16 September 2020
64137
0
4.1 out of 5
Radicular syndrome is not a separate disease, but is a complex set of symptoms that occur when spinal nerves are compressed at the points where they branch from the spinal cord. This can be observed in many diseases, but in any case, the appearance of radicular syndrome requires immediate diagnosis of the causes of development and the beginning of treatment adequate to the situation. Indeed, in addition to the fact that it is accompanied by severe pain, prolonged compression or compression of the nerve roots can lead to irreversible changes and ultimately necrosis of the nerve fibers, resulting in loss of sensitivity and motor disorders in those parts of the body for the innervation of which they were responsible.
General information
In official medicine, damage to the spinal roots is also called radiculopathy. It is always based on compression of the nerve. This may be caused by an increase in size or displacement of certain anatomical formations bordering the spinal cord, the emergence of neoplasms or a reflex reaction of the body to irritants, manifested by muscle spasms, etc. There are many, and quite diverse, reasons for the development of radicular syndrome, but more on them later .
Radiculopathies have always been and remain common. But if previously they occurred mainly in people aged 40-60 years, today they are often diagnosed at a younger age, including teenagers. Damage to the spinal nerves and bundles can be observed in any part of the spine, on the basis of which radiculopathy is distinguished:
- cervical;
- chest;
- lumbosacral spine.
In all cases there is pain of varying severity and nature. But the place of its concentration and the area to which it will irradiate (give off) directly depends on which specific spinal root is infringed. This also has a direct impact on the nature of other symptoms that will accompany radicular syndrome. After all, the nerve roots extend in pairs at the level of each of the 33 vertebrae, each of which is responsible for transmitting sensory and motor impulses to the corresponding part of the body.
The pain associated with radiculopathy can be very similar to that characteristic of heart disease, including myocardial infarction, or other life-threatening conditions, such as peritonitis. This significantly complicates diagnosis and often leads to the prescription of treatment that is completely inappropriate for the patient.
Pain in radicular syndrome can reach such intensity that it deprives the patient of rest and completely immobilizes them. This can be combined with spastic muscle tension, forced posture, the appearance of sensory disturbances, for example, a feeling of numbness in the corresponding part of the body, impaired mobility up to paralysis, and other symptoms. Without intervention, this can lead to irreversible changes in the structure of the nerve and disability, so it is important to diagnose radicular syndrome as early as possible, determine the cause of its development and eliminate it conservatively or surgically, depending on the complexity of the situation.
Diagnostics
The primary diagnosis of radicular syndrome of the lumbosacral spine is made based on the symptoms of the medical history and physical examination (including a thorough examination of the neurological status). A thorough analysis of motor, sensory and reflex functions allows us to determine the level of damage to the nerve root.
If the patient reports typical unilateral radiating leg pain and there are one or more positive neurological test results, then a diagnosis of radiculopathy is very likely.
However, there are a number of conditions that may present with similar symptoms. Differential diagnosis must be carried out with the following conditions:
- Pseudoradicular syndrome
- Traumatic disc injuries in the thoracic spine
- Damage to discs in the lumbosacral region
- Spinal stenosis
- Cauda equina
- Spinal tumors
- Spinal infections
- Inflammatory/metabolic causes - diabetes, ankylosing spondylitis, Paget's disease, arachnoiditis, sarcoidosis
- Trochanteric bursitis
- Intraspinal synovial cysts
To make a clinically reliable diagnosis, as a rule, instrumental diagnostic methods are required:
- X-rays – can detect the presence of joint degeneration, fractures, bone defects, arthritis, tumors or infections.
- MRI is a valuable technique for visualizing morphological changes in soft tissues, including discs, spinal cord and nerve roots.
- CT (MSCT) provides complete information about the morphology of the bone structures of the spine and visualization of spinal structures in cross section.
- EMG (ENMG) Electrodiagnostic (neurophysiological) studies are necessary to exclude other causes of sensory and motor disorders, such as peripheral neuropathy and motor neuron disease
Causes
The spinal cord is an organ of the central nervous system. It is located in the spinal canal, on one side formed by the vertebral bodies together with the cartilaginous layers separating them (intervertebral discs), and on the other by the bony processes of the vertebrae. Thus, nature took care of protecting such a delicate and important organ for human life as the spinal cord.
The vertebral processes connect at several points, thereby forming natural openings called foraminal openings, through which the nerve roots extending from the spinal cord exit. They are large nerve fibers. As they move away from the spinal cord, they branch more and more into smaller fibers and reach all organs and parts of the human body, ensuring the transmission of appropriate signals to them that regulate their functioning.
