Microcephaly is a congenital anomaly, which is characterized by a significant reduction in the size of the brain (and, as a result, the skull) as a result of disruption of the growth processes of brain tissue during the period of intrauterine development of the baby.
It can be an independent defect or a manifestation of any other genetic diseases (in this case we are talking about true microcephaly), and it can also develop as a consequence of various diseases the mother suffered during pregnancy (secondary, or false, microcephaly). However, in any case, this pathology is accompanied by a lag in the child’s mental development of varying degrees of severity and the presence of other neurological symptoms.
Statistical information
The incidence of the defect ranges from approximately 1:2000 to 1:10000 among all newborns. As an independent disease, true microcephaly is much less common and is detected in one out of 50 thousand children, both girls and boys. If this pathology occurs as a manifestation of another hereditary disease, then its frequency in the population is determined by the frequency of the underlying disease.
Anatomy of the brain
The brain is the main organ of the human nervous system; its formation and development begin in the earliest stages of the embryonic period.
The first rudiments of nervous tissue are formed already on the 18th day of intrauterine development. They are a neural plate, which consists of a small number of neurons (nerve cells). As the embryo forms, their number increases, as a result of which the brain and spinal cord and other elements of the system are formed from the neural plate.
A neuron is a highly specialized cell that consists of a body and many processes through which it communicates with a huge number of other cells. Thanks to this structure, the main function of the nervous system is ensured, namely the reception and processing of information, including the regulation of the vital functions of the entire organism as a whole. Through some neurons (they are called afferent), information in the form of nerve impulses enters the brain, where it is processed and a response nerve impulse is formed, which is sent to organs and tissues through other neurons (they are called efferent).
The formation of nerve cells in the brain is completely completed only at the time of birth, on average reaching about 150 billion neurons. However, throughout a person’s life they are not able to reproduce (divide), and at the same time they gradually die due to so-called apoptosis (a genetically programmed process of death of malfunctioning or damaged cells).
The brain is anatomically divided into three sections.
- Large hemispheres of the brain (right and left). Being the higher parts of the brain, they consist of the cortex and subcortical structures (hypothalamus, thalamus, etc.). The cerebral cortex contains neurons that are responsible for the formation of personality, the processes of self-knowledge and learning (higher nervous activity of a person). Subcortical structures ensure the formation of instinctive and behavioral reactions (sexual, food, etc.). It is also worth noting that the cerebral cortex under normal conditions has an inhibitory effect on subcortical structures; in other words, a person’s consciousness can suppress his instinctive reactions.
- Brain stem. It includes the medulla oblongata, the pons, and the midbrain and diencephalon. They provide reflex activity of the human body, and also maintain communication between the brain and spinal cord. In addition, the trunk contains various nerve centers (for example, vasomotor, respiratory, etc.). They, in turn, ensure the performance of those physiological functions that are not controlled by consciousness (for example, a person breathes automatically, without thinking about it).
- The cerebellum is a small structural formation that is responsible for coordinating human movements, maintaining muscle tone and maintaining balance during complex movements (walking, running, etc.).
The human skull is divided into the brain and facial sections. The latter includes the bones of the face. The development of the skull comes from embryonic tissue called ectoderm. It surrounds the rudiments of the brain from the very beginning of their formation.
There are three stages in the formation of the skull bones:
- membranous - a layer of cells that surrounds the future brain, becomes soft membranous tissue, simultaneously increasing with the growth of brain tissue;
- cartilaginous - from about the sixth to seventh week of embryonic development, this tissue in the area of the base of the skull gradually turns into denser cartilaginous tissue;
- bone - already from the eighth to tenth week of the intrauterine period, ossification points are formed in various parts of the skull, which are zones of the beginning of the growth of bone tissue.
By the time of birth, some areas of membranous tissue (fontanelles) remain in the roof of the skull of a newborn child, which ensure bone mobility during childbirth or when the brain enlarges for any reason.
The large (anterior) fontanelle has a diamond shape and is located at the junction of the frontal and parietal bones. It completely ossifies and closes by the age of two years.
The small (posterior) fontanel has the shape of a triangle and is located in the occipital region at the junction of the parietal and occipital bones. As a rule, it becomes overgrown by the second month of life.
The lateral fontanels are paired and small in size, they are located on the side surface of the head, slightly in front and behind the ears, and are also completely overgrown by the second month of life.
The bones of the facial skull are formed from the so-called gill arches, which are derivatives of mesoderm (another embryonic tissue). Thus, the development of the brain and facial parts of the skull occurs independently of each other. In addition, the formation of the facial skull is practically independent of the development and growth of the brain; however, the size of the cerebral skull normally always corresponds to the volume of the cerebral hemispheres.
