Mental retardation (oligophrenia, dementia) is a specific condition caused by a special level of activity of the central nervous system, and not a mental illness.
It is chronic, non-progressive and occurs in connection with organic pathology of the brain. The affected central nervous system limits the intellectual development of the child. As a rule, such a deviation occurs during intrauterine development and is finally formed before three years of age.
Due to various types of brain damage that provoked the breakdown of mental functions, a person can develop oligophrenia even in adulthood. This is called dementia. It should be distinguished from acquired dementia, which refers to a decrease in intelligence due to age-related changes in the brain.
Mental retardation is classified as a severe pathology. However, depending on the form of its development, a specialist can adapt the patient to the surrounding society as much as possible and correct some deficiencies.
Classification of the device
There are several degrees of this pathology, determined by IQ:
- mild (moronicity) – IQ 69–50. This form is characterized by slight developmental retardation, which allows a person to socialize in the surrounding society;
- moderate (not pronounced imbecility) – IQ 49–35. Such patients have basic communication skills, are able to understand gestures and respond to them, but it is difficult to understand them when they are worried;
- severe (severe imbecility) – IQ 34–20;
- deep (idiocy) - IQ less than 20. It is characterized by practically undeveloped speech, lack of instincts and primitive reactions. Among the additional manifestations you can notice the following: low or complete lack of coordination of movements, apathy, unjustified malice, anger, etc.
Moronicism is, in turn, divided into three more forms (depending on IQ):
- light – 69–65;
- moderate –64–60;
- heavy – 59–50.
Mental retardation, characterized by a decrease in intelligence, disorders of speech and motor development, and emotional and volitional spheres, is a very common disease. In the world, there are from 1 to 3% of people suffering from this disease. The fact that 75% of them have a mild form can “calm down.”
Quite often, this pathology is combined with other quite serious mental and somatic diseases: Down's disease, cerebral palsy, epilepsy, autistic disorders, blindness, deafness, etc.
UL cannot progress, but with a mild degree, timely educational measures and teaching methods can even increase intelligence.
Possibilities of regulating cognitive function in children using vitamin-mineral complexes
Despite the growing well-being of the population of the Russian Federation, the problem of year-round polyhypovitaminosis in children is quite acute. A decrease in the amount of food entering the body due to changes in a person’s lifestyle, the consumption of refined foods, shelf-stable products, and foods that have undergone long-term culinary processing makes it impossible to replenish the required amount of essential micronutrients only with the help of a balanced diet. Studies of vitamin and mineral status in children conducted in recent years show that ascorbic acid deficiency among the child population reaches 70–95%; 60–80% of children have an insufficient supply of thiamine, riboflavin, pyridoxine, niacin and folic acid [1]. Cognitive function is a complex and incompletely understood phenomenon. However, a number of studies have been conducted to assess certain cognitive functions, such as memory and reproduction, mental acuity and the ability to concentrate, the ability to learn and solve problems, the ability to mobilize and the speed of the thinking process, which has allowed us to establish a clear relationship with the provision of the child’s body with certain micronutrients. Development of the human brain The main growth of the brain and the peak development of synapses occur from the 34th week. pregnancy up to 2 years of life, by preschool age synaptic density reaches the level of the adult brain. Myelination of some areas of the brain that control higher cognitive functions continues into adolescence. Research has shown that the maturation of specific brain regions during childhood is associated with the development of specific cognitive functions. Development of the frontal lobes of the brain, responsible for higher cognitive functions, appears to occur in bursts: during the first 2 years of life, between 7 and 9 years, and at 15 years. Development of several subcortical structures, including the basal ganglia, amygdala, and hippocampus, continues into late adolescence. In addition, a meta-analysis confirmed the relationship between hippocampal size and memory subsystem performance during brain development in children and young adults. Diet has been shown to have a direct effect on gene expression in animal and human studies. One of the first studies, Nutritional Epigenomics, showed that offspring of mothers who starved during the wartime 1940s had an increased risk of developing cardiovascular disease, kidney and lung damage, metabolic disorders, decreased cognitive function and DNA hypo- and hypermethylation segments. Folic acid deficiency during neural tube closure between days 21 and 28 after conception is known to predispose to fetal malformations. During the first 2 years of life, the brain grows rapidly, reaching 80% of its adult weight. During this period of life, nervous tissue can be especially sensitive to nutritional deficiencies. During adolescence, structural changes in the brain and cognitive maturation occur, in particular, major events in the prefrontal cortex [2]. The influence of micronutrients on cognitive functions Omega-3 PUFAs are an important structural component of the gray matter of the brain, which, according to some scientists, is responsible for the development of intelligence in the body. Omega-3 PUFAs are also necessary for the proper functioning of the retina. Sufficient Omega-3 content in food largely determines the child’s mental abilities, the correct development of fine motor skills and motor-visual coordination. Omega-3 PUFAs are essential for the normal functioning of cells in the human body; they are not synthesized in the body and must come from outside with food. The main and most studied members of the Omega-3 PUFA family are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). The main role of omega-3 PUFAs is to ensure the functioning of cell membranes, transmembrane ion channels and the regulation of physiological processes through the synthesis of lipid mediators. EPA and DHA are embedded in the phospholipid layer of cell membranes and affect their fluidity, changing basic functions such as enzymatic activity, impulse transmission and receptor function. Essential fatty acids promote neuronal growth and synapse formation, therefore influence signal transmission and processing, and also regulate gene expression in the brain. A number of epidemiological studies have shown a positive association between consumption of fish, a source of omega-3 fatty acids, during pregnancy and children's cognitive development. Early research found that eating fish during pregnancy was associated with better speech and social skills. The ALSPAC study found that children whose mothers consumed little seafood during pregnancy had lower IQ at age 8, minor behavioral problems at age 7, and poorer development of fine motor skills, language, and social behavior at ages 6, 18, and 30. and 42 months A Danish national cohort study of 25,446 children aged 6 months and 18 months demonstrated that maternal fish consumption was beneficial for children's mental development, even after adjusting for other factors such as breastfeeding, sociodemographic characteristics and others. Two studies of Inuit children in Arctic Canada found that higher levels of DHA in umbilical cord blood were associated with improved cognitive function and school performance [2]. The source of PUFAs are food products, which for a number of reasons are rarely included in the diet of people living in our country: some varieties of marine fish (salmon, tuna, sardine, mackerel), vegetable oils (rarely consumed rapeseed and soybean), nuts , some types of fruits. In this regard, there is a need for additional intake of omega-3 PUFAs in the form of biologically active food additives. Deficiency of omega-3 PUFAs makes a significant contribution to the increased risk of a child developing attention deficit hyperactivity disorder (ADHD). Evidence suggests that dietary supplementation with omega-3 PUFAs helps compensate for behavioral problems and learning difficulties in patients with ADHD [3–5]. The existence of a relationship between omega-3 PUFA deficiency and the risk of ADHD is confirmed not only by clinical, but also by experimental data. Firstly, limiting the diet of animals with omega-3 PUFAs leads to an increase in hyperactivity and a decrease in cognitive abilities in the offspring. Secondly, animal studies have shown an association between omega-3 PUFA deficiency and abnormalities in dopamine metabolism. Third, clinical observations indicate decreased levels of omega-3 fatty acids in patients with ADHD. Finally, biochemical data indicate the role of omega-3 PUFA deficiency in the formation of behavioral disorders through disruption of dopamine metabolism in the basal ganglia [6]. Of particular interest is the study of electromagnetic activity of the brain depending on the intake of omega-3 PUFAs. Children (n=33) aged 8–10 years received placebo, moderate dose DHA (400 mcg/day), or high dose DHA (1200 mg/day) for 8 weeks. Relative changes in the cerebral cortex during attention tests were determined using functional magnetic resonance imaging. At the 8th week. the DHA content in erythrocyte membranes increased by 47% in the group with a medium dose of DHA and by 70% in the group with a high dose of PUFAs. In the placebo group, DHA levels dropped by 11%. During attention tests, both DHA groups showed significantly greater changes from baseline in dorsolateral prefrontal cortex activation than the placebo group. The higher the dose of DHA, the greater the decrease in cerebellar activation, which corresponded to a decrease in hyperactivity. RBC DHA content was positively correlated with the degree of activation of the dorsolateral prefrontal cortex (improved behavioral control) and shorter reaction time [7]. Clinical observations confirm the results of basic research and indicate a clear relationship between omega-3 PUFA deficiency and the risk of ADHD. Children with ADHD had significantly lower levels of DHA PUFA and total omega-3 fatty acids in the blood [8]. Choline. Of great importance for the formation of mnestic functions in a child is a vitamin-like substance - choline, which has membrane-protective, anti-atherosclerotic, nootropic and sedative effects. In the form of acetylcholine (a compound of choline and acetic acid ester), choline is a transmitter of impulses in the nervous system. Choline is necessary for the normal functioning of