Introduction
The onset of pregnancy in a woman with epilepsy is not only a desirable, but also a very important stage of life.
Therefore, it is necessary for a patient of fertile age to be immediately explained upon her first visit to an epileptologist that this event, like any good impromptu event, must be planned. The ability to have children with epilepsy in women is reduced on average by 2 times compared to the general population. This is due to both social and organic reasons. Antiepileptic drugs (AEDs) can disrupt the functions of the endocrine system and provoke the development of sexual disorders (hypo- or hypersexuality), obesity, hypothyroidism, polycystic ovary syndrome, delayed sexual development, menstrual dysfunction and ovulation disorders.
Pregnancy is contraindicated only in women with severe epilepsy, when taking AEDs does not help to avoid frequent generalized seizures, in addition, the woman has severe mental disorders.
Epilepsy is not a contraindication to IVF, although we should not forget that to stimulate the production of eggs, women candidates for IVF undergo massive administration of hormonal drugs. This can sometimes trigger seizures.
Read also
Causes of epilepsy
“Where did my seizures come from?
There are no epileptics in our family!” - the most common phrase at the reception, we will tell you about the causes of epilepsy. Indeed, up to 70% of all epilepsies are genetically predetermined... Read more
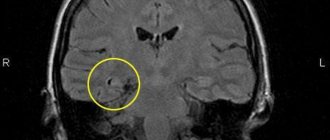
Temporal lobe epilepsy
Temporal lobe epilepsy is a special form of epilepsy, which is characterized by the localization of the epileptic focus in the temporal region of the brain. This type of pathological process is one of the most…
More details
Treatment of epilepsy in Samara
Epilepsy therapy is a long process and requires interaction between the epileptologist and the patient. Currently, it is possible to stop attacks and achieve remission in 60%! How to do it? Basic…
More details
Symptoms of epilepsy
How does epilepsy manifest? The most “famous” epileptic attack is a convulsive one, as the most “bright” one, this attack includes general tonic-clonic seizures, blueness of the face, salivation, ...
More details
Epilepsy
These are epileptic seizures that occur repeatedly, regardless of any cause, and are associated with chronic illness of the cerebral cortex. Epilepsy is a very common disease. Approximately…
More details
Preconception preparation for women with epilepsy
Pregravid (from Latin gravida
- pregnant) preparation - a set of preventive, diagnostic and therapeutic measures, the result of which is the readiness of future parents to fully conceive, bear and give birth to a healthy child. Planning a pregnancy is not just about taking vitamins, quitting drinking and smoking 1-2 months in advance. before conception. Preconception preparation begins 6–10 months in advance. before the desired pregnancy and includes a specific list of procedures.
Pregravid preparation takes place in several stages:
Medical examination of spouses.
Preparing a couple for conception, a woman for bearing a child.
Determining favorable days for conception.
The number and scope of studies before a planned pregnancy are determined for each patient individually by a therapist, gynecologist, or geneticist. From the point of view of an epileptologist, it is necessary to determine the concentrations of AEDs in the blood plasma; perform a general blood test to determine platelet levels; biochemical blood test to determine the level of ALT, AST, bilirubin, alkaline phosphatase; take an electroencephalogram (EEG) or conduct video-EEG monitoring. In some cases, when planning pregnancy, it is advisable to conduct an ultrasound examination of the uterus and its appendages, as well as a number of hormonal studies that reflect the function of the woman’s reproductive system. To select the dose of AED, regular testing of the concentration of the drug in the blood is indicated, and to maintain a constant concentration, it is advisable to use dosage forms with a slow release (durant forms).
An indication for an unscheduled determination of the concentration of AEDs in the blood before pregnancy is an increase in frequency/severity of attacks or the appearance of symptoms of intoxication.
During the preconception period, it is recommended to consult a geneticist to determine the risk of epilepsy in the unborn child. Epilepsy is not a hereditary disease, but in some cases it can be inherited. The risk of transmitting epilepsy to a child from mother with genetic epilepsies is on average 10%, with unknown etiology and structural epilepsy - 3%. The risk of paternal transmission of epilepsy is on average 2.5%. If both parents suffer from epilepsy, the risk of a child inheriting epilepsy increases to 10–12%. If a woman suffers from structural or unknown etiology epilepsy, the risk for the unborn child increases threefold compared to the general population, but in the case of genetic generalized or focal epilepsy - 10 times.