Each spinal root is formed by sensory and motor nerve fibers. The first ones depart from the spinal cord from the side of the vertebral processes, i.e., closer to the back of the body and are therefore called posterior. The motor roots are located almost adjacent to the vertebral bodies and intervertebral discs and are called anterior. Thus, from their names it is clear that the anterior roots are responsible for motor capabilities and are responsible for muscle contraction, while the posterior ones transmit signals to receptors that must respond to the action of various kinds of irritating factors: touch, rough blows, etc.
As already mentioned, the spinal roots exit on both sides of the spine through natural openings formed by the arches and processes of the vertebrae. Therefore, any changes in the condition of the spine and the surrounding soft tissues can affect the condition of such important nerves and lead to the development of radicular syndrome.
The bulk of cases of radiculopathy occur in diseases accompanied by degenerative changes or inflammatory processes in the spine and surrounding tissues. In the latter case, it is provoked by a reflex muscle spasm that occurs in response to pain, or swelling of the soft tissues.
The most common causes of radicular syndrome are:
- osteochondrosis;
- protrusion and intervertebral hernia;
- spondylosis;
- spondyloarthrosis;
- spondylolisthesis;
- traumatic injury to the spine;
- infectious diseases of the spine;
- neoplasms.
The significant “rejuvenation” of radicular syndrome is largely due to changes in the lifestyle of modern people for the worse. It is excess weight, a sedentary lifestyle, bad habits, stress and lack of habit of maintaining posture that become the main reasons for the development of the above diseases, which in turn cause the occurrence of radiculopathy. All of them contribute to poor circulation, which becomes a “trigger” for the occurrence of degenerative changes in the cartilage tissue of the intervertebral discs and the development of corresponding pathologies.
Osteochondrosis
Osteochondrosis is a chronic disease in which there is a gradual destruction of the intervertebral discs against the background of degenerative-dystrophic changes occurring in them, i.e., the cartilage located between the vertebral bodies, acting as shock absorbers and ensuring the flexibility of the spine. They gradually become thinner and lose their natural elasticity. This leads to the fact that the bodies of neighboring vertebrae come closer together, and the diameter of the foraminal openings decreases, which can result in pinching of the spinal roots.
Protrusions and intervertebral hernias
Protrusions and hernias are one of the consequences of osteochondrosis, accompanied by deformation of the shape of the intervertebral disc and its protrusion. Initially, a protrusion is formed. This means that the disc is already deformed, but its outer shell (annulus fibrosus) still retains its integrity. If untreated, it ruptures in the most vulnerable place, which leads to the loss of internal contents (nucleus pulposus) into the spinal canal or the area from the front of the spine, i.e. the formation of a full-fledged intervertebral hernia.
Both protrusion and hernia can compress the spinal roots, either just one of them or both at once. This directly determines on which side neurological disorders will be observed. Large hernias and sequestered ones, that is, separated from the intervertebral disc, can also compress the spinal cord itself, which is fraught with serious complications. If the sequester begins to move along the spinal canal, this will be accompanied by the appearance of signs of damage to those nerve roots to the level of which it descends. If it reaches the lumbosacral region and the large bundle of nerves located there, called the cauda equina, it can lead to paresis and paralysis of the lower extremities.
Spondylosis
Spondylosis is another complication of osteochondrosis, in which the intervertebral discs wear out and become so thin that the vertebrae come together to a critically close distance. Against this background, their deformation occurs, which is accompanied by the formation of bone outgrowths called osteophytes on their edges. Over time, adjacent vertebral bodies can firmly fuse together, which leads to severe pinching of the spinal roots.
Spondyloarthrosis
This disease means the destruction of the facet joints, i.e., the place where the processes of the vertebrae meet. It involves damage to all elements of the joint, including its capsule, ligaments, surfaces and even periarticular muscles. This may also be accompanied by the formation of osteophytes and pinched nerve roots.
Spondylolisthesis
Spondylolisthesis is a pathology of the spine in which the body of one or more vertebrae is displaced relative to the underlying one by a certain distance. Since this disrupts the spinal axis and displaces all the anatomical structures in this area, this leads to compression of the spinal cord roots or even the spinal cord itself.
Traumatic injuries
Spinal injuries are far from uncommon. Strong blows, falls from heights, road traffic accidents and other factors can lead to vertebral subluxations, fragmentation and compression fractures, which is almost always accompanied by the development of radicular syndrome.