the nervous system; it is part of the myelin protective sheath of the nerves, protecting the human brain throughout life. It is believed that the level of intelligence largely depends on how much choline we received in the womb and during the first 5 years of life. Vitamin B4 restores liver tissue damaged by toxic drugs, viruses, alcohol and drugs. It prevents the development of gallstone disease and improves liver function. Choline normalizes fat metabolism, stimulating the breakdown of fats, and helps absorb fat-soluble vitamins (A, D, E, K). Lack of choline in children leads to irritability, increased fatigue, and nervous breakdowns. Choline is a component of lecithin, a substance very important for brain tissue. Lecithin (a mixture of phospholipids) belongs to the group of essential nutritional components. Lecithin deficiency is a serious problem for child health. Lecithin is a mixture of phospholipids: choline, inositol and phosphatides. Essential fatty acids and phospholipids, being the structural units of all cell membranes, restore the barrier and metabolic functions of cells, ensure the entry of nutrients into the cell and the removal of waste products from it. Phosphatidylcholine promotes the emulsification of dietary fats and increases the absorption of fat-soluble vitamins A, D, E in the digestive tract. Manifestations of lecithin deficiency in children are quite diverse and variable. In children of the first years of life, due to lecithin deficiency, intracranial hypertension may occur, delayed psychomotor and speech development, behavioral disorders (psycho-emotional imbalance), decreased ability to concentrate, and memory impairment [9]. Classic manifestations of lecithin deficiency in children include disorders of neuropsychic development (decreased functionality of the central nervous system, increased irritability, tearfulness, etc.), disorders of cognitive functions (decrease in memory parameters, attention, thinking, academic performance), decreased motor activity (fatigue and increased fatigue), etc. Researchers from the USA have demonstrated that lecithin has the ability to improve the so-called “brain chemical activity”, having a beneficial effect on higher cortical (cognitive) functions such as memory, speech and motor skills. Subsequently, this allowed A. Barbeau (1978) to highlight the problem of using lecithin for the treatment of neurological diseases (Friedreich's ataxia, Huntington's chorea, etc.) [10]. Since the 1980s. A number of works have appeared in the medical literature on the use of lecithin for various cognitive impairments, memory disorders, as well as in the treatment of dementia of the Alzheimer’s type [11]. Domestic experts reported the possibility of effective use of lecithin in other types of psychoneurological pathology in children and adolescents, including early childhood autism (ECA), psychomotor development delay (PDMR), Gilles de la Tourette syndrome, asthenoneurotic reactions, depressive neurosis, Meniere's disease, epilepsy and etc. It is assumed that lecithin, which is part of the myelin sheaths covering nerve fibers, can in some cases ensure the onset of remission in multiple sclerosis (MS), which often occurs in childhood (up to 18 years) [12]. Synergy between micronutrients and vitamins. Vitamins for children Supradin Kids It is well known that vitamins are nutrients, their use (vitamin prophylaxis and vitamin therapy) is an integral part of neurodietology. The combination of vitamin or vitamin-mineral complexes with biologically active substances (omega-3 PUFAs, lecithin, choline) reflects a progressive way to optimize nervous functions, somatic health and vitamin provision of children. Ascorbic acid helps increase the body's resistance to stress and helps to successfully cope with its consequences. This substance is of great importance in the synthesis of hormones responsible for the stability and adaptation of the body to changing environmental conditions. Vitamin C helps activate thinking processes and is used by the body in the production of neurotransmitters and nerve cells. The combination of polyunsaturated fatty acids with antioxidant vitamins C and E allows you to prevent damage to the active component by oxidative processes and achieve maximum absorption. In recent years, there has been increased interest in the relationship between vitamin B12, folic acid and choline metabolism and cognitive development. Folic acid affects neuronal cell proliferation and differentiation of stem cells, slows down apoptosis, modifies DNA biosynthesis, and plays an important role in the biosynthesis of homocysteine and S-adenosylmethionine. Choline is thought to serve a similar role in brain development. S-adenosylmethionine is considered the main donor of methyl groups in various metabolic methylation reactions. Thus, choline and folic acid deficiency can lead to DNA hypomethylation, altering gene transcription. In addition, choline is a component of cell membrane phospholipids and a precursor to the neurotransmitter acetylcholine. Vitamin B12 plays an important role in axonal myelination and also protects neurons from degeneration. The synergism of the components makes it most effective to use rationally formulated vitamin-mineral complexes for children, rather than individual monocomponents. Supradin Kids Gel is intended for use in children aged three years and older. Contains B vitamins (B1, B2, B6), niacin, pantothenic acid, antioxidant vitamins (beta-carotene, C, E), vitamin D3. Beta-carotene is the most common and most effective provitamin A. Theoretically, one molecule of beta-carotene can be broken down into two molecules of vitamin A. However, in the body, beta-carotene is only partially converted into vitamin A, and the rest accumulates unchanged. Moreover, the proportion of beta-carotene converted into vitamin A in the body is controlled by vitamin A status, thereby avoiding toxicity caused by excess vitamin A in the body. It is a known fact that beta-carotene is not soluble in water, and its oil solutions have a very low concentration (no more than 0.1%). Therefore, the absorption of beta-carotene from tablet preparations and oil solutions significantly depends on the fat content in the diet and the state of the digestive system. The combination with lecithin significantly increases the bioavailability of beta-carotene. The use of beta-carotene in frequently ill children, along with a dose-dependent clinical effect, leads to an immunomodulatory effect, which manifests itself in a decrease in the level of T-lymphocytes and serum immunoglobulin A when stimulating the functional activity of phagocytic cells in peripheral blood [13]. Supradin Kids with Omega-3 and choline are sweet marmalade candies in the shape of fish and stars, which are intended for children from 3 years old. This is a multivitamin complex that contains Omega-3 and choline. In addition, cyanocobalamin is added to the complex. The presence of this vitamin in the complex is especially important for children following various types of diets. Supradin Kids Junior are sweet, colorful chewable tablets intended for children over 5 years old. Compared to the previous form, they additionally contain calcium, magnesium, choline, iron, zinc, manganese, cyanocobalamin, copper, folic acid, selenium, iodine, biotin, chromium. Microelements have high biological activity and participate in the basic redox processes of the body, various types of metabolism (protein, fat, carbohydrate, vitamin, mineral), gas exchange, heat exchange, tissue respiration, tissue permeability, immunobiological reactions. Taking part in these processes, trace elements are not limited to any one function. Zinc not only is related to the activity of the sex glands, but also affects protein, fat, carbohydrate and mineral metabolism. Copper and iron are involved in redox processes, and are also associated with the function of hematopoiesis. Iodine has a multilateral effect on the body. Iron was found in the body as part of more than 70 of enzymes and proteins different in its function. The disadvantage of iron in the body has a completely defined characteristic clinical picture: hypochromic anemia, myoglobindic atonia of skeletal muscles, increased fatigue and slight excitability, headaches, dizziness, depression, myoglobindic disadvantage of myocardiopathy, heart, atrophic glossitis, givinginuria. Copper takes part in nitrogen metabolism, part of the nitratedreductal complex. In the body - participates in processes that provide tissues with oxygen: the formation of hemoglobin and the formation of red blood cells. Copper is part of the ceruloplasmine of animals and humans, is the cofactor of enzymes of cytochromoxidase, polyphenol, di-, amino and ascorbinoxidase. Copper induces the formation of a superoxide ion-radical, which, in a reaction with hydrogen peroxide in the presence of trivalent iron, generates hydroxide radicals that go to the breakdown of pathological elements-detritus, inflammation products that mutated cells. Copper is involved in many physiological and pathological processes of the body and is contained in the mitochondria and microsomas (breathing, detoxification, gender reaction, oxidation of lysine and ascorbic acid-with excess of the latter there is a shortage of copper). Copper takes part in the synthesis of collagen and elastin, hemoglobin. The content of copper is very important for the function of vitamins A, E, P, PP, C, as well as stabilization of thiol groups. Copper provides the functioning of the desalation enzyme, which translates stearic acid into oleic and other polyunsaturated fatty acids. With a deficiency of copper, dysplasia of connective tissue, neurodegeneration and hypomoylinization of the brain and spinal cord, hypochromic anemia, and eczema develop. Selenium stimulates immunity in our body, is an antioxidant and has a protective effect on cytoplasmic membranes, preventing their damage and genetic disorders. It contributes to the normal development of the cell. Selenium, along with cobalt and magnesium, is a factor that counteracts a violation of the chromosomal apparatus. Selena ions activate mitochondria and microsomas, glutation-reductase, glutathione-peroxidase, cytochrome P450, participate in the synthesis of glycogen, ATP, the transmission of electrons from hemoglobin to oxygen, support the work of α-tocopherols, are an antidote against the transmission of electrons. heavy metals, including Mercury, silver, cadmium. Selenium deficiency occurs not only for low intake, but also with chronic intoxication with heavy metals, liver diseases, as well as in the treatment of phenylketonuria by parenteral and semi -synthetic nutrition. Currently, zinc has been identified in almost 200 enzymes that determine the course of various metabolic processes, including the synthesis and decay of carbohydrates, fats, proteins and nucleic acids. It has been established that zinc affects the function of the genetic apparatus, growth and division of cells, osteogenesis, keratogenesis, takes part