You need to undergo genetic testing if:
both partners in a couple have epilepsy;
the couple already has a child with epilepsy;
in the family, one or both parents had cases of epilepsy, developmental defects (congenital cleft palate or cleft lip, finger deformities, etc.) and hereditary diseases;
the patient had 2 or more spontaneous miscarriages, cases of fetal or newborn death.
The main goal of the doctor is to achieve complete control of the attacks before the desired pregnancy occurs. An important indicator is the duration of the absence of attacks in the patient before pregnancy: if for 9 months. If there are no seizures, then there is a very high probability that there will be no seizures during pregnancy. However, it is difficult to predict the course of each specific pregnancy.
It is not advisable to stop taking AEDs during the period of conception. A woman should be warned that the risk of developing congenital anomalies of the fetus while taking AEDs increases threefold, but that refusal to take the drug is fraught with even more serious consequences - injury or death of the fetus in the event of an epileptic seizure. It is necessary to explain to the patient that sudden cessation of taking AEDs sharply increases the risk of attacks, can lead to failure of remission, and increase the frequency of existing attacks.
The administration of folic acid is indicated to prevent pathological effects on the fetus and reduce the risk of miscarriage (spontaneous miscarriages). Folic acid supplements must be prescribed before the patient becomes pregnant, since for most women pregnancy itself is a surprise. It is recommended to start taking folic acid supplements 3 months in advance. before the expected pregnancy at a dosage of 3–5 mg/day and continue taking until 14 weeks. pregnancy. In addition to folic acid, the use of complex vitamin preparations recommended for pregnant women is also indicated. Anemia treatment is carried out before pregnancy with the use of drugs containing iron and folic acid.
Since sodium valproate is more likely than carbamazepine to have a teratogenic effect, and the combination of valproate and lamotrigine is especially dangerous, carbamazepine is the drug of choice, but only if there are no contraindications to its use (most forms of genetic generalized epilepsy, secondary bilateral synchronization on the EEG in patients with focal epilepsy). Information about the effect of “new” AEDs on the intrauterine development of the fetus is still insufficient, therefore, unless there is an urgent need, it is better to refrain from introducing them into therapy during the period of preparation for pregnancy.
The doctor is at a great disadvantage. By allowing a woman to become pregnant and give birth to a child, he takes on additional responsibility and new risks. If teratogenic consequences occur, the patient and her relatives will attribute this to the AEDs prescribed by the doctor; in case of exacerbation of the disease, the cause of suffering will be considered to be incorrectly selected therapy, and not the long-awaited pregnancy. In addition, the question of having a child in patients with epilepsy, for various reasons, does not arise at a very young age.
Features of management of pregnant women with epilepsy
At this period of life, the leading doctor is an obstetrician-gynecologist, with whom the patient should be regularly monitored. Until the 28th week. examinations are carried out once a month, from the 28th to the 36th week - once every 2 weeks, and after the 36th week. - every week. Throughout pregnancy, a woman should be observed by an epileptologist: with complete control of seizures - once every 2 months, with repeated partial seizures - once a month. The patient should be warned about the need to consult a doctor if attacks become more frequent. If there is any concomitant pathology: diabetes mellitus, anemia, arterial hypertension, kidney disease, etc., supervision of related specialists is required. Most gynecologists, neonatologists and pediatricians are very afraid of the negative effects of AEDs on the body of the mother and fetus, while at the same time they do not attach such importance to the drugs they prescribe. However, the prescription of AEDs is the competence of an epileptologist; changing the treatment regimen is possible only in agreement with him. If other specialists make adjustments to therapy or insist on discontinuing AEDs, then you need to inform your epileptologist about this.
Currently, there is no reliable data on the increased incidence of pregnancy complications (preeclampsia, arterial hypertension, spontaneous abortions, changes in the frequency of seizures, status epilepticus) in women with epilepsy taking AEDs compared to the general population.