Infectious diseases
From the point of view of the occurrence of radiculopathy, the greatest danger is posed by syphilitic and tuberculosis infections, as well as osteomyelitis and nonspecific bacterial meningitis. In such cases, damage to the nerves by pathogenic viruses and bacteria may occur, which will lead to their inflammation.
Neoplasms
The spine and spinal cord, just like other organs, can be subject to the formation of benign and malignant tumors. In addition, with oncological diseases of other organs, metastases can separate from the maternal tumor, which, through the bloodstream, enter the tissues surrounding the spine and can also provoke pinching of the nerve roots and the occurrence of corresponding symptoms.
One of the very common benign tumors of the spine is hemangioma. Many people are already born with such a vascular neoplasm located in the vertebral body, or acquire it with age. It is not dangerous, but it significantly increases the risk of spinal compression fracture.
Surgery
Surgical methods for the treatment of radicular syndrome in the lumbosacral spine are necessary in cases where there is resistance to conservative treatment or there are symptoms indicating severe compression of the root such as:
- Increased radicular pain
- Signs of increased root irritation
- Muscle weakness and atrophy
- Incontinence or bowel and bladder dysfunction
As symptoms worsen, surgery may be indicated to relieve compression and remove degenerative tissue that is affecting the root. Surgical treatments for radicular syndrome in the lumbosacral spine will depend on which structure is causing the compression. Typically, these treatments involve some way to decompress the spine or stabilize the spine.
Some surgical procedures used to treat lumbar radiculopathy are:
- Fixation of vertebrae (spinal fusion - anterior and posterior)
- Lumbar laminectomy
- Lumbar microdiscectomy
- Laminotomy
- Transforaminal lumbar
intercorporeal fusion - Cage implantation
- Correction of deformity
Symptoms
The nature of the manifestations of radicular syndrome depends on the degree of compression of the nerve, the characteristics of its location, shape, thickness and a number of other individual characteristics. But radicular syndrome is always characterized by the presence of 3 components: pain, sensory and motor disorders.
The first signs of radiculopathy appear suddenly. As a rule, this occurs after making a sudden movement or heavy physical work. Initially, the pain may be mild or moderate, but it tends to intensify after any movement, laughing, coughing, sneezing and subside when taking a certain body position. In this case, the pain syndrome will be combined with:
- motor disorders with the development of cramping syndrome, i.e. short-term involuntary painful muscle contractions like cramps;
- sensory (sensitive) disorders in the form of paresthesia, i.e. the appearance of a tingling sensation, crawling, limited local sensation of cold or heat.
Pain with radicular syndrome is different from others. They are burning, baking, shooting. Their characteristic feature is spread from the spine to the extremities, irradiation into neighboring areas of the body, for example, legs, thigh or heart area, arms, etc., which is determined by the level of damage.
Pain syndrome causes reflex tension in the muscles and ligaments in the affected area, which leads to an even greater increase in pain. To alleviate his condition, a person tries to take a forced position of the body and avoids movements that will involve the affected segment of the spine.
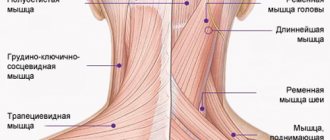
In this case, the muscles will be more tense on the side of the compressed root, which can be determined by palpation, i.e. palpation, of the back. This can cause the body to tilt in one direction or another. If the spinal roots are pinched at the level of the cervical vertebrae, over time this can lead to the development of torticollis, which will cause curvature of the spine.
If left untreated, the patient's condition will progressively worsen. Over time, compression of the spinal root will lead to:
- paresis (weakness) of the muscles innervated by the affected root;
- reduction of corresponding tendon reflexes;
- reduction or even complete loss of sensitivity of the corresponding part of the body (dermatitis);
- disruption of nutrition of the tissues of the innervated area, which will result in a decrease in muscle size, and then their atrophy, as well as thinning of the skin and an increase in its susceptibility to damage.
The spinal roots pass at the level of each vertebra. In which spinal motion segment one or both of them will be infringed completely determines the nature of the resulting disorders and their localization (on one side or both). If several roots are compressed at the same time, the symptoms will be mixed and combine the symptoms of damage to each of them.
If the radicular syndrome is infectious in nature, there will additionally be elevated body temperature, chills, a feeling of weakness and other characteristic symptoms.