in a non -immemed answer, affects the production of behavioral reflexes, and brain development [14]. Iodine plays an active role in the biosynthesis of hormones. He participates in the formation of thyroid hormones - thyroxine and triiodothyronine. Up to 90% of organic iodine circulating in the blood falls on the share of thyroxine. This hormone controls the state of energy metabolism, the intensity of the main metabolism and the level of heat production. It actively affects the physical and mental development, differentiation and maturation of tissues, is involved in the regulation of the functional state of the central nervous system and the emotional tone of a person. In addition to severe forms of mental retardation, iodine deficiency determines a decrease in the intellectual potential of the entire population living in the zone of iodine failure. Studies performed in recent years in different countries of the world have shown that the average indicators of the mental development of the population (IQ index) living in the regions of iodine deficiency, significantly (15–20%) lower than those in the regions without iodine deficiency. Supradin Kids Mishka - marmalade cubs, are intended for children from 11 years old. This complex contains vitamins in doses recommended for school -age children, and is a basic complex for the prevention of various pathological conditions. The composition of the complex includes: vitamins A, C, D3, B6, B12, Nicotinamide, Biotin, Folic acid, vitamin E. Dosage mode of vitamin-mineral complexes of the Supradin line is presented in table 1. The conclusion if the child does not receive the necessary set nutrients, a mechanism is activated that increases the level of activity of a number of hormones, in particular cortisol, which leads the nervous system to a state of excitation, which prevents the normal assimilation of the educational material. In children, especially for early school age, the mechanisms of self -regulation and compensation are not fully developed, as a result, the child feels tired or, conversely, tense and nervous, which leads to problems with performance and behavior, depletion of adaptive reserves. Different forms of vitamin complex of Supradin KIDS contain vitamins, macro- and trace elements in doses in accordance with the age-related dietary daily need of the child's body. The developed marmalade forms contribute to the development of an independent desire for a healthy lifestyle in the child and increase compliance. The components of this vitamin complex not only strengthen the child’s health, but also improve cognitive functions - memory and attention. Literature 1. Shikh E.V., Ilyenko L.I. Clinical and farmacological aspects of the use of vitamin-mineral complexes in pediatrics: Textbook. M.: Publishing House Medical Practice-M, 2008. 96 p. 2. Anett Nyaradi, Jianghong Li, Siobhan Hickling et al. The Role of Nutrition in Children's Neurocognitive Development, From Pregnancy Through Childhold // Frontiers in Human Neuroscience. 2013. March 26. 3. Germano M., Meleo D., Montorfano G. et al. Plasma, Red Blood Cells Phospholipids and Clinical Evalving afterga Omega-3 Supplement in Children with Attend Hyperaactivity Disorder (ADHD) // Nutr. Neurosci. 2007. Vol. 10 (1–2). P. 1–9. 4. Liu PJ, Ma F. PolyunsatUrated Fatty Acids and Attendation-Deficit Hyperaactivity Disorder // Zhongguo Dang Dai Er Ke Za Zhi. 2009. Vol. 11 (9). P. 783–785. J. Pediatr. 2010. Vol. 169 (2). P. 149–164. 6. Gromova O.A., Torshin I.Yu., Egorova E.Yu. Omega-3 PNSK and cognitive development of children // Pediatrics, practical medicine. 05 (11). 7. Mcnamara Rk, Able J., Jandacek R. et al. Docosahexaenoic Acid Supplementation Incresses Prefrontal Cortex Activity Sustained Attenation in Healthy Boys: A Placebo-Controlled, Dose-Ranging, Functional Magnet IC Resonance Imaging Study // Am. J. Clin. Nutr. 2010. Vol. 91 (4). P. 1060–1067. 8. Spahis S., Vanasse M., Belanger Sa et al. Lipid Profile, Fatty Acid Composition and Pro-and Anti-Oxidant Status in Pediatric Patients with Attendation-Deficit/Hyperaactivity Disorder // Prostaglandins Leukot. Essent. Fatty Acids. 2008. Vol. 79 (1–2). P. 47–53. 9. Barbeau A. Lecithin in Neurological Conditions // N. English. J. Med. 1978. Vol. 299. P. 200–201. 10. Barbeau A. Emering Treatments: Replaceement Therapy with Choline or Lecithin in Neurological Diseases // Can. J. 11. Studenikin V.M., Balkanskaya S.V., Silkovsky V.I. The influence of lecithin on the neurological status of children // attending physician. 12. Studenikin V.M. Polyvitamin preparation with lecithin: use in children's neurology // attending physician. 2003. No. 6. S. 56–57. 13. Plaksin V.A. The effect of synthetic beta-carotene on clinical and immunological parameters of often sick children: abstract. dis. . Ph.D. honey. Sci. Arkhangelsk, 1998. 14. Blinkov I.L., Starodubtsev A.K., Suleimanov S.Sh., Shikh E.V. Microelements. Brief clinical encyclopedia. Khabarovsk, 2004, S. 211.
Reasons for appearance
As mentioned above, brain damage and structural defects are to blame for underdevelopment of the brain. There are the following main groups that determine the presence of a control system:
- hereditary diseases (chromosomal and genetic);
- intrauterine infections - toxoplasmos, rubella and others that negatively affect the fetus;
- maternal consumption of toxic substances, alcoholic beverages, strong drugs, radiation, smoking;
- fetal prematurity;
- problems during childbirth and in the first months of a child’s life - oxygen starvation, mechanical head injuries, infectious diseases;
- lack of normal upbringing, training and socialization, the impossibility of full-fledged brain function as a result of this;
- unknown etiology.
Causes
>This pathology is not a separate disease, but an intermediate state between normal and dementia. MCI is provoked by pathological processes in the central nervous system:
- Vascular diseases: multi-infarction conditions, cerebral infarctions, combined vascular and hemorrhagic brain damage, chronic cerebral ischemia. Cognitive impairment can be observed during the course of the underlying disease and as consequences;
- Neurodegenerative diseases, which include: Huntington's chorea, Parkinson's disease, senile dementia of the Alzheimer's type, progressive supranuclear palsy and dementia with Lewy bodies. Cognitive disorders precede the development of the main symptoms;
- In demyelinating pathologies, MCI manifests itself in the early stages of multiple sclerosis, progressive paralysis, and progressive multifocal leukoencephalopathy. Cognitive impairment increases as the underlying disease progresses;
- Traumatic brain injuries can cause permanent or transient cognitive impairment during the post-traumatic injury period. The clinical picture depends on the nature, depth, diffuseness or locality of the lesion;
- Dysmetabolic encephalopathies lead to metabolic disorders and dysfunction of internal organs. This provokes dysfunction of the central nervous system. Hypoglycemic, renal, disteroid, and hepatic disorders can cause cognitive impairment. Hypoxic encephalopathy, lack of protein and vitamin B, poisoning;
- If cognitive impairments are provoked by neuroinfections, then the disorder manifests itself in the early stages with Creutzfeldt-Jakob disease, HIV-associated encephalopathy, acute and subacute meningoencephalitis. In the latter case, the disorders are a consequence of the infectious process;
- With brain tumors, pathology is observed in the initial stages. Symptoms depend on the location of the tumor.
Development mechanism
The pathogenesis of the disorder is extremely diverse and depends on the underlying disease. In old age, the mechanisms of aging are decisive.
Based on cerebrovascular disorders, mild cognitive impairment develops in 68% of cases. In this case, MCI is caused by circulatory failure due to pathological changes in the cerebral vessels. The second most common condition is atrophy, that is, degenerative damage to brain tissue. About 13-15% of elderly and old patients suffer from anxiety and depressive disorders.
Signs of mild UO
Mental underdevelopment with decreased intelligence, congenital or acquired, can be noticed in very young children, three years old. However, the diagnosis is made no earlier than the child reaches seven years of age.
Signs of mental retardation in newborns are almost impossible to detect, especially its mild form. But then this will manifest itself in developmental delays and difficulties in adapting to kindergarten. It is difficult for a child to communicate with peers, find a common language with them, maintain a daily routine, master new skills, and absorb knowledge. He cannot sit in one place, gets tired quickly, does not show any desire to understand the world, and is inattentive.
A child may have a similar but passing problem - mental retardation. The difference is that a child with mental retardation is not always able to learn a new skill, while a child with mental retardation still learns it after several repetitions.
This is why it is so important to detect the symptoms of MR early in order to begin corrective measures immediately. Here they are:
- Abnormal motor development. The baby begins to hold his head up late, tries to sit up, stand up, and walk. His grasping reflex is impaired, he is unable to hold a toy, and a little later, a spoon.
- The processes of excitation and inhibition are unbalanced - the baby is overly impulsive, irritable, or excessively lethargic and slow.
- Belated babble. He begins to speak with a significant delay or there is no speech at all. The child is not able to speak coherently, as it is difficult for him to construct a sentence. He does not understand what is being said to him, so he cannot fulfill even basic requests.
- Poor emotional-volitional sphere, self-isolation, lack of interest in what is happening around.
- There is no interest in toys, their incorrect use prevails, preference is given to primitive games.
- There is no abstract thinking, that is, logic, mathematical and creative abilities.
A few words should be said about emotions: the child experiences grief and joy, hostility and sympathy, is sad and happy, but all this is expressed very weakly, not in many ways.
Outwardly, such a child is no different from his peers. But his inability to concentrate properly leads to learning difficulties.
Children with a mild degree of ID are afraid of a change of environment and are highly dependent on their parents and educators. Difficulties in recognizing emotions create problems with communication, so kids withdraw into themselves. But it is also possible that they draw attention to their person in different ways, often very awkward.
Such individuals are well aware that they are different from healthy people, so they take measures to conceal their problem. Many people manage to gain self-care skills, although this happens more slowly than their peers. The school period is especially difficult for them, since writing, reading and mathematics are difficult for them.