During pregnancy, the minimum effective doses of AEDs should be used, preferably in monotherapy [1]. Taking one drug reduces the risk of possible fetal development defects. The dose of AEDs should be as low as possible, but one that does not cause generalized seizures. Changing the drug to an analogue may lead to an increase in attacks. It is recommended to continue taking the same drug from the same manufacturer.
An important safety factor is the use of drugs with controlled release of the active substance, which can be used 2 times a day. This eliminates concentration peaks that have a particularly adverse effect on the fetus.
Nausea and vomiting due to toxicosis can significantly complicate the use of AEDs. To avoid a decrease in the concentration of drugs in the blood, you can use intravenous or rectal forms. With frequent vomiting (up to 20 or more times a day), hospitalization is indicated.
Unfortunately, none of the “first aid drugs for seizures” are registered in Russia. The only available way to prevent an attack in Russian conditions is the use of diazepam tablets under the tongue when an attack is anticipated. Taking additional doses of AEDs, as a rule, does not make sense, since their absorption period is quite long.
Pregnant women are contraindicated in taking psychotropic drugs and strong sleeping pills. Sleep disorders should be treated with non-drug methods: herbal medicine (decoction of calamus, fireweed, oregano, chamomile, mint, linden, peony, etc.); psychotherapy (listening to quiet relaxing music before bed); aromatherapy; compliance with sleep hygiene, as well as work and rest regimes.
Fluoroquinolones are contraindicated in epilepsy. The use of some other groups of antibiotics and antimicrobials: macrolides, high doses of penicillins should also be avoided if possible. However, if inflammation is present, the benefit of antibiotic therapy may outweigh the risk.
Pregnant women with epilepsy are contraindicated for physiotherapy in the head and neck area.
Valproate intake is associated with weight gain. However, weight gain also occurs during pregnancy. In most cases it is impossible to say unequivocally what explains weight gain - taking valproate or an abnormal course of pregnancy. To correct body weight, observation by a gynecologist-endocrinologist and diet are indicated. Replacing valproate with another AED during pregnancy is not justified; it can lead to the occurrence/increase of attacks and is only permissible if absolutely necessary.
In 15–20% of women, the number of attacks may increase, more often in the first or third trimester of pregnancy. Increased seizure frequency cannot be predicted based on seizure type, duration of epilepsy, or increased frequency of seizures during a previous pregnancy. Even the presence of hormonal-dependent epilepsy is not a prognostic factor for increased frequency of epileptic seizures during pregnancy. The resumption of attacks may be due to the pharmacokinetics of AEDs during pregnancy.
The most common triggers for seizures during pregnancy are emotional stress and sleep deprivation. An increase in body temperature can provoke attacks and accelerate the elimination of AEDs. Hypoglycemia (low blood glucose levels) and alcohol consumption can also lead to the occurrence/increasing frequency of attacks. Seizures may become more frequent after a traumatic brain injury. Therefore, you need to lead a correct lifestyle, carefully monitor your health, and observe a work and rest schedule. However, quite often attacks occur completely unpredictably, and a “healthy lifestyle” does not prevent them. Therefore, it is necessary to take a sufficient dose of AEDs, and not just eliminate provoking factors.
Severe and moderate forms of ARVI or influenza aggravate the course of epilepsy and can provoke the appearance/increase in seizures. Despite this, specific prophylaxis (vaccination) is not recommended, because, firstly, the effect of a number of vaccines on the fetus has not been adequately studied, which means they are potentially dangerous for the fetus, and secondly, an adverse reaction to their introduction is an increase in temperature. To prevent influenza in pregnant women, natural immunomodulators (“folk remedies”) are used, as well as hygiene measures (avoid crowded places, wash your hands and face, wash your nose and eyes after returning from the street).
Generalized seizures are considered the most dangerous for both mother and child. During their development, many factors have a negative impact on the body of the mother and child. Focal seizures can generally be considered to have no impact, but it is important to remember that they can take a generalized form.