Cervical region
The cervical spine is formed by 7 vertebrae. Compression of the spinal nerves at the level of each of them is accompanied by radicular syndrome, in which pain is concentrated in the spinal region and then spreads to other areas in combination with the corresponding manifestations:
- C1 – pain is felt in the back of the head, often associated with dizziness and nausea. If only one root is pinched, the head will be tilted towards the affected side. When palpating the neck in the area of the first vertebra, muscle tension on the corresponding side may be felt, and pressure will be painful.
- C2 – pain is localized both in the back of the head and the parietal region, there is a decrease in the sensitivity of the skin of the back of the head. In this case, there is a limitation of neck mobility, consisting of difficulties in turning and tilting the head.
- C3 – pain affects the back of the head, the side of the neck, radiates to the tongue, eyes and forehead. In these same areas, tingling or crawling sensations occur, as well as decreased sensitivity. It is difficult for the patient to tilt and raise his head, and when pressing on points in the projection of the third cervical vertebra, painful sensations occur.
- C4 – pain is concentrated in the area of the shoulder girdle and radiates to the anterior surface of the chest up to the 4th rib; it is also observed in the lower third of the posterolateral part of the neck. It is often accompanied by hiccups and voice changes.
- C5 – pain is present in the shoulder girdle, the lateral surface of the shoulder, which is associated with sensory disturbances, limited ability to abduct the shoulder, a decrease in the deltoid muscle and a decrease in the biceps reflex.
- C6—pain originating in the lower neck spreads through the biceps to the outer part of the forearm to the thumb. Additionally, a violation of sensitivity in these same areas and a decrease in muscle tone of the biceps, shoulder and forearm muscles are detected. The severity of the wrist reflex decreases.
- C7—pain is observed in the back of the shoulder and forearm, reaching the middle finger of the hand, and it is quite deep. Decreased sensitivity manifests itself in the triceps, pectoralis major and latissimus muscles, and wrist muscles. Additionally, the severity of the triceps reflex decreases.
Thoracic region
Degenerative-dystrophic changes in the thoracic spine are observed extremely rarely, in less than 1% of cases, but are not completely excluded. Therefore, due to the low frequency of damage to the spinal roots of the thoracic region, it can be very difficult to correctly diagnose the cause of chest pain, since they are almost always caused by diseases of the heart and gastrointestinal tract.
But since pinching of the nerve roots in the thoracic vertebrae is not excluded, let us consider the characteristic manifestations of nerve compression in each spinal motion segment:
- T1-T2 – pain is localized in the shoulder joint and armpits, they can radiate to the subclavian region, as well as the middle surface of the shoulder. This is accompanied by weakness and a decrease in the volume of the muscles of the hand, and the appearance of a feeling of numbness in it. If the spinal roots are damaged at the level of this spinal motion segment, drooping of the eyelids, swallowing disorders, and difficulty in moving food through the esophagus may additionally be observed.
- T3—T6 – girdling pain. They pass along the corresponding intercostal spaces and can be felt in the chest, and if the left nerve root is affected, then they can simulate an attack of angina.
- T7—T8 – pain radiates from the area of the spine in the area of the lower edge of the scapula, also spreads along the intercostal spaces and reaches the epigastric region. As a result, the patient may experience dyspeptic symptoms (heartburn, belching, a feeling of fullness in the stomach, rumbling, diarrhea, etc.), and abdominal pain.
- T9-T10 – pain is girdling and radiates to the upper abdomen, which can mimic the symptoms of appendicitis.
- T11—T12 – pain is often felt in the groin and suprapubic region, which is combined with impaired intestinal motility and resulting discomfort, changes in the consistency and frequency of stool.
Lumbosacral region
Due to the fact that the lumbar (L-vertebrae) and sacral (S-vertebrae) parts of the spine bear the greatest loads, it is in them that degenerative-dystrophic changes and inflammatory processes most often occur. Therefore, radicular syndrome most often occurs due to damage to the spinal roots in these parts of the spine.
- L1 – pain and sensory disturbances are observed in the groin area and spread to the upper outer quadrant of the buttock;
- L2 – pain is present in the front and inner part of the thigh, weakness is observed when adducting the hip;
- L3 – pain is observed in the greater trochanter, the anterior surface of the thigh and goes down to the lower third of the middle part of the thigh. But sensory disturbances are observed only on its inner surface in the area above the knee.