Features of childhood dementia
Preschool age only forms a personality, which is characterized by many factors: developmental characteristics, temperament, individuality.
Only after the child goes to school can parents identify a developmental disorder. Such children practically do not master the program. It is not possible to attract the attention of oligophrenics and fix it on something. Difficulties arise with memorization and retelling—children suffering from ID are unable to retain received information in memory for a long time.
A “special” student usually does not understand the essence of the task and does not grasp the connections between things and phenomena. It is very easy to intimidate him in such a situation: you just have to shout, and the psychological trauma that follows the stress is inevitable.
Depending on the environment, such a child can develop into two completely different personality types:
- kind and sympathetic, ready to help at any moment, vulnerable and warm-hearted;
- embittered and aggressive, who, having no desires and feelings of their own, are subject to the negative influence of others.
A practicing psychotherapist shared the story of a boy who was doomed to mental illness while still in utero development. A dysfunctional mother carried a child in violation of all acceptable rules: she smoked, drank alcoholic beverages, and took psychotropic drugs. After the birth of the child, he was deprived of proper attention.
After some time, the visiting nurse noticed some mental underdevelopment of the baby: he could not hold his head up on his own and did not make any sounds. Thanks to the prompt and coordinated work of medical workers, the boy was saved. And at the moment it has practically adapted to modern living conditions.
A predisposition to mental illness or unacceptable behavior of a pregnant woman is a reason to warn her about the possible dementia of the unborn child.
However, a loving and caring mother who leads a healthy lifestyle and has absolutely no prerequisites for the occurrence of mental pathologies can also face the problem of dementia in her child.
Having noticed the first alarm bells, which are a definite reason for consultation, you must immediately contact a qualified specialist. This will give you the opportunity to deeply adapt your baby to society before the moment of his socialization.
Cognitive impairment in children and adolescents with consequences of traumatic brain injury.
When comparing the state of visual and auditory-verbal memory in children and adolescents in the long-term period of severe TBI, it was found that adolescents have more pronounced and persistent impairments in auditory-verbal memory than children, while visual memory disorders did not depend on age. According to the authors, this is due to the fact that the underlying parts of the cortex responsible for visual memory are mainly formed by the age of 6, while the development of brain structures providing auditory-verbal memory continues [28].
Attention deficits in the long-term period of TBI in children and adolescents are often reported by parents and teachers. Attention deficits affect both their daily behavior and learning. It has been established that the greatest difficulties in children and adolescents with TBI are caused by performing long tasks that require constant concentration of attention. External events and their own thoughts prevent them from concentrating. At school, they cannot follow long-term instructions, and at home, where activities are often less structured than at school, parents note that their child cannot engage in one task for a long time [34].
Post-traumatic epilepsy is a serious neurological consequence of TBI and often aggravates the manifestations of cognitive impairment. It was shown that the development of symptomatic post-traumatic epilepsy was observed in 5.7% of patients aged 4 to 14 years and occurred during the first year after suffering a closed moderate or severe TBI [16].
Among the examined adolescents with consequences of TBI, 37% had latent epileptiform activity on the EEG [14,16,39]. In recent years, evidence has accumulated indicating the pathogenic effect on the central nervous system of long-term persistent epileptiform activity, even in the absence of epileptic attacks. It has been established that latent epileptiform activity has a negative impact on distributed and sustained attention, indicators of visual and kinesthetic memory, as well as motor skills and the coordination sphere, which indicates the need for long-term dynamic observation of adolescents who have suffered a TBI by a neurologist with repeated EEG studies [14, 16.39].
Emotional and behavioral disorders in children and adolescents in the long-term period
TBIs are difficult to differentiate because they are closely related. Traumatic
cerebrovascular disease is characterized by a predominance in its picture of pronounced exhaustion and
irritability, sometimes reaching affective explosiveness; against this background it is often
hysterical, neurasthenic, hypochondriacal or depressive symptoms occur. Often
motor disinhibition, impulsivity, and inability to adhere to
instructions given by adults, inability to cope with certain tasks, refusal
from their implementation. Residual effects after traumatic brain injuries serve
a predisposing factor when a child or adolescent finds himself in difficult life circumstances to the emergence of psychogenic or neurotic disorders, are a favorable basis for the pathological formation of personality. Emotional and behavioral disturbances in the long-term period of TBI lead to difficulties in social contacts and relationships with peers [13,16,24,27,37].
Diagnostics
Mental development disorders are difficult to detect at an early stage. However, such diagnosis is extremely necessary for early correction and compensation of the detected defect.
The diagnosis of “mental retardation” is made on the basis of special methods that allow assessing the intellectual level of an individual. Sometimes specialists use neuropsychological diagnostics, which allows us to determine the level of development of higher mental functions, as well as assess the child’s potential.
A correctly made diagnosis makes it possible to timely develop corrective methods to eliminate the pathology and treat it. In this case, the doctor must make sure that the little patient does not have signs of progression of underdevelopment or signs of more serious mental illnesses (schizophrenia, schizoaffective disorder, etc.).
It is also important to determine that the patient’s condition is not pedagogical neglect. This often happens to children who have lost their parents and were sent to an orphanage. There they can be subjected to harsh treatment, bullying, violence, etc. But if the child changes the situation for a better one - he is adopted, he lives and is raised in a normal family, then his condition returns to normal.
Non-dementia cognitive disorders: clinical aspects
Cognitive impairment (CI) accompanies most neurological diseases involving the brain, since the predominant part of the cortex is involved in cognitive activity. The brain is also a target organ in many somatic diseases, especially in pathologies that are widespread in old age. An increase in human life expectancy is naturally accompanied by an increase in the number of patients with cognitive disorders. Thus, currently 47 million people worldwide suffer from CI of varying severity, and by 2050 this figure will approach 130 million people [1]. Timely identification of cognitive decline, clarification of its clinical features, qualitative and quantitative characteristics will help the practicing neurologist in the topical and nosological diagnosis of the disease. For an internist, the rate of progression of cognitive disorders can be an important element in monitoring the effectiveness of treatment measures and choosing therapeutic tactics for somatic pathology. CIs reduce the patient's adherence to therapy and worsen the prognosis of both neurological and somatic diseases, and have a negative impact on the quality of life not only of the patient, but also of his immediate relatives. All this allows us to consider CI an important problem of modern medicine. Early diagnosis and early treatment are especially important, since some cognitive impairment may be reversible, and treatment options in the advanced stage of cognitive impairment are very limited.
According to the latest revision of the international recommendations for the diagnosis of mental disorders (Diagnostic and statistical manual of mental diseases - DSM-V), cognitive disorders include a decrease, compared with the premorbid level, in one or more higher brain functions that provide the processes of perception, storage, transformation and transmission of information [2].
There are several classifications of cognitive disorders, the simplest of which, and very important in practical terms, is based on the severity of the impairment. There are severe CIs - dementia and non-dementia CIs [3]: subjective, mild (moderate) and moderate.
Criteria for mild cognitive impairment (MCI):
- a decrease in cognitive abilities compared to the average age and educational level, which is reflected in the patient’s complaints or is not subjectively realized;
- no changes in integral indicators of cognitive functions according to general screening scales (for example, the Brief Mental Status Assessment Scale);
- the absence of any disturbances or difficulties in daily functioning, including its most complex forms.
Extensive neuropsychological testing may reveal mild changes in a number of tests. Abroad, cognitive decline that does not reach a moderate degree is designated as premild cognitive impairment.
In addition to what is expected, foreign literature describes subjective cognitive decline - the presence of complaints about cognitive dysfunction: increased forgetfulness, decreased concentration, increased fatigue during mental work, difficulty finding the right word in a conversation. Complaints about the experienced cognitive decline are very significant for patients and force them to seek medical help, but not a single neuropsychological test confirms objective cognitive decline; there are no changes during a neuropsychological examination. It is likely that among patients with subjective CI there are both patients with affective disorders (anxiety-hypochondriacal, depressive) and patients at an early stage of the dementing process.
In 2014, diagnostic criteria for subjective cognitive decline (SCD) were proposed [4]:
- patient complaints about a persistent deterioration in mental performance compared to the past, which arose for no apparent reason;
- the absence of any deviations from the age norm according to cognitive tests used to diagnose Alzheimer's disease and other dementing diseases;
- cognitive complaints are not associated with any established diagnosis of neurological, psychiatric disease or intoxication.
Currently, SCS is considered as the earliest manifestation of Alzheimer’s disease, when the symptoms are extremely difficult to objectify [5], but in some patients corresponding changes are detected according to positron emission tomography and beta-amyloid and tau protein are detected in the cerebrospinal fluid [6, 7] . Among patients with SCS, the greatest attention should be paid to a decrease in tolerance to mental stress, which may be a reflection of the process of depletion of the compensatory capabilities of the brain (cerebral cognitive reserve) under special conditions: in a state of fatigue or a stressful situation.
The term and diagnostic criteria for mild cognitive impairment (MCI) syndrome were proposed in 1997 by R. Petersen et al. [8]. Currently, the following diagnostic criteria are used for the syndrome of “mild neurocognitive disorder”, according to the American Classification of Mental Disorders V revision [9].
- A slight decrease compared to the previous level of one or more cognitive functions (attention, executive functions, memory, speech, praxis, gnosis, social intelligence), which is confirmed by patient complaints, information from third parties, including the attending physician; neuropsychological tests or independent clinical assessment.