The study of the concentration of AEDs in the blood during pregnancy should be carried out repeatedly, at least once every 2 months, and in the case of recurring attacks - monthly. This must be done not only because during pregnancy the metabolism of AEDs or drug concentrations may change due to weight gain, but also to monitor compliance.
Plasma concentrations of lamotrigine may decrease significantly during pregnancy. Also, at the end of the first trimester, due to increased clearance, it may be necessary to increase the daily dosage of levetiracetam.
To assess the full functioning of the placenta and early diagnosis of fetoplacental insufficiency, it is advisable to study the hormones of the fetoplacental complex (placental lactogen, progesterone, estriol, cortisol) monthly from the end of the first trimester of pregnancy.
Particular attention is paid to the study of alpha-fetoprotein. At the end of the last century, it was found that in cases of neural tube defects in the fetus (anencephaly and spina bifida), the content of alpha-fetoprotein, a protein synthesized in the fetal liver, increases in the mother’s blood serum. With neural tube defects, alpha-fetoprotein penetrates through the capillary wall in the area of the defect into the amniotic fluid, and from there into the mother's bloodstream. With the introduction into clinical practice of a method for determining the level of alpha-fetoprotein in maternal blood serum, it was possible to increase the accuracy of diagnosing neural tube defects of the fetus. Thus, using this method, up to 97–98% of cases of anencephaly are detected. Determination of serum alpha-fetoprotein levels is also used to diagnose multiple pregnancies, anterior abdominal wall defects and other fetal malformations. It has been established that with Down syndrome in the fetus, the content of alpha-fetoprotein in the mother's blood serum decreases. Determination of alpha-fetoprotein levels is carried out at 15–20 weeks. pregnancy, the most informative study is at 16–18 weeks; it is repeated if changes are detected during ultrasound.
Fetal ultrasound is performed at 19–21 weeks. pregnancy to exclude developmental anomalies. A high level of alpha fetoprotein in the maternal serum is an absolute indication for fetal ultrasound.
An important diagnostic method is cardiotocography. This method allows you to obtain more objective information about the state of the fetal cardiovascular system compared to auscultation of heartbeats. Cardiotocography evaluates the fetal heart rate, its variability, the presence of accelerations (increased heart rate by 15–25 beats per minute during fetal movements) and decelerations (decrease in heart rate by no more than 30 seconds during contractions). The normal state of the fetus corresponds to a heart rate of 120–160 per minute, good heart rate variability (mainly due to accelerations) and the absence of high-amplitude decelerations. The value of this research method lies in the simultaneous determination of fetal heartbeats and uterine motility. The method allows you to diagnose intrauterine fetal hypoxia due to fetoplacental insufficiency.
The patient should warn the obstetrician that a number of medications are contraindicated for her: nootropics, analeptics, psychotropic drugs (with the exception of fractional administration of small doses of benzodiazepines in order to potentiate pain relief during childbirth).
Due to the potential for vitamin K deficiency when taking enzyme-inducing AEDs (carbamazepine) in the last weeks of pregnancy, it is advisable to prescribe vitamin K to a woman using these AEDs at a dose of 10–15 mg/day.
Epilepsy and pregnancy
Until recently, pregnancy was contraindicated for a number of diseases - due to unpredictable complications of the disease during pregnancy and the lack of safe treatment that does not have a harmful effect on the fetus. Epilepsy was just one of this series. Most often, women with this disease were not recommended to become pregnant.
Features of the functioning of the body of a pregnant woman against the background of epilepsy
During pregnancy, changes are observed both in the functioning of many organs and at the biochemical level, which affects the course of epilepsy in the mother. In some cases, the number of seizures becomes more frequent, while in others, on the contrary, it decreases. Research data shows that the frequency of seizures increases in 17–33% of pregnant women. Typically, such changes are associated with the fact that women change anticonvulsants, reduce the dose and regimen of medications, fearing their harmful effects on the fetus, so patients suffering from epilepsy should prepare for pregnancy in advance.
Often, taking several drugs (polytherapy) needs to be replaced by taking one drug (monotherapy), which cannot always be done during pregnancy - relapses of seizures are likely.