At the end of the 19th and beginning of the 20th centuries in Europe and North America, children with microcephaly were sold to the circus. There they took part in the so-called “freak show”.
Causes of microcephaly
Depending on the cause of microcephaly, there are two forms: primary and secondary. In the first case, the disease is caused by a chromosomal mutation, as well as as a result of unfavorable external factors during fetal development in the first and early second trimester.
Secondary microcephaly occurs both in the third trimester and after a complicated birth or during serious illnesses suffered by the child in the first months of life. It characterizes a more serious condition of the child, namely cerebral palsy and related complications.
Other causes of microcephaly can also be identified, the main one being a dysfunction of the genes that encode a protein called microcephalin, which is necessary for the proper development of the skull. Another common cause is Edwards, Down, Patau and “cry the cat” syndromes, which lead to multiple fetal malformations.
Microcephaly can be caused by other factors that affect the fetus during its intrauterine development in the mother’s body:
- Radioactive exposure;
- Excessive consumption of alcoholic beverages and smoking, as well as drugs;
- Taking strong medications;
- Past infectious diseases such as influenza, rubella, chickenpox and toxoplasmosis;
- Disorders of the endocrine system in a pregnant woman;
- Low water;
- Diabetes.
Reasons for the development of the anomaly
Taking into account the causes and time of occurrence, primary microcephaly (true or hereditary) and secondary (syndromic) are distinguished.
Primary microcephaly in children is a manifestation of hereditary diseases; it accounts for about 7–34% of all types of this anomaly.
Primary microcephaly
The following diseases are independent forms.
Giacomini syndrome is a hereditary microcephaly, which is predominantly manifested by mental disorders in combination with the occurrence of convulsive conditions, as well as the progression of paralysis.
Payne's syndrome - this disease is also hereditary. It affects only boys and is manifested by constant convulsive conditions of the lower extremities, nervous disorders and abnormalities in the functioning of the heart.
Microcephaly can be a manifestation of the following pathologies:
- Down syndrome - the appearance of an extra chromosome in the XXI pair, clinically manifested by impaired mental development of the child, a decrease in the size of the brain and cerebellum, as well as other characteristic symptoms;
- Patau syndrome - the appearance of an extra chromosome in the XIII pair, characterized by low birth weight of the newborn, microcephaly and other anomalies of the skull and internal organs;
- Edwards syndrome - the appearance of an extra chromosome in the XVIII pair, while children have a small or long and narrow skull, low birth weight, underdeveloped brain and cerebellum, as well as developmental defects of the facial skeleton, legs (mainly feet) and internal organs;
- cat cry syndrome is a chromosome defect in the V pair, which is manifested by microcephaly, low body weight, retardation in physical and mental development, as well as a characteristic cry in a child, similar to the meowing of a cat (due to damage to the cartilage of the larynx);
- Prader-Willi syndrome - damage to chromosome XV, characterized by microcephaly, delayed psychomotor development and various anomalies of internal organs and skeletal bones;
- Miller-Dieker syndrome is a defect in the XVII chromosome, leading to disruption of the development of brain neurons in the embryo, as a result of which the brain of a newborn child is reduced and devoid of convolutions, in addition, there is severe muscle weakness, delayed physical and mental development and defects of internal organs;
- phenylketonuria is a hereditary disease characterized by impaired processing and use of one of the amino acids - phenylalanine; the resulting toxic substances have a damaging effect on the central nervous system of the pregnant woman, and also inhibit the development and growth of the fetal brain.
Secondary microcephaly develops due to the influence of unfavorable factors on the fetus in the embryonic period, when the formation and formation of all brain structures occurs. In this case, the genetic apparatus of the parents is not damaged.
Causes of secondary microcephaly
- viruses and infections (rubella, cytomegalovirus, measles, toxoplasmosis);
- alcohol abuse - ethanol almost freely penetrates from the mother’s blood through the placenta into the fetus’s body, the most severe manifestation is the so-called fetal alcohol syndrome, manifested by mental retardation and defects in the development of internal organs;
- drug abuse - they can also easily penetrate the placental barrier and adversely affect the fetus;
- taking certain medications that are contraindicated during pregnancy (for example, anticancer drugs such as colchicine or busulfan);
- intrauterine hypoxia - insufficient oxygen delivery to the tissues and organs of the fetus, which leads to a delay in its growth and development, as well as the occurrence of mental retardation and various anomalies;
- fasting - if the expectant mother fasts for a long time or does not take the required amount of protein food, then the fetal organs cannot form normally, which can be fraught with the development of congenital dystrophies and pathologies;
- mechanical injuries in the early stages of pregnancy can lead to disruption of the development of the brain and internal organs, often even incompatible with life;
- exposure to radiation - in the embryonic period, very intensive growth of all tissues occurs, therefore the damaging effects of radiation on the fetus lead to irreversible changes in the brain.