- CIs do not deprive the patient of independence in daily activities (including complex activities, such as financial transactions or taking medications). The patient remains independent, but daily activities may require greater effort than before or the use of special coping strategies.
- CIs are not caused by delirium.
- CIs are not associated with other mental disorders such as depression or schizophrenia.
Depending on the nosological affiliation, there are 4 clinical variants of MCI syndrome.
- The monofunctional amnestic type with predominant memory impairment is thought to be associated with the prodrome of Alzheimer's disease;
- The monofunctional non-amnestic type with preserved memory and impairment of any other cognitive function is caused by non-Alzheimer's cerebral pathology. Dyscirculatory encephalopathy is characterized by impaired regulation of voluntary activity; for dementia with Lewy bodies - disturbances of spatial praxis and/or gnosis; for frontotemporal degeneration - behavioral and/or speech disorders.
- Multifunctional with impairment of several cognitive functions, including memory impairment, usually transforms over time into dementia of the Alzheimer's type.
- Multifunctional patients without memory impairment have a low likelihood of developing dementia of the Alzheimer's type; the cause of MCI is another cerebral pathology [10].
Features of diagnosis of non-dementia CIs
Assessment of the patient's cognitive functions is an integral part of the clinical examination of neurological status. Diagnosis of cognitive disorders is based on complaints from patients and/or their relatives, results of neuropsychological research methods and clinical assessment of the patient’s daily activities. Both patients with the amnestic type of MCI and patients with emotional-behavioral disorders (depression, apathy or affective lability) can complain of forgetfulness and memory loss, so it is necessary to carefully examine the emotional-behavioral sphere. To objectify emotional and behavioral disorders, you can use special questionnaires that the patient fills out (Beck Depression Scale, Hospital Anxiety and Depression Scale, Spielberger Anxiety Scale), or rating scales by which the severity of symptoms is assessed by the attending physician (for example, the Hamilton Depression Scale) [11 ]. It is necessary to ask patients about the medications they are taking, since many medications can impair cognitive function (central anticholinergics, barbiturates, benzodiazepines, tricyclic antidepressants, typical antipsychotics). In case of CI, these medications should be discontinued.
Patients with the subcortical-frontal (non-amnestic) variant of MCI (for example, vascular cognitive disorders) have relatively intact memory and rarely complain of forgetfulness. Their predominant complaints are headaches, non-systemic dizziness, noise and heaviness in the head, increased fatigue, sleep disturbances, primarily associated with existing emotional and movement disorders. Patients can describe their condition: “the head feels like cast iron”, “the head feels like a dust bag hit”, etc., and upon detailed questioning it turns out that these unpleasant sensations interfere with concentration or cause a feeling of fatigue, reducing the tolerance of intellectual stress. Intellectual work requires significantly more time than before; patients get tired quickly and are easily distracted from the work they have started. In fact, such complaints are nothing more than a kind of subjective equivalent of a lack of concentration. The cognitive status of such patients reveals a decrease in concentration and rate of cognitive activity (bradyphrenia), and a violation of frontal control functions (planning and control).
Screening tests such as the Mini-Cog, Mini-Mental State Examination, and clock drawing test are not sensitive enough for nondemented cognitive impairment and may produce false-negative results. The Montreal Cognitive Function Assessment Scale is a more sensitive method for non-dementia disorders, but it cannot be considered optimal.
A necessary step in determining the severity of CI and further approaches to patient management is the distinction between MCI and mild dementia. The most important part of this assessment is to answer the question to what extent CIs influence everyday life. At the stage of MCI, patients may experience difficulties in complex and new activities (for example, when trying to master a computer or other equipment that they have never had to deal with before), but can work in the same volume and quality, fully retain their professional and social competence, fulfill their usual role in the family and society, and maintain their hobbies and interests. The diagnosis of dementia is legitimate if there are difficulties in the patient’s usual activities, the need for help or help from relatives is formed, and criticism and adequacy of the assessment of the situation decreases.
Different methods are optimal for diagnosing amnestic and non-amnestic variants of MCI: for amnestic variants, it is recommended to use methods based on memorizing and reproducing a list of words or retelling the text; and to identify subcortical-frontal disconnection with impaired regulation of voluntary activity, methods that assess the rate of mental activity and concentration of attention (for example, the “symbols and numbers” test) [11].
A comprehensive neuropsychological examination using standard tests for memory, executive functions, attention, is labor- and time-consuming and is not always feasible in clinical practice. For a screening study of cognitive functions and topical diagnosis of their disorders, the 3-CT test (three cognitive neuropsychological tests, O. S. Levin, 2010) can be used [12]. A decrease in the number of semantically mediated associations is one of the earliest signs of approaching dementia, which is most characteristic of the manifestation of Alzheimer's disease associated with dysfunction of the temporo-limbic system. When subcortical-frontal dysfunction predominates (for example, with cerebrovascular pathology), the number of phonetically mediated associations decreases faster than the number of semantically mediated associations.
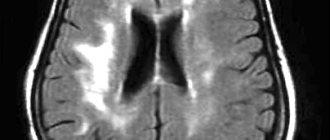
For nosological diagnosis and establishment of the cause of MCI, clinical, laboratory and instrumental research methods are required. It is especially important to make a timely nosological diagnosis in case of potentially reversible cognitive disorders associated with complications of various somatic and endocrine diseases (hypothyroidism, deficiency of vitamin B12 and folic acid, renal and liver failure, respiratory failure, chronic hypoxia of a different nature, etc.), volumetric process, impaired liquor dynamics [13–15]. Neuroimaging (preferably magnetic resonance imaging of the brain) makes it possible to diagnose the neurosurgical pathology that is the cause of CI (for example, a brain tumor, liquorodynamic disorders, etc.); is mandatory for a combination of cognitive and other neurological (motor, sensory) disorders, with a progressive course of CI. Neuroimaging also allows for differential diagnosis of the main nosological variants of MCI. MCI associated with Alzheimer's disease is characterized by atrophy of the hippocampus and temporoparietal regions of the brain. In the degenerative process with Lewy bodies, expansion of the posterior horns of the lateral ventricles is determined. Frontotemporal degeneration is characterized by the localization of the atrophic process mainly in the frontal and/or anterior temporal lobes of the brain. Neuroimaging markers of vascular cognitive impairment are cerebral infarctions and leukoaraiosis [16–18].
Thus, the lack of effective treatment for cognitive disorders at the stage of dementia requires a modern neurologist to pay increased attention to non-dementia forms of CI, deep knowledge of clinical and neuropsychological diagnostic methods, and analysis of cognitive disorders that allow identifying the problem at the earliest stages. Approaches to the treatment of such patients should be individual and comprehensive, taking into account the pathogenetic factors of cognitive deficits in each specific case.
Literature
- Societies can both grow old and lower dementia burden // Lancet Neurol. 2015. Vol. 14. No. 10. ID967.
- Diagnostic and statistical manual of mental diseases. V ed. (DSM-V). London: American Psychiatric Association, 2013.
- Yakhno N. N., Zakharov V. V., Koberskaya N. N., Mkhitaryan E. A., Grishina D. A., Lokshina A. B., Savushkina I. Yu., Posokhov S. I. “Premeditated” (subjective and mild) cognitive disorders // Neurological Journal. 2017; 22 (4): 198–204. DOI: https://dx.doi.org/10.18821/1560–9545–2017–22–4–198–204.
- Jessen F., Amariglio RE, van Boxtel M., Breteler M., Ceccaldi M., Chételat G. et al. Subjective Cognitive Decline Initiative (SCD-I) Working Group. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer's disease // Alzheimer's Dement. 2014; 10(6):844–852.
- Amariglio RE, Becker JA, Carmasin J, Wadsworth LP, Lorius N, Sullivan C et al. Subjective cognitive complaints and amyloid burden in cognitively normal older individuals // Neuropsychologia. 2012; 50(12):2880–2886.
- Perrotin A., Mormino EC, Madison CM, Hayenga AO, Jagust WJ Subjective cognition and amyloid deposition imaging: A Pittsburgh Compound B positron emission tomography study in normal elderly individuals // Arch. Neurol. 2012; 69(2):223–229.
- Striepens N., Scheef L., Wind A., Popp J., Spottke A., Cooper-Mahkorn D. et al. Volume loss of the medial temporal lobe structures in subjective memory impairment // Dement. Geriatr. Cogn. Discord. 2010; 29 (1): 75–81.
- Petersen RS, Smith GE, Waring SC et al Mild cognitive impairment: clinical characterization and outcome // Arch Neurol. 1999, Mar; 56(3):303–308.
- American Psychiatric Association. Diagnostic and statistical manual of mental diseases. 5th edition (DSM–V). Washington DC, London, England; 2013. 947 p.
- Petersen RC Mild cognitive impairment as a diagnostic entity // J Intern Med. 2004, Sep; 256(3):183–194.
- Parfenov V. A., Zakharov V. V., Preobrazhenskaya I. S. Cognitive disorders. M.: Remedium, 2014.
- Diagnosis and treatment of cognitive impairment and dementia: method. recommended / O. S. Levin, E. E. Vasenina. M.: MEDpress-inform, 2015. 80 p.
- Vizilo T. L., Vlasova I. V. Clinical and neurological characteristics of patients with traumatic encephalopathy // Polytrauma. 2006. No. 1. P. 68–72.