- L4 – pain spreads along the front of the thigh, extends to the knee and the middle surface of the lower leg up to the ankle. This is associated with a decrease in the quadriceps muscle, as well as a decrease in the strength of the tibialis muscles. That is why, when the spinal roots are damaged at the level of the 4th lumbar vertebra, the foot seems to slam when walking.
- L5 – pain sensations originating in the lower back radiate to the buttock, descend along the lateral surface of the thigh and lower leg and cover the first 2 toes. In these same areas, a decrease in sensitivity is observed, which is combined with a decrease in the tone of the tibialis muscle, as well as only the big toe or the entire foot.
- S1 - damage to the nerve roots at the level of the 1st vertebra of the sacral body is associated with the appearance of pain in the lower back and sacrum, which radiates along the posterolateral surface of the thigh and lower leg to the foot and 3-5 fingers. Sensitivity and muscle tone disturbances are concentrated along the lateral edge of the foot, and the calf muscle also suffers. In this case, there may be a decrease in the ability to turn the foot and extend it.
- S2 – pain and sensory disturbances are present in the sacral area, affecting the back of the thigh and lower leg, the plantar part of the foot, and the big toe. Often there are cramps in the thigh.
- S3-S5 – damage to the spinal roots at this level is called sacral caudopathy, which is usually associated with the appearance of signs of compression of 3 roots simultaneously. This condition is characterized by the presence of pain and lack of sensitivity in the area of the sacrum and perineum, and there is also often a disruption in the functioning of the sphincters of the pelvic organs.
Signs of osteochondrosis of the thoracic region
Clinical manifestations of thoracic osteochondrosis depend on the patient’s age, degree and stage (acute or remission) of the disease.
At first, without treatment, thoracic osteochondrosis can be asymptomatic - even in the second stage of the disease, pain is often absent. The most characteristic of the disease is the pain that occurs when taking a deep breath - if you take a full lungful of air and hold your breath for a few seconds. For osteochondrosis of the thoracic region, two types of pain are specific:
- dorsago
- acute attacks of pain that quickly pass (usually torment at night, when bending and turning the body, load); - Dorsalgia
is a mild pain lasting up to 3 weeks, which subsides as the patient “walks around.”
Other important criteria for self-diagnosis are stiffness and crunching in the sternum area - for example, when trying to move your shoulders one by one, or bring your shoulder blades together.
Significant symptoms and sensations during the treatment of thoracic osteochondrosis include:
- Pain when lifting weights
or after a long stay in one position is usually shooting. With movement and active breathing, the pain intensifies and can “encircle” the chest, radiating to the armpit or collarbone. Some patients are also bothered by aching pain in the shoulders at rest. Unlike angina pectoris and other “heart” pains, which last from 3-5 minutes to an hour, thoracalgia with thoracic osteochondrosis can last for weeks and months, sometimes intensifying for several days, then declining. Treatment of thoracic osteochondrosis with “heart” medications (Corvalol, Valocordin, aspirin-cardio) does not bring results. - “Goosebumps” in the chest
. The sensation most often occurs in the upper part of the thoracic region, in the muscle fibers. May be accompanied by a feeling of numbness, decreased sensitivity (both in the chest and mid-back). Because of this, the feet become cold, peeling of the skin, brittle nails and other symptoms of insufficient tissue nutrition are observed. - Colic in internal organs
. Sharp, stabbing pain can occur in the stomach, heart and even kidneys, which is why patients often suspect they have an ulcer, angina or heart attack. If you have such symptoms, to treat osteochondrosis of the thoracic spine, it is better to visit a neurologist, and only then contact specialized doctors to avoid making an incorrect diagnosis. - Reflex disorders.
With thoracic osteochondrosis, they are most often expressed in rhythmic twitching of the shoulder and trapezius spinal muscles in response to their stretching. - General weakness of the thoracic spine
. It becomes more difficult for patients to maintain their posture; they begin to slouch and hunch over. At the same time, the muscles of the back become more and more tense, the back “hardens”. - Labored breathing
. Shortness of breath when climbing stairs, a feeling of lack of air or tightness in the chest are the most common symptoms of thoracic osteochondrosis. Treatment begins with the patient's complaints of cough, which is why patients assume they have pneumonia. - Instability of the psycho-emotional sphere
. People who go through the symptoms and treatment of osteochondrosis of the thoracic spine become more irritable, suffer from constant fatigue and fatigue even with sufficient rest. - From the gastrointestinal tract, patients are concerned about a feeling of satiety and loss of appetite
, bloating, flatulence, heartburn, irregular bowel movements, and nausea. Patients are plagued by pain in the throat and esophagus, a feeling of a “lump” when swallowing.