What diagnostics are needed to determine a treatment program?
Effective treatment of microcephaly in Israel begins with an accurate diagnosis, which ensures the selection of the optimal treatment program in the future. The presence of modern equipment in the diagnostic wards of the Assuta clinic makes it possible to carry out all the necessary examinations. Israeli clinics provide everything that may be required during therapy. The primary type of disease can be diagnosed before the baby is born, using a prenatal ultrasound examination. Today, the effectiveness of this method is about 70%, and the disease itself can only be detected at 25-30 weeks of pregnancy. If primary microcephaly is suspected, in addition to ultrasound, other invasive examinations may also be required, which can confirm the pre-established diagnosis.
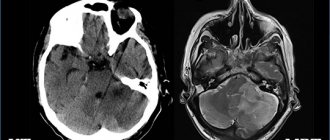
After birth, a child with suspected microcephaly is examined by a doctor who, based on a visual examination, can confirm or refute the diagnosis. In addition, a number of additional diagnostic procedures are also carried out, which make it possible to determine the degree of complexity of the disease. For microcephaly, mandatory examinations include MRI of the brain, CT, EEG and neurosonography.
calculate the cost of treatment
Forecasts
The life expectancy of a child diagnosed with microcephaly varies, since there are many causes of the disease, and very often the disease is accompanied by other abnormalities in the child’s body. As a rule, children with this disease live shorter lives, and their quality of life depends on the correct choice of therapy. Some children with mild degrees of the disease live a normal life, without significant deviations in intelligence and everyday behavior. Treatment of microcephaly in Israel is designed to stop the development of the disease and help the child adapt to life as much as possible.
https://www.assutahospital.ru/images/stories/2b3c24ec8648a921d5f23625e5f1e23d.jpg
2018-04-07 11:13:30 2018-04-07 11:13:30 IsramedikTurmed
5 1 Rating: 5
Votes: (2) https://www.assutahospital.ru/nevrologia/lechenie-mikrocefalii-v-izraile.html
Symptoms of microcephaly
In most cases, it appears immediately after the baby is born. If concomitant pathologies are compatible with life, then as the child grows older, the skull may undergo some changes and even increase slightly in size, but will always lag behind the age norm.
The usual appearance of such a newborn is characterized by the following features:
- noticeable predominance of the facial part of the skull over the brain;
- reduction in the vertical dimensions of the skull;
- prominent brow ridges;
- the presence of skin folds in the occipital region;
- the forehead is narrow and, in the case of a pronounced form, can be inclined at the back;
- wide and short nose;
- large, low-set ears.
The large fontanel and cranial sutures with this anomaly heal already in the first months of the baby’s life. In the future, children with microcephaly, as a rule, are lagging behind in weight and height, have a disproportionate physique, large sparse teeth and a narrow, high (Gothic) palate.
Neurological disorders can be represented by severe muscle weakness and loss of coordination, spastic paresis, convulsions and strabismus. Often such children may suffer from cerebral palsy (CP) and epilepsy. They begin to hold their heads up, crawl, sit and walk late. In addition, there is a noticeable delay in speech development, limited vocabulary, unclear articulation and impaired understanding of speech addressed to them.
With mild mental retardation, such patients can be quite trainable, capable of self-care, as well as performing simple tasks. But, in most cases, a microcephalic child requires care and supervision from adults.
Depending on their temperamental characteristics, these children can be classified into the so-called torpid or eretic group. Patients in the first case are characterized by lethargy, inactivity, and indifference to the environment; in the second case - hyperactivity, fussiness and unstable attention. The emotional sphere in patients with microcephaly is relatively preserved: children are good-natured and friendly, much less often they are emotionally unstable and have a tendency to affective outbursts.
Depending on the postnatal course of microcephaly, 4 types of its clinical manifestation are distinguished.
- Type I is characterized by the absence of an increase in symptoms of the disease. At the same time, the child retains completely normal motor activity, convulsions and spasms are not observed, and the IQ level is within 60;
- Type II is characterized by frequent manifestations and rapid progression of convulsive syndrome. The death of patients with this form of pathology, as a rule, occurs mainly from respiratory infections at the age of 10–12 years;
- Type III manifests itself with rapid progression; convulsive syndrome develops quite early, while its spastic component is sharply expressed. There is also a delay in psychomotor development;
- Type IV is an autosomal recessive pathology (unclassified microcephaly). It is characterized by the complete absence of convulsive and spastic syndrome.
