature of Donormil's action is the absence of a direct effect on somnogenic structures; its effect is carried out at the level of waking systems by inhibiting their activity. A fundamentally different mechanism of hypnotic action (compared to traditional hypnotics) allows it to be used more widely when changing one drug to another, reducing the dosage of “habitual hypnotics,” as well as when it is necessary to discontinue hypnotics.
Comparison of the effectiveness of Donormil and hypnotics of other groups
- The effectiveness and tolerability of Donormil and benzodiazepines were compared (Ya.?I.?Levin et al., 2008). Donormil is comparable in effectiveness to benzodiazepines. However, when using Donormil, there were no side effects characteristic of benzodiazepines, such as the development of dependence, withdrawal syndrome, and possible increased manifestations of sleep apnea syndrome. In addition, in elderly patients treated with benzodiazepines, excessive sedation, muscle relaxation, balance disorders (falls), attention problems, worsening dysmnestic disorders and drug interactions may additionally be observed (increased hypotensive effect of drugs, depressive effect on the central nervous system when combined with beta blockers, increasing the concentration of cardiac glycosides in the blood serum, enhancing the hypoglycemic effect when combined with antidiabetic drugs, etc.).
- The effectiveness and tolerability of Donormil, zolpidem and placebo in the treatment of insomnia were compared (G.?V.?Kovrov et al., 2008). The study proved the absolute superiority of Donormil over placebo, as well as the comparable effectiveness of Donormil and zolpidem against symptoms of insomnia. Unlike zolpidem, Donormil had no withdrawal symptoms.
- The effectiveness and tolerability of Donormil and zaleplon were compared (S.?P.?Markin et al., 2008). The use of Donormil and zaleplon contributed to rapid falling asleep. However, when using zaleplon, episodes of awakening were observed (due to a short half-life), which required repeated dosing of the drug. Unlike Donormil, zaleplon in some cases caused the development of physical dependence with withdrawal symptoms, even when used in therapeutic doses.
Donormil for sleep disturbances in post-stroke patients (S.?P.?Markin, 2008)
A total of 60 patients aged 54.7 ± 4.9 years who suffered an ischemic stroke 2–3 weeks old were examined. Various sleep disorders were observed in 100% of cases from 4 to 7 times a week. According to the questionnaire (questionnaire for subjective assessment of sleep), before treatment, sleep disturbances (11.9 ± 0.18 points) were identified in 34 people (56.7%) and borderline values of sleep function (19.9 ± 0.17 points) were identified in 26 people (43.3%). On average, the total score was 16.2 ± 0.15 points. Subsequently, patients in the main group took Donormil at a dose of 15 mg (1 tablet) 15–30 minutes before bedtime for 14 days. Patients in the control group received only placebo. As the study results showed, the use of Donormil contributed to a significant improvement in sleep (including sleep in all its characteristics) in patients of the main group (). Thus, the total assessment of sleep quality was 25.2 ± 0.14 points (p < 0.001) compared to the control group, where no significant changes were obtained (16.1 ± 0.16 points (p > 0.05)).
Donormil for sleep disturbances in old age (S.?P.?Markin, 2009)
A total of 59 patients aged 67.5 ± 3.6 years were examined. As shown by the results of neuropsychological testing (the “5 words” test, the Schulte test and the “clock drawing” test), only 17 people (28.8%) had normal test scores. While 42 people (71.2%) had cognitive impairment of varying degrees of severity. At the same time, all patients complained of sleep disturbances 5 to 7 times a week. Thus, according to the subjective sleep assessment questionnaire, sleep disturbances (11.2 ± 0.16 points) were detected in 39 people (66.1%) and borderline values of sleep function (19.8 ± 0.15 points) were detected in 20 people ( 33.9%). On average, the total score was 15.2 ± 0.15 points. Subsequently, all patients (including those with cognitive impairment) took Donormil at a dose of 15 mg (1 tablet) 15–30 minutes before bedtime for 14 days. As the study results showed, the use of Donormil contributed to a significant improvement in sleep (including sleep in all its characteristics) among all patients (). Thus, the total assessment of sleep quality was 25.2 ± 0.14 points (p < 0.001) compared to the initial data. At the same time, in the group of patients with impaired cognitive functions, no deterioration was noted. In addition, when sleep was normalized, there was an improvement in attention in patients, which was confirmed by the results of the Schulte test ().
Literature
- Wayne A.?M. Sleep Medicine / Selected Lectures in Neurology; edited by prof. V.?L.?Golubeva. M.: Eidos Media, 2006. pp. 12–20.
- Wayne A.?M. Sleep medicine: problems and prospects // Collection of clinical lectures “Sleep Medicine: new treatment opportunities.” Journal neurol. and a psychiatrist. them. S. S. Korsakov. 2002. Appendix pp.3–16
- Kovrov G.?V., Vorobyova O.?V. Sleep disturbance: from complaint to diagnosis and treatment // Ros. honey. magazine T. 14. No. 6. 2006. pp. 3–6.