In women, symptoms for the treatment of osteochondrosis of the thoracic region also include pain in the chest and mammary glands, and in the groin. They are incorrectly classified as gynecological problems. In this case, it is better to start checking symptoms and treating thoracic osteochondrosis with medications with a visit to an orthopedist or neurologist. Treatment of thoracic osteochondrosis in men similarly allows solving problems with potency and urination caused by innervation disorders
Diagnosis of radiculopathy
For an experienced neurologist, it is not a problem to detect signs of radicular syndrome. In addition to the characteristic symptoms, the results of an examination of the patient (the doctor evaluates the posture that the person involuntarily assumes, muscle tone, the presence of painful sensations on palpation) and specific neurological tests carried out help him make a diagnosis. But in order to accurately determine at what level compression of the spinal root occurs and what causes it, a number of instrumental studies are required. The neurologist will determine which of them are necessary and write a prescription:
- radiography of the spine in 2 projections;
- CT;
- MRI;
- electroneuromyography.
If there is a suspicion of the presence of diseases of the heart, gastrointestinal tract or others, ultrasound, blood tests, urine tests, etc. may be additionally prescribed.
For diagnosing intervertebral disc pathologies, MRI is considered the most informative method. With its help, you can detect even the slightest changes in the structure of the discs, which will not be visible with any other type of examination. But if it is necessary to accurately examine bone elements and detect their deformations, an X-ray, or better yet a CT scan, is required.
Treatment of osteochondrosis of the thoracic spine
Treatment of osteochondrosis of the thoracic region at stages 1 and 2 of the disease involves conservative therapy aimed at relieving inflammation, stopping pain, restoring nerve conduction and blood supply. Also, to alleviate the condition, drugs and techniques are used to relieve spasm, incl. strengthening the back muscles.
Treatment of osteochondrosis of the thoracic region with medications in the acute stage of the disease takes from 1 to 3 months; in the future, lifelong adherence to simple rules is required to maintain remission. If there are no indications for hospitalization, maintenance therapy is carried out on an outpatient basis and does not require large costs.
In cases of advanced osteochondrosis, spinal cord herniations and other potentially dangerous conditions, surgery is prescribed to decompress and stabilize the spine (microdiscectomy, foraminotomy, laminectomy). Postoperative treatment of thoracic osteochondrosis in a hospital takes from 3 to 7 days, complete healing - up to 14 days.
Physiotherapy for thoracic osteochondrosis
For the treatment of osteochondrosis of the thoracic spine, the following is used:
- Magnetic laser therapy.
Helps relieve pain, swelling and inflammation, increases humoral immunity. The course consists of 14 daily sessions of 10-15 minutes. The intervals between courses should last at least 1 month, and the number of courses per year should not exceed 4. - Amplipulse (SMT), incl.
with novocaine. Has a strong analgesic effect. Stimulates muscles and prevents muscle atrophy. Helps relieve swelling and inflammation, dilates blood vessels and improves tissue nutrition. The course requires 8-15 procedures for 10-20 minutes. - Ultrasound therapy (optional with hydrocortisone).
Provides micromassage of periarticular tissues, improves nutrition of cartilage, prevents inflammation and joint destruction, dilates blood vessels and accelerates regeneration. It has an analgesic and antispasmodic effect. The course includes 10-12 procedures of 10-15 minutes each. - Mineral baths, mud therapy, ozokerite and paraffin baths and other balneological techniques.
They provide a long-lasting dilation of blood vessels, have an antioxidant and anti-inflammatory effect, relieve swelling and facilitate movement in the joint. The duration of the session, the length of the course and the impact depend on the composition of the bath or therapeutic mixture. - Hydromassage.
Improves tissue nutrition and nerve conduction, promotes relaxation of spasming muscles. Accelerates regeneration and shortens the recovery period after exacerbations of thoracic osteochondrosis. Course – 10-25 sessions. The duration of the session is gradually increased from 15 to 30 minutes. - Thermotherapy.
It has a relaxing, analgesic and anti-inflammatory effect, improves lymph and blood circulation. The duration of the course and procedure depends on the technique. - Acupuncture.
Stimulates regeneration and improves the innervation of tissues around the spine, the functioning of the internal organs of the chest, normalizes blood circulation and reduces pain due to the release of endorphins. The course consists of 15 sessions, which are held daily or every other day. - Traction methods.