Symptoms and clinical picture
The main visual symptom of microcephaly becomes noticeable immediately after the birth of the child. Disproportion of the skull is visible to the naked eye. The temporal part of the head seems to have been cut off. At the same time, the baby’s body is proportional.
With age, the symptoms of the disease begin to develop at an intensive pace . Microcephaly can have two forms - passive and aggressive. In the first case, the baby experiences lethargy and low mobility; in the second, excessive excitement.
Symptoms of microcephaly in children are the following conditions:
- narrow and sloping forehead;
- excessively protruding brow ridges;
- disproportionate physique;
- pronounced muscular dystonia;
- wide and short nose;
- narrow palate combined with sparse teeth;
- respiratory impairment;
- signs of mental retardation;
- critically low level of immunity;
- the presence of folds on the back of the head;
- pathologies of the cardiovascular system;
- spastic type paresis;
- convulsive conditions.
Consequences and quality of life
The quality of life of children with microcephaly is primarily determined by the severity of mental development disorders, which determines their future ability to self-care and learning.
Debility is a mild degree of mental retardation. In this case, children can be taught basic self-care skills, simple work, as well as speech, reading and writing. Such patients get along well in society, however, they cannot master the regular school curriculum, so they must go to special schools designed for children with mental disabilities. In this case, the prognosis for life is relatively favorable - these people can live up to 30 years, and in the most rare cases even into old age.
Imbecility is severe mental retardation. In such children, the ability to self-care is sometimes preserved, but often they still require constant care. Their intellectual abilities are extremely underdeveloped, and they are quite difficult to train. In this case, the prognosis for life is also less favorable - in quite rare cases, such patients even survive to adulthood. The cause of death, as a rule, is infectious diseases of the upper respiratory tract (pneumonia) or malformations of other internal organs, which are very often detected in children with microcephaly.
Idiocy - severe mental retardation. Such children are not able to care for themselves and cannot be taught. Their survival directly depends on the care of those around them. In this case, the prognosis is unfavorable - death occurs already in the first years of the child’s life due to disruption of the functioning of internal organs, concomitant developmental defects or infectious complications.
Types of disease
There are primary and secondary forms of the disease. In the first case, we are talking about congenital microcephaly, which occurs due to hereditary factors or as a result of a gene mutation. Occurs with a frequency of up to 34% of cases. Giacomini and Payne syndromes are considered independent diseases. Both diseases are of hereditary etiology.
They manifest themselves as mental disorders, increasing convulsive states, and the progressive occurrence of paralysis. Payne's syndrome is additionally accompanied by disturbances in the functioning of the heart. Microcephaly in a child is a pathology that is a sign of other syndromes: Patau, Down, Edwards, cat cry, Prader-Willi, Miller-Diecker, which in this case determines its secondary nature of origin.
All of these syndromes are associated with defects in certain chromosomes. The hereditary disease phenylketonuria, which occurs due to a violation of the metabolism of amino acids, especially phenylalanine, is the cause of the development of microcephaly in the fetus. As a result of insufficient utilization of phenylalanine, toxic products accumulate, which inhibit the growth of brain tissue.
Secondary microcephaly occurs against the background of diseases and injuries during the perinatal period or during childbirth. The causes of the secondary form are not related to genetic factors. There are 4 types of pathology, taking into account the nature of the postnatal course:
- Type 1. Symptoms do not increase, there are no convulsions or spasms of the limbs, motor activity is within normal limits. Intelligence quotient (IQ) is about 60.
- Type 2. Convulsive syndrome is observed with increasing intensity and strength of manifestation. The life expectancy of such children is about 10-12 years. Death usually occurs due to respiratory infections.
- Type 3. Characterized by a progressive convulsive syndrome with pronounced, predominant spasticity, impaired mental and motor functions.
- Type 4. Autosomal recessive form. It is characterized by the absence of convulsions and spasticity.
The quality of life of sick children depends on the degree of mental and physical impairment. Correct therapy in some cases can improve the patient's condition. There are stages of mental disorders:
- Moronism. Mild mental retardation. Children learn writing, reading, and self-care skills. Patients are not able to master the standard school curriculum, so they study in specialized schools and boarding schools. The prognosis is relatively favorable. Life expectancy can exceed 30 years; patients rarely live into old age.
- Imbecility. Mental retardation of moderate severity. The ability for self-care is often preserved. Intellectual functions are poorly developed. The child has difficulty learning. Life expectancy can reach 20 years. The cause of death is often pneumonia and other infectious lesions of the respiratory system, congenital malformations of organs.