- Vizilo T. JL, Schmidt V.P., Mikhailov V.P. et al. Clinical and functional features of various stages of atherosclerotic discirculatory encephalopathy // Neurological Journal. 2000. 1. pp. 17–20.
- Subbotin A.V., Getmanenko I.M., Semenov V.A. The effectiveness of psychological methods for diagnosing cognitive impairment in patients with vascular diseases of the brain in the early stages of the disease // Medicine in Kuzbass. 2011. No. 3. P. 45–48.
- Galvin JE, Price JL, Yan Z. Resting bold fMRI differentiates dementia with Lewy bodies vs Alzheimer disease // Neurology. 2011; 76(21):1797–1803.
- Debette S., Beiser A., DeCarli C. et al. Association of MRI markers of vascular brain injury with incident stroke, mild cognitive impairment, dementia, and mortality: the Framingham Offspring Study // Stroke. 2010; 41(4):600–606.
- O'Brien JL, O'Keefe KM, LaViolette PS et al. Longitudinal fMRI in the elderly reveals loss of hippocampal activation with clinical decline // Neurology. 2010; 74 (24): 1969–1976.
T. L. Vizilo1, Doctor of Medical Sciences, Professor A. D. Vizilo
Federal State Budgetary Educational Institution of Higher Education Kemerovo State Medical University, Ministry of Health of the Russian Federation, Kemerovo
1 Contact information
Non-dementia cognitive disorders: clinical aspects / T. L. Vizilo, A. D. Vizilo For citation: Attending physician No. 5/2019; Page numbers in the issue: 10-12 Tags: elderly, old age, brain, mental performance
Prevention and treatment
In order to prevent the development of mental retardation in the womb, pregnant women who have an unfavorable history (physiological indicators, predisposition) are recommended to undergo a more thorough examination. Doctors place women under special observation who suffered from viral diseases during pregnancy.
Birth injuries received by newborns, as well as infectious diseases they suffered at an early age, can lead to brain damage.
A child with mild mental retardation has the opportunity to develop and learn within the limits of his biological capabilities. This pathology is incurable, but its timely and competent correction will make it possible for such a person to become a full-fledged member of society, albeit with limited abilities. A special role in this case is played by the environment and perception. There is no doubt that such people require increased attention.
Mental retardation requires close contact with loved ones, teachers, doctors, and psychologists. The doctor selects specialized institutions for children with mental development problems taking into account the child’s capabilities and abilities. Additionally, the psychotherapist can prescribe medication support using pharmacological drugs. Medical and educational measures and labor training for the mentally retarded show good results.
It is always important to remember that any mental illness is not a death sentence. The main thing is to contact a specialist in time, who will help make your stay in society as comfortable and fruitful as possible for the patient.
In the case of mild oligophrenia, experts give a relatively favorable prognosis. This applies to cases not burdened with concomitant psychopathological and somatoneurological disorders. People with such deviations are quite capable of mastering certain types of professions, can adapt to independent living, and even create families.
Cognitive disorders without dementia: classification, main causes and treatment
The article gives a definition, classification, diagnostic criteria, principles of pathogenetic and symptomatic treatment of non-dementia cognitive impairment. The possibilities of using the dopaminergic and noradrenergic drug piribedil (Pronoran) for the treatment of mild and moderate cognitive impairment that does not reach the severity of dementia are discussed in detail.
Table 1. Cognitive functions (according to DSM-V)
Table 2. DSM-V Diagnostic Criteria for Moderate and Severe Neurocognitive Disorder
Table 3. Classification of cognitive impairment by severity [5]
Table 4. Diagnostic criteria for depression according to the International Classification of Diseases, 10th revision
Rice. 1. Increase in the total score on the Montreal Cognitive Function Assessment Scale during therapy with Pronoran (group A), piracetam (group B), ginkgo biloba (group C) and vinpocetine (group D)
Rice. 2. Dynamics of subjective neurological symptoms during therapy with Pronoran (p < 0.05)
About 90% of the human cerebral cortex is involved in cognitive activity. Therefore, most neurological diseases involving the brain are accompanied by some kind of cognitive impairment. Usually they are combined with changes in the emotional and behavioral sphere, being united by a common pathomorphological and pathophysiological substrate. A practicing neurologist needs to assess the presence and characteristics of cognitive and other neuropsychiatric disorders and take this information into account when syndromic, topical and nosological diagnosis of nervous system diseases.
Cognitive impairment is no less important for clinicians in other medical specialties. The target organ of many somatic diseases, in particular diseases of the cardiovascular system, which are widespread in old age, is the brain. Assessing the state of the brain in this case is extremely important for assessing the effectiveness of controlling the underlying disease and choosing therapeutic tactics.
The presence of cognitive impairment has an extremely negative impact on the quality of life of the patient and his immediate family, making it difficult to treat concomitant diseases and carry out rehabilitation measures. Therefore, timely diagnosis and the earliest possible start of treatment for existing cognitive disorders are very important.
Definition and classification of cognitive impairment
According to the latest revision of the international recommendations for the diagnosis of mental disorders (Diagnostic and statistical manual of mental diseases - DSM-V), cognitive disorders include a decrease compared to the premorbid level of one or more higher brain functions that provide the processes of perception, storage, transformation and transmission of information (Table 1) [1].
It is important not only to establish cognitive decline and conduct its qualitative analysis, but also to quantify the severity of existing disorders. It is known that some medications that are effective for severe cognitive impairment (dementia) have a much lesser effect on cognitive impairment that does not reach the level of dementia. This is probably due to various neurochemical changes that are noted in the early and later stages of the pathological process [2–4].
Dementia (or, according to DSM-V, frank neurocognitive disorder) is characterized by significant impairment of higher brain functions that interfere with the patient's normal functioning. In dementia, due to severe cognitive impairment, the patient is at least partially deprived of independence and needs outside help in the most ordinary life situations (for example, when navigating the area, shopping in a store) (Table 2) [1].
In the treatment of patients with severe cognitive disorders, priority should be given to drugs with a symptomatic effect, which can reduce the severity of the disorders and thereby improve the quality of life of patients and their relatives.
The diagnosis of non-dementia cognitive impairment is established in cases where, despite the existing intellectual defect, the patient maintains independence in everyday life. In this case, the patient may experience some difficulties in mental work, which is reflected in complaints. However, the patient overcomes these difficulties without resorting to outside help (Table 2) [1]. In the treatment of patients with non-dementia cognitive disorders, one should not only use symptomatic therapy, but also carry out measures to prevent dementia.
According to the classification of academician N.N. Yakhno, non-dementia cognitive disorders are divided into mild and moderate (Table 3) [5]. At the same time, patients with moderate impairments may experience difficulties in the most complex and unusual activities for the patient. At the same time, patients with mild impairments are completely independent and independent in all types of activities, including the most complex ones.
In recent years, neurologists, psychiatrists and representatives of other neurosciences have been paying increasing attention to an even earlier stage of cognitive failure - the so-called subjective cognitive impairment. The formulation “subjective cognitive impairment” (subjective memory impairment, cognitive complaints) is currently widely used both in the scientific literature and in everyday clinical practice as an independent diagnosis. This diagnosis is made if there are cognitive complaints, while the results of objective cognitive tests remain within the age norm.
Patients may complain of increased forgetfulness, decreased concentration, increased fatigue during mental work, and sometimes difficulty finding the right word in a conversation. These complaints represent a very pressing problem for the patient, which can serve as an independent or main reason for contacting a doctor. At the same time, the use of standard cognitive tests does not reveal any significant deviations from accepted standards. Patients with subjective cognitive disorders retain full independence in everyday life. Cognitive difficulties are also invisible from the outside: relatives, colleagues and other people always assess the patient’s cognitive abilities as completely intact.
The following international diagnostic criteria (2014) for the syndrome of subjective cognitive impairment are currently known [6]:
- patient complaints about a persistent deterioration in mental performance compared to the past, which arose for no apparent reason;
- the absence of any deviations from the age norm according to cognitive tests used to diagnose Alzheimer's disease and other dementing diseases;
- cognitive complaints are not associated with any established diagnosis of neurological, psychiatric disease or intoxication.
The dissociation between patient complaints, test results, and patients' daily functioning raises legitimate questions about the true nature of the complaints. These questions are still far from being resolved and are being actively studied. At the current stage of scientific knowledge, it seems that patients with subjective cognitive impairment represent a very heterogeneous group, which includes both patients with the earliest stages of the dementing process and patients with anxiety-depressive and hypochondriacal spectrum disorders.
In some cases, the predominantly subjective nature of disorders is explained by methodological difficulties in objectifying cognitive status. There are currently no generally accepted recommendations for the use of specific techniques to diagnose dementia or non-dementia cognitive impairment. Therefore, in practice, tests of varying degrees of sensitivity, specificity and reproducibility are used. The use of tests with low sensitivity will lead to underdiagnosis of mild and moderate cognitive impairment and to overdiagnosis of so-called subjective impairments.
The diagnosis of “subjective cognitive impairment” is often given to patients with a high premorbid intellectual level. Cognitive functions reduced as a result of cerebral disease in comparison with the individual norm for a long time will formally be within the limits of the average statistical standard. Consequently, cognitive decline may remain formally unconfirmed for a long time, in other words, “subjective.”