Used for non-surgical elimination of hernias and protrusions, combating numbness of the limbs and clamps. They help increase the distance between the vertebrae, improve posture, promote decompression of nerve roots, relax and strengthen the back muscles. This reduces the intensity of inflammation and pain. The standard course is 10-12 sessions, repeated completion may be required. - Manual therapy.
Improves blood circulation in the spinal cord, helps fight fainting. Restores the anatomically correct position of the spine, promotes the treatment of hernias and protrusions. Eliminates spasms and tightness in the thoracic region. The course is a minimum of 10-15 sessions lasting from several minutes to an hour.
In addition to physical therapy and drug treatment for thoracic osteochondrosis, patients may need to work with a psychologist. This will help get rid of the anxiety that accompanies diseases of the musculoskeletal system, and will also motivate you to maintain healthy posture. During physical activity, patients are recommended to wear an orthopedic corset (but not constantly, so as not to weaken the back muscles).
Massage for thoracic osteochondrosis
For osteochondrosis of the thoracic spine, clinical massage is recommended - classic therapeutic (with drugs for the treatment of thoracic osteochondrosis or essential oils), vacuum, lymphatic drainage, water or acupressure. The doctor or device has an indirect effect on the thoracic region through the muscles of the shoulders and upper back, stimulates blood microcirculation, eliminates pain and swelling, restores normal range of motion and normalizes the tone of the muscle corset. Massage also enhances the effect of treating thoracic osteochondrosis with medications. Treatment of thoracic osteochondrosis in male drivers and operators involves the use of massage devices - cushions and seat covers, bolsters, hand massagers.
Gymnastics for the treatment of thoracic osteochondrosis
The first lasting effect from exercise therapy occurs during the first 2 weeks of classes, but temporary relief is possible after 4-7 sessions. It is necessary to increase the load in the treatment of osteochondrosis of the thoracic region gradually, alternating it with rest. Performing exercises through pain and severe fatigue is not allowed, as are sudden movements that can injure the joint and adjacent tissues. It is very important to perform exercises for the treatment of thoracic osteochondrosis daily, or better yet, 3-5 times a day, at least 5 repetitions each.
- Stand straight, feet together, arms along your body. As you exhale, raise your arms up, and as you inhale, bend back. Lower your arms and bend forward as you exhale, lowering your head and shoulders.
- Sit on a chair. As you inhale, place your straight arms behind your head, and as you exhale, bend well back, without lifting your shoulder blades from the back of the chair.
- Standing on all fours, arch your back and freeze for 3 seconds, looking straight ahead.
- Lying on your stomach, place your hands on the floor and bend back, lifting your chest off the floor.
- Lying on your stomach, extend your arms along your body. Bend your chest, making a “boat”: at the same time lift your legs and head up.
In addition to the proposed gymnastics for the treatment of thoracic osteochondrosis, patients benefit from Nordic walking, yoga, cycling and water sports (swimming, diving, water aerobics). Don't forget to relieve your spine during the day: don't sit in one position for more than 2 hours, and during your lunch break, try to lie down on a flat surface for 40 minutes. Stretch, stand up, bend over as soon as your back begins to stiffen.
Relief of symptoms and treatment of osteochondrosis of the thoracic region in women also requires maintaining the correct position of the body when performing household duties - try to spend as little time as possible in inclined positions, if possible, sit down straight if long-term housework is required.
Treatment of radicular syndrome
Treatment for each patient is selected individually depending on what disease caused the development of radicular syndrome. In the absence of a serious threat to the health and life of the patient, for example, sequestration of an intervertebral hernia or other severe complications, they initially try to relieve the nerves from compression using conservative methods. In such situations, in accordance with the diagnosis, patients may be prescribed:
- drug therapy, which consists in the use of NSAIDs in the form of injections, tablets, ointments or suppositories, chondroprotectants, muscle relaxants, vitamins (if the radicular syndrome is infectious, the use of antibiotics, antiviral and other agents is indicated);
- manual therapy, which helps eliminate functional blocks, normalize muscle tone, and most importantly, restore the normal position of the vertebrae and release compressed spinal roots;
- physiotherapy, which increases the effectiveness of other measures taken to treat radicular syndrome;
- Exercise therapy, which is an obligatory component of treatment and is necessary to improve blood circulation, strengthen muscles and prevent their atrophy.