- Idiocy. . The child cannot be taught and needs adult care. The prognosis is unfavorable. Death is possible during the first years of life. Main causes of death: concomitant pathologies, complications of infectious etiology, malfunctions of internal organs.
Depending on the nature of the course and temperament, patients with torpid and eretic forms are distinguished. In the first case, the child has an autistic syndrome (passivity, isolation, indifference, low mobility), in the second, motor restlessness, fussiness and emotional excitability predominate.
Diagnostics
Prenatal diagnosis of microcephaly includes ultrasound examination (ultrasound). During this procedure, the doctor compares the data obtained on the size of the fetus's head and torso with normal values. The most reliable information can only be obtained if you know exactly the duration of pregnancy.
Determining mutations of genes and chromosomes is the so-called invasive diagnostics. This method is carried out with a puncture of the fetal bladder, because the material for research is fetal villi, amniotic fluid, and also particles of epithelium.
Prenatal screening also includes a biochemical blood test. In addition, the pregnant woman is asked to fill out a special form, which, among other questions, contains a column about the timing of pregnancy. All information received and test results are processed in a special computer program that shows the likelihood of developing brain microcephaly.
A newborn baby is examined by a neonatologist in the delivery room in the very first minutes of his life through an external examination. If the diagnosis is confirmed, then an additional comprehensive examination is required.
Children with microcephaly must be consulted by a geneticist to identify concomitant hereditary diseases. In order to determine the degree and prognosis, it is also important to conduct a full instrumental examination: ultrasound of the brain (neurosonography), electroencephalography (EEG), radiography of the skull, as well as computed and magnetic resonance imaging (CT and MRI).
In addition, in order to identify defects in the development of other organs and systems, the child should receive consultations from specialized specialists: otolaryngologist (ENT), ophthalmologist, cardiologist, neurologist, neurosurgeon, orthopedist.
Causes
The development of microcephaly in a child can be influenced not only by internal, but also by external factors .
The most common cause of the disease is considered to be a genetic predisposition, but in some cases it is provoked by the negative impact of certain conditions on the body of a pregnant woman.
An important role is played by maintaining a proper lifestyle, diet and timely prevention of infectious diseases during gestation .
The following factors can cause the development of microcephaly in a child :
- exposure to adverse factors during pregnancy;
- genetic predisposition;
- congenital anomalies in women;
- intoxication of a woman during pregnancy;
- injuries to the abdominal area at any stage of pregnancy;
- consequences of radiation exposure of women;
- fasting of a woman during pregnancy;
- disruption of the process of growth and formation of brain tissue during intrauterine development;
- uncontrolled use of potent medications during gestation;
- abuse of alcohol, drugs or smoking during pregnancy;
- serious endocrine pathologies in women;
- intrauterine fetal hypoxia;
- consequences of infectious diseases during pregnancy.
What is Crouzon syndrome in a child? Find out about this from our article.
Treatment
Medical care for microcephaly comes down mainly to symptomatic support for patients, since it is impossible to restore normal brain activity, but there are ways to correct it. Treatment implies an integrated approach aimed at the physical and intellectual development of the child with the goal of maximizing his adaptation in society. It is carried out in three directions.
- Drug therapy. It is used to stimulate metabolic processes in the brain. For this, nootropic, sedative, anticonvulsant and dehydration drugs, as well as B vitamins, are prescribed.
- Physiotherapeutic procedures, physical therapy and massage.
- Therapeutic measures aimed at correcting the mental development of the child. In the event that mental retardation does not reach a severe degree (idiocy), then it is quite possible for such a patient to be taught basic self-care skills, performing simple work, and sometimes even speech and writing. For this purpose, long-term classes with specialists, special training programs and other necessary activities are held.
There is a so-called conductive pedagogy. Its essence is to create conditions that encourage the child to mental, motor and emotional activity, which creates the prerequisites for the further development of his intellect and psyche. During this treatment, the patient learns both simple and complex movements, learns to think and make decisions. At the beginning, the child develops motor behavioral stereotypes, which, as a result of long and hard work with teachers, gradually become meaningful and automated, that is, he does not just learn and repeat certain movements, but realizes the purpose for which he does this.
For each patient, an individual training program is drawn up, which in turn includes therapeutic exercises and physical education, exercises with various sports equipment, classes with a speech therapist, audiologist, psychotherapist and other specialists. This technique allows one to achieve fairly good results in children with various forms of mental retardation, including microcephaly.
Treatment of children with the primary form of pathology is sometimes successful. However, it should be remembered that even with timely and well-chosen therapy, the baby will never be completely healthy, but he will be able to lead a more simplified social life.