Cognitive complaints may be caused by anxiety and depressive disorders in the absence of organic cerebral disease. Thus, patients with high levels of anxiety will be overly bothered by minor situational forgetting. In this case, the reason for contacting a doctor becomes such widespread complaints, including among healthy people, as “I don’t remember why I came into the room,” “I don’t remember what I put where,” “I didn’t recognize a person I knew or didn’t remember him.” surname" etc.
However, the greatest research interest in a heterogeneous group of patients with subjective cognitive impairment is caused by patients with decreased tolerance to mental stress, since this pathological phenomenon may indeed be the earliest clinical manifestation of the dementing process. As is known, at the very initial stages of a neurodegenerative or cerebrovascular disease, clinical symptoms may be absent, despite the presence of organic brain damage, sometimes significant. This is explained by the so-called cerebral reserve, that is, the compensatory capabilities of the brain. The presence of such capabilities will lead to false negative test results. At the same time, in everyday life the patient may experience difficulties under special conditions when the cerebral reserve is depleted and cannot overcome the difficulties that arise, for example, in a state of fatigue or emotional stress. Currently, the world is actively developing the “intelligent treadmill” methodology. It will assess the degree of tolerance to increased mental stress, which may decrease before the development of clinically defined cognitive disorders.
International studies indicate that the risk of developing dementing diseases among patients with subjective cognitive impairment is significantly higher than the average in the population [6]. Therefore, even isolated complaints that are not confirmed by cognitive tests should not be ignored by the attending physicians. They cannot serve as the basis for any specific clinical diagnosis, but their presence is an indication for active prevention, primarily non-pharmacological (mental and physical activity, optimization of nutrition and lifestyle).
Diagnosis of mild cognitive impairment
As follows from the above criteria (Table 2), the diagnosis of moderate neurocognitive impairment syndrome is based, firstly, on complaints from patients and/or their relatives, and secondly, on objective test results. It should be borne in mind that cognitive complaints are not always straightforward. Typically, patients with the so-called amnestic type of mild neurocognitive impairment syndrome, whose cognitive status is dominated by progressive mnestic disorders, complain of decreased memory or increased forgetfulness. Such patients are more likely to develop Alzheimer's disease in the future. However, according to an analysis of specialized outpatient care for patients with cognitive impairment, the most common cause of mild cognitive impairment syndrome is cerebrovascular pathology. Thus, the experience of the first Russian clinic for memory disorders indicates that discirculatory encephalopathy or the consequences of acute cerebrovascular accidents cause 68% of moderate cognitive impairment [7].
Vascular cognitive impairment in most cases belongs to the so-called subcortical-frontal type. At the same time, memory for current events and life events practically does not suffer, and the cognitive status is dominated by a decrease in concentration of attention and rate of cognitive activity (bradyphrenia), a violation of the frontal control functions (planning and control). A characteristic feature is also the frequent combination of cognitive and emotional-behavioral disorders: depression, apathy or affective lability. It should be emphasized that emotional and behavioral disorders in chronic cerebrovascular insufficiency are organic in nature and are caused by the same brain damage (dysfunction of frontostriatal connections) as cognitive impairment. The comorbidity of vascular depression and vascular cognitive impairment is at least 80% [8–11].
Patients with vascular cognitive disorders rarely complain of forgetfulness, since their memory is relatively intact. The structure of complaints is dominated by so-called subjective neurological symptoms: headache, unsystematic dizziness, noise and heaviness in the head, increased fatigue, sleep disturbances. These symptoms are quite typical for the initial stages of dyscirculatory encephalopathy and in the recent past were considered as an important sign of chronic ischemic brain damage. It is now clear that headache, dizziness and other unpleasant sensations in the head cannot be a direct result of cerebral ischemia. The pathogenesis of subjective neurological symptoms is more complex and is associated primarily with existing cognitive, emotional and motor disorders. Thus, the headache most often has the character of a tension headache, which, as is known, is almost always caused by anxiety and/or depression. Sleep disturbances also have an emotional cause. Increased fatigue can either be a sign of depression (Table 4) or reflect a decrease in mental performance. In the latter case, this complaint is the subjective equivalent of cognitive disorders. Dizziness in chronic cerebrovascular insufficiency is usually non-systemic in nature and is described as a feeling of unsteadiness when walking. Behind this sensation, as a rule, there are real imbalances due to damage to the frontostriatal and frontocerebellar connections.
Subjective neurological symptoms are almost always present in the initial stages of chronic cerebrovascular insufficiency. They cannot be the basis for a diagnosis, but should lead the doctor to suspect chronic cerebrovascular disease. To confirm the diagnosis, careful assessment of cognitive and emotional status using objective techniques is necessary. At the stage of moderate (non-dementia) cognitive impairment, the most sensitive methods should be used, for example, the Montreal Cognitive Function Assessment Scale [12].
Pathogenetic and symptomatic therapy of non-dementia cognitive impairment
To date, a single generally accepted protocol for the management of patients with cognitive impairment that does not reach the severity of dementia has not been fully developed. Many international studies have failed to demonstrate that pharmacotherapy with drugs such as acetylcholinesterase inhibitors, piracetam, and nonsteroidal anti-inflammatory drugs prevents or reduces the risk of dementia [2–4]. At the same time, the same studies demonstrated the ability of some of the above drugs to reduce the severity of symptoms in patients with mild cognitive impairment syndrome.
Empirically, vasotropic and neurometabolic drugs, the dopaminergic and noradrenergic drug piribedil (Pronoran) and NMDA receptor blockers are currently widely used in everyday clinical practice.
The results of a number of large studies and practical experience indicate the clinical effectiveness of the drug piribedil (Pronoran). Pronoran has a complex mechanism of action: it stimulates postsynaptic D2/D3 receptors for dopamine and blocks presynaptic alpha-adrenergic receptors. In this case, blockade of presynaptic adrenergic receptors leads to an increase in cerebral noradrenergic activity. Thus, with the use of this drug, the activity of two cerebral neurotransmitter systems increases: dopaminergic and noradrenergic. Both of these systems are directly involved in cognitive activity. It is believed that dopaminergic stimulation of the prefrontal cortex, indirectly through the mesocortical dopaminergic pathway, plays an important role in attention processes and provides intellectual flexibility, that is, the ability to change the paradigm of behavior. Noradrenergic activation is important for the processes of memorizing and reproducing information, since it provides an optimal level of concentration and motivation for mnestic activity. With age, the synthesis and activity of both dopamine and norepinephrine decrease. Therefore, correction of these neurotransmitter disorders during the use of Pronoran helps to reduce the severity of age-associated impairments in attention and memory. In addition, due to its adrenergic blocking and dopaminergic effects, Pronoran also has a beneficial vasotropic effect, which creates additional benefits in cognitive impairment of vascular etiology [13–16].
In clinical practice, Pronoran is used for the treatment of mild and moderate cognitive impairment, not reaching the severity of dementia, in patients over 50 years of age. The drug can be prescribed both for vascular cognitive impairment and at the initial stages of the neurodegenerative process. A large number of clinical studies have been performed for this indication, including using a double-blind method. So, in France in the 1980s. 14 clinical studies were conducted, which involved more than 7 thousand patients with non-dementia cognitive impairment. It has been shown that Pronoran promotes a significant improvement in memory, concentration and intellectual flexibility, that is, the ability to change the paradigm of behavior depending on external conditions [17, 18]. In 2001, the clinical effectiveness of Pronoran was again demonstrated in the work of D. Nagaradja and S. Jayashree. The authors used Pronoran for mild cognitive impairment syndrome in accordance with modern diagnostic criteria. It was shown that the study drug resulted in a more than twofold increase in the frequency of cognitive improvement on the Mini-Mental State Examination Scale compared to placebo, which was statistically and clinically significant [19].
Currently, Russian specialists also have significant experience in using Pronoran in patients with cognitive impairment that does not reach the severity of dementia. Thus, as part of the PROMETHEUS study, Pronoran was administered to 574 patients from 33 cities in 30 regions of Russia, of which 336 women and 207 men, aged from 60 to 89 years (average age 69.5 ± 5.5 years) with mild or moderate cognitive disorders . Patients were selected for treatment with cognitive complaints who scored 25–27 on the Mini-Mental State Examination or performed the clock-drawing test with errors, but did not meet diagnostic criteria for dementia. During therapy, a statistically significant improvement in cognitive function was recorded, which was noted already in the sixth week of treatment and subsequently increased until the end of the 12-week follow-up. At the same time, one part of the patients received monotherapy with Pronoran, and the other part received Pronoran in combination with vasotropic and/or neurometabolic drugs. There was no significant difference between these groups of patients, that is, the combination of Pronoran with vasotropic and neurometabolic therapy had no advantages over monotherapy with the study drug [20, 21].
As part of the largest Russian non-comparative study, more than 2 thousand patients aged 50 to 94 years (mean age 64.9 ± 8.3 years) with a diagnosis of first or second stage dyscirculatory encephalopathy and with mild or moderate cognitive impairment received Pronoran therapy. violations. All patients took Pronoran for three months. According to the attending physicians, in 2/3 of cases there was a significant or moderate improvement in cognitive and other neurological functions [22].