In case of very severe pain, patients can undergo blockades of the corresponding spinal motion segment. They do not have a therapeutic effect, but are able to eliminate pain of any severity in a matter of minutes.
But conservative therapy does not always bring positive changes in the patient’s well-being. If the patient’s condition does not improve within 3 months after its onset, he will be indicated for appropriate surgery. Also, surgical intervention may be prescribed immediately if:
- large intervertebral hernias;
- sequestered hernias;
- dangerous tumors of the spine or surrounding tissues;
- spondylolisthesis and some other pathologies.
In each case, the method of surgical intervention is selected individually, based not only on what pathology was detected, but also on its severity. For example, for small intervertebral hernias, percutaneous surgery techniques can be used, in particular cold plasma nucleoplasty or hydroplasty. For larger intervertebral disc defects, endoscopic surgery or microdiscectomy is indicated. For large hernias, the only way out of the situation is microdiscectomy or open discectomy with stabilization with a metal structure. If the patient is diagnosed with spondylolisthesis, it will be possible to eliminate the radicular syndrome only by implanting special fixing titanium plates, etc.
Thus, the appearance of symptoms of radicular syndrome or radiculopathy is a reason to immediately contact a neurologist, conduct an appropriate examination and begin treatment. But even if there are indications for surgery, you should not be afraid of it. Modern spinal surgery techniques are highly effective, and they are much safer than non-intervention and the inevitable addition of complications and subsequent disability.
Conservative treatment:
- Rest: avoid activities that cause pain (bending, lifting, twisting, turning or bending backwards. Rest is necessary for acute pain syndrome
- Drug treatment: anti-inflammatory, painkillers, muscle relaxants.
- Physiotherapy. For acute pain syndrome, the use of procedures such as cryotherapy or chivamat is effective. Physiotherapy can reduce pain and inflammation of the spinal structures. After the acute period has stopped, physiotherapy is carried out in courses (ultrasound, electrical stimulation, cold laser, etc.).
- Corseting. The use of a corset is possible in case of acute pain syndrome to reduce the load on the nerve roots, facet joints, and lumbar muscles. But the duration of wearing a corset should be short, since prolonged fixation can lead to muscle atrophy.
- Epidural steroid injections or facet joint injections are used to reduce inflammation and control pain in severe radicular syndrome.
- Manual therapy. Manipulations can improve the mobility of the motor segments of the lumbar spine and relieve excess muscle tension. Using mobilization techniques also helps modulate pain.
- Acupuncture. This method is widely used in the treatment of radicular syndrome in the lumbosacral spine and helps both reduce symptoms in the acute period and is included in the rehabilitation complex.
- Exercise therapy. Exercise includes stretching and strengthening exercises. The exercise program allows you to restore joint mobility, increase range of motion and strengthen your back and abdominal muscles. A good muscle corset allows you to support, stabilize and reduce tension on the spinal joints, discs and reduce the compression effect on the spine. The volume and intensity of exercise should be increased gradually to avoid relapse of symptoms.
- In order to achieve stable remission and restore full functionality of the spine and motor activity, it is necessary for the patient, after completing the course of treatment, to continue independent exercises aimed at stabilizing the spine. The exercise program must be individual.
Treatment of cervical radiculopathy
Surgery for cervical radiculopathy is indicated only for symptoms of spinal cord compression (spondylogenic cervical myelopathy) and severe pain.
In the vast majority of patients with vertebrogenic cervical radiculopathy, conservative therapy shows good results. The main task at the first stage of treatment is pain relief. Nonsteroidal anti-inflammatory drugs (NSAIDs) are used, which have both analgesic and anti-inflammatory effects. NSAIDs should be used from the first hours of the development of the disease. The choice of drug is determined by the ratio of its effectiveness and safety. To reduce the severity of the pain syndrome and improve the patient's condition, some drugs from the group of anticonvulsants and antidepressants can be used (if the pain syndrome lasts more than 6-7 weeks). To relieve acute pain, combined vitamin preparations of group B (B1, B6, B12) are also used, which have a positive effect on processes in the nervous system (metabolism, metabolism of mediators, transmission of excitation) and on the regeneration of damaged nerves.
In the acute period, immobilization of the neck with a soft or semi-rigid collar is indicated (primarily at night), the duration of which should be limited to several days
Subsequently, physiotherapy, reflexology, massage, and therapeutic exercises are carried out. In case of chronic pain syndrome, a comprehensive psychophysiological approach is required, taking into account the importance of both peripheral and psychological factors in the origin of pain.