- Kovrov G.?V., Levin Ya.?M. Insomnia and its treatment. The quality of life. Medicine, 2004. No. 4 (7). pp. 54–57.
- Levin Ya.?I. Insomnia/Selected Lectures in Neurology; edited by prof. V.?L.?Golubeva. M.: Eidos Media, 2006. pp. 338–356.
- Levin Ya.?I. Modern therapy of sleep disorders: world and Russian experience // Collection of clinical lectures “Sleep Medicine: New Therapy Opportunities.” Journal neurol. and a psychiatrist. them. S.?S.?Korsakova. 2002. App. pp. 17–27.
- Levin Ya.?I. Doxylamine (Donormil) in the treatment of insomnia // Ros. honey. magazine 2006. T. 14. No. 9. P. 704–709.
- Markin S.?P. Depressive disorders in the clinical picture of cerebral stroke // Ros. honey. magazine 2008. T. 16. No. 26. P. 1753–1757.
- Markin S.?P. The influence of sleep disorders on the effectiveness of rehabilitation treatment of patients who have suffered a stroke // Ros. honey. magazine 2008. T. 16. No. 12. P. 1677–1681.
- Markin S.?P. Treatment of sleep disorders in elderly people with impaired cognitive functions // Consilium medicum. 2009. No. 2. P. 55–60.
- Markin S.?P. Doxylamine and post-stroke sleep disturbances // European Journal of Neurology. 2008. Vol. 15. Sup. 3. P. 209.
- Rachin A.?P. Therapy of sleep disorders: classification and analytical approaches // Handbook of a polyclinic doctor. 2007. No. 6. pp. 64–69.
- Sokolova L.?P., Kislyi N.?D. Sleep disorders in the elderly: features of therapy // Consilium medicum. 2007. T. 9. No. 2. pp. 133–137.
S. P. Markin , Doctor of Medical Sciences
Voronezh State Medical Academy named after. N. N. Burdenko , Voronezh
Contact information about the author for correspondence
Features of the slow phase
There are 4 stages inside it. They all have different bioelectrical characteristics. As a person goes deeper into it, it becomes more and more difficult to wake him up.
To fall asleep, the brain begins to secrete a special substance. It causes lethargy and slows down your metabolism.
Periods
They include: nap, light, moderately deep and deep. The last two are collectively called delta sleep. At this time, specific delta waves are observed.
Signs
The sleeper begins to breathe slowly, his pulse slows down, and his eyes gradually stop moving.
Influence
The body is restored and healed, the body is filled with energy. The body is physically recovering.
Features of the fast phase
Considering what REM sleep is, we can note the increased functioning of the respiratory and cardiovascular systems.
Interesting! During daytime rest, this phase does not occur or does not last very long. This is why a person who has not slept all night cannot fully rest during the day.
Signs
At the stage of REM sleep, muscle tone decreases, the muscles of the mouth and neck are completely immobilized. This period is characterized by active eye movements under the eyelids.
Influence
During this period, the brain processes what it has seen and heard during the day. It adapts to changes in the environment.
When problems with proper rest arise, the psychological defense function is disrupted. A person feels lethargic and irritable throughout the day. He is extremely distracted and constantly wants to cry.
Dreams
It is during this period that the sleeper begins to see vivid, eventful dreams. This is explained by the fact that the part of the cerebral cortex that is responsible for vision and emotions is activated.
Usually dreams have a plot, characters and a lot of experiences.
Alternation of stages
During slow-wave sleep and REM sleep, different functions are performed. Throughout the entire cycle, there are five stages with their own physiological characteristics:
- Stage 1 – takes 4-5% of the time, light sleep, the process of basic actions in the body slows down, blood pressure decreases;
- Stage 2 – 45-55%, there is a decrease in body temperature, slowing of breathing, decreased heart rate;
- Stage 3 – from 4 to 6% of the time, the beginning of deep, sound sleep;
- Stage 4 – 12 – 15%, rhythmic, unhurried breathing is observed;
- Stage 5 – 20 – 25% of the time, a person has calm dreams, the brain relaxes, and the heartbeat quickens.
It takes from 15 to 40 minutes to fall asleep. If this takes 1 hour, then this is a sign of insomnia, which means it is necessary to take measures to eliminate it. The first cycle, that is, alternating slow and fast sleep, takes 1 hour, then the slow phase of another cycle begins again. Each time the sleep will be deeper. In the ratio of fast and slow sleep, the latter remains up to 80% of the total night time.
NREM and REM sleep
After passing through all the cycles, awakening occurs. It usually takes up to 3 minutes. During this time, consciousness is connected.
The alternation of stages does not change in a healthy person. The following factors can disrupt the sequence:
- emotional instability;
- age-related changes;
- prolonged stress, depression;
- mental disorders;
- long-term chronic diseases;
- injuries.
These disorders require treatment, as they can lead to complications. Deficiency of night rest or certain stages leads to the appearance of serious diseases.