According to some data, the magnitude of the therapeutic effect of dopamine and noradrenergic therapy in relation to non-dementia cognitive disorders may be greater than that of other vasotropic and neurometabolic drugs actively used in clinical practice. In the FUETE study, 189 patients were observed, including 139 women and 57 men, aged from 42 to 82 years (mean age 63.6 ± 8.5 years) with cognitive disorders not reaching the severity of dementia, against the background of arterial hypertension and cerebral atherosclerosis . Patients were treated with various drugs, and representatives of the therapeutic groups did not differ in age, level of education and clinical features of the underlying disease. During the therapy, regression of both subjective and objective cognitive disorders was observed in all compared therapeutic groups. At the same time, the severity of subjective improvement and objective dynamics of cognitive tests during the use of Pronoran after two months of therapy were significantly greater compared to vasotropic and neurometabolic therapy (Fig. 1) [23].
Regression of cognitive disorders, according to special tests, is the main criterion for the effectiveness of the therapy. However, as noted above, many patients with moderate cognitive impairment, primarily of a vascular nature, also complain of headache, unsystematic dizziness, noise, heaviness or other unpleasant sensations in the head, increased fatigue and sleep disturbances. These complaints are of the same nature and are associated with both cognitive failure and changes in the emotional status of patients at the initial stage of chronic cerebrovascular insufficiency. They significantly reduce the quality of life of patients and are often the main reason for visiting a neurologist. Therefore, the dynamics of subjective neurological symptoms in patients with the syndrome of mild neurocognitive impairment of vascular etiology during therapy is extremely important for assessing the significance of the clinical effect and the degree of influence of therapy on the daily life of patients. Regression of subjective neurological symptoms most contributes to adherence to therapy.
In the study by N.N. Yakhno et al. (2006) 29 patients diagnosed with “moderate cognitive impairment” against the background of discirculatory encephalopathy of the first and second stages received Pronoran for three months [24]. No other vasotropic or neurometabolic drugs were used. During treatment with Pronoran, the frequency and severity of headaches, dizziness, fatigue and the subjective feeling of forgetfulness significantly decreased (Fig. 2). Other authors have also reported a weakening of subjective neurological symptoms with the use of Pronoran [17, 18]. Thus, dopamine and noradrenergic therapy contributes to a significant improvement in the well-being of patients, and consequently increases the quality of life and adherence to ongoing treatment measures.
It can be summarized that to date, Pronoran has established itself as an effective drug that improves cognitive abilities and well-being in patients with the initial stages of organic cerebral diseases without dementia. Unlike Parkinson's disease, for which significantly larger doses are used, for non-dementia cognitive impairment Pronoran is prescribed at a dose of 50 mg/day once a day. The recommended duration of therapy is at least three months.
Correction
It is impossible to completely cure mental retardation, even in a mild form, since organic brain damage is irreversible. But it can easily be corrected by child psychiatrists and teachers at specialized schools. Special programs have been developed, based on concrete and visual methods, to help children acquire simple skills and the ability to demonstrate compensatory capabilities.
Training takes place at a slow pace, familiar to the patient. As a result, the patient can freely adapt to the surrounding space and respond appropriately to its changes.
The neurocorrectional assistance program takes into account the child’s neuropsychological characteristics and strengths. It allows you to develop:
- fine motor skills, coordination and motor skills;
- visual-motor coordination - strengthen the muscles of the eyes and the tracking movements of the latter, which is necessary for reading and writing, establish communication between the eye and hand;
- stable connections between the hemispheres of the brain to increase the speed of processing sensory information;
- attention, self-control;
- functions of thinking, spatial perception, ability to construct coherent speech and logical-grammatical construction;
- concept of wrong behavior;
- auditory perception of speech and non-speech sounds, the ability to differentiate tempo-rhythmic patterns.
In some cases, to achieve your goals, there may be a need for a speech therapist, speech pathologist, or neurologist.
From cognitive impairment to dementia
Recently, the problem of pre-dementia mild and moderate cognitive impairment has received increasing attention from doctors and researchers. Although mild and moderate cognitive impairment is not as severe a socioeconomic burden as dementia, the presence of even mild cognitive impairment significantly reduces the patient’s quality of life, and the risk of developing dementia among patients with moderate cognitive impairment is very high and amounts to up to 10-10% 15% per year. Therefore, an extremely important aspect for a neurologist is the diagnosis of cognitive impairment at pre-dementia stages with the goal of prescribing therapy as early as possible to prevent or delay the onset of dementia.
A brief excursion into the history of the Kyrgyz Republic
The criteria for vascular dementia were developed in the late 60s of the twentieth century, so in the pathogenesis of vascular CR, the leading role was given to multi-infarction brain damage, which distinguished neurodegenerative AD from vascular dementia. Subsequently, the presence of multiple large and small (lacunar) infarctions was identified as the cause of vascular dementia. Later, in addition to heart attacks, infarction in areas of the brain strategic for cognitive functions, non-stroke lesions of the white matter of the brain, cerebral hemorrhages, and states of cerebral hypoperfusion began to be identified as the cause of vascular dementia. In 1993, Hachinski et al. proposed the term “vascular cognitive impairment” - vascular cognitive disorders, to designate cognitive disorders that develop as part of cerebrovascular diseases.
The above criteria once again show how difficult it is to diagnose mild cognitive impairment, while MCI manifests itself and is diagnosed more clearly.
Diagnostic criteria for mild and moderate cognitive impairment
| Diagnostic criteria for mild cognitive impairment. Yakhno N.N., Zakharov V.V., Lokshina A.B., 2005. | Modified diagnostic criteria for MCI syndrome (MCl-Revised), J. Touchon, R. Petersen, 2004. |
| 1. Complaints about decreased memory or mental performance, expressed independently or with active questioning of a doctor. 2. Mild cognitive impairment, predominantly of a neurodynamic nature, identified during a neuropsychological study. 3. The absence of cognitive impairment according to the results of dementia screening scales is the result of a brief mental status scale of at least 28 points. 4. Stage 2 on the global deterioration rating (GDS). 5. Absence of disturbances in daily activity, including its most complex forms. | 1. Cognitive impairment, according to the patient and/or his immediate environment (the latter is preferable) 2. Signs of recent decline in cognitive abilities compared to the individual norm. 3. Objective evidence of cognitive impairment obtained using neuropsychological tests (a decrease in the results of neuropsychological tests by at least 1.5 standard deviations from the average age norm). 4. There are no disturbances in the patient’s usual forms of daily activity. However, there may be difficulties in complex activities. 5. There is no dementia - the result of the brief mental status assessment scale is at least 24 points. |
It should be noted that CR of varying severity are observed in the vast majority of patients (87%) who have suffered a stroke. Thus, a decrease in visual memory and attention predominates in patients with deep lesions in the right hemisphere of the brain, and a decrease in auditory-verbal memory predominates in patients with lesions in the left hemisphere
Today, due to various circumstances, mostly mild cognitive impairment and dementia are diagnosed in clinical practice. The syndrome of mild cognitive impairment (synonym: “mild cognitive decline syndrome”) requires special consideration.
MCI syndrome refers to impairments of memory and other higher functions in older people that go beyond the age norm (natural aging), but do not cause social maladaptation; at this stage of development it is difficult to attribute them to any nosological form.
Patients with MCI may experience:
- moderate decrease in the ability to concentrate;
- difficulties in simultaneous perception of several stimuli;
- memory impairment for current events, names of new acquaintances, geographical names;
- absent-mindedness, frequent searches for forgotten things.
Along with impaired memory and attention, at the pre-dementia stage there may be mild speech impairments, expressed in forgetting the names and surnames of loved ones, difficulties in choosing the right word, vocabulary depletion, and mild visual-spatial impairments (difficulty orienting in unfamiliar places). At the same time, patients remain completely critical of their condition; sometimes they even tend to exaggerate the cognitive impairments they have, which leads to severe anxiety and depression. MCI is often accompanied by fatigue, decreased mood and anxiety due to the awareness of one’s own inferiority.
ICD-10 offers the following criteria for diagnosing MCI:
- presence of decreased memory, attention and/or learning ability;
- subjective complaints of increased fatigue during mental work;
- lack of connection between cognitive impairment and confusion;
- absence of dementia;
- organic nature of cognitive disorders.
MCI syndrome occupies an intermediate position between changes in cognitive functions caused by aging and dementia, and can be classified as a pre-dementia stage.
From MCI to dementia
In the vast majority of cases, cognitive changes in MCI syndrome are progressive. The outcome of progression of MCI is dementia. According to the DSM-111-R manual (1987), dementia is defined as impairment of short-term and long-term memory, combined with disorders of abstract thinking, judgment and other higher functions of the body, as well as personality changes . All this quite seriously interferes with the patient’s professional activities, complicates normal social activity and contact with other people. Dementia is diagnosed only when intellectual-mnestic impairments are combined with a decrease or decay in the ability to perform professional and social activities.
Comparative characteristics of MCI and dementia:
| UKR | Dementia |
| Daily activities are not impaired (only the most complex activities are limited) | Patients “cannot cope with life” due to an intellectual defect and require outside help |
| Mini-Mental State Examination score usually below 24 | Mini-Mental State Examination score is often (but not always) below 24 |
| The course is variable: along with progression, long-term stabilization and spontaneous regression of the defect are possible | The cognitive defect is in most cases progressive, but sometimes has a stationary or reversible nature |
| Criticism is intact, violations are more disturbing to the patient himself | Criticism is reduced, violations worry the patient’s relatives more |