Antiepileptic drugs significantly reduce folic acid levels in the mother, which increases the risk of neural tube defects in the fetus. Therefore, patients with diagnosed epilepsy should take increased doses of folic acid - from 0.8 to 4 mg per day.
Controlling epileptic seizures is important not only for the woman, but also for the health of the fetus, but the degree of possible harm depends on the type of epilepsy. Studies have shown that generalized seizures can cause fetal hypoxia, which can damage the brain and central nervous system, sometimes leading to fetal death. The effect of localization-related seizures on the fetus has not been studied. Fortunately, epilepsy does not increase the rate of stillbirths, abnormal fetal growth, or other pregnancy complications.
The main problem with epilepsy in pregnant women is taking antiepileptic drugs, most of which are teratogens, that is, drugs that can cause malformations in the fetus.
Epilepsy in itself does not increase the level of fetal malformations in a woman. Clinical studies have shown that pregnancy outcomes and complication rates are similar between untreated and untreated women with epilepsy and those without epilepsy. But since epilepsy is dangerous to a woman’s health, regardless of her condition (not pregnant, pregnant, breastfeeding), treatment is still necessary during pregnancy.
Which anticonvulsant drug is best for a pregnant woman to take?
There is no definite answer to this question, because the selection of medication, dose and regimen is always individual. This means that the same drug will not always be effective when prescribed to different women. But before prescribing any drug, it is important to know how much a woman needs treatment. If no seizures have been observed within two years before pregnancy, then a woman can carry a child without treatment, but it is best to discontinue medications before conception.
During pregnancy, the volume of blood plasma increases significantly, so the concentration of many substances in the blood, including antiepileptic drugs, decreases. Blood filtration by the kidneys also increases, although the amount of urine they excrete remains virtually unchanged. But accelerated metabolism leads to the fact that the drug is eliminated from the body faster. During pregnancy, the blood level of proteins (albumin) involved in the absorption of antiepileptic drugs also decreases. Because of this, the initial dose of the drug may not be effective in stopping seizures.
Let us repeat: if we talk about the effectiveness of drugs, the choice primarily depends on the type of epilepsy. Sodium valproate and lamotrigine are usually prescribed for the treatment of primary generalized epilepsy. In cases of partial epilepsy, the choice of drugs is greater.
No less important is the aspect of the effect of medications on the fetus. The incidence of various abnormalities in fetal development is higher in cases where a woman takes several antiepileptic drugs rather than just one.
Most often, while taking antiepileptic drugs, the following developmental deviations are recorded: cardiovascular anomalies, defects of the genitourinary system, neural tube and craniofacial, in particular cleft palate (cleft palate). Taking medications in the first trimester of pregnancy is especially dangerous for the development of the fetus. However, studies show that the incidence of malformations increases with sodium valproate or a combination of several drugs, while the incidence of carbamazepine, oxarbazepine and phenytoin (as monotherapy) does not increase the incidence.
So, the drugs that it is advisable to avoid during pregnancy are valproate, phenobarbital and phenotoin.
During pregnancy, the following actions are recommended for women with epilepsy:
- Pregnant women taking antiepileptic drugs should be under the supervision of an experienced obstetrician-gynecologist with experience in caring for such patients. A woman diagnosed with epilepsy is at risk for pregnancy complications, so it is advisable that she also be monitored by a specialist in maternal-fetal diseases.
- If necessary, a consultation with a neurologist or psychiatrist is carried out. It is advisable that this doctor also have experience in managing pregnant women with epilepsy.
- If a woman is taking several medications, she should try to choose one drug—switch from polytherapy to monotherapy. However, this transition must be gradual. For example, if a woman is taking 3 medications, she should first try to switch to 2 medications, and then to one.
- A pregnant woman with epilepsy should take at least 4 mg of folic acid per day in the first trimester.
- The examination of such a pregnant woman should include a general blood test, determination of the level of salts (electrolytes) in the blood, a neurological examination, and, if necessary, magnetic resonance imaging, computed tomography, and encephalography.
- A woman is recommended to undergo prenatal genetic screening, which should include determination of the content of a number of substances in the blood and an ultrasound scan at 11–13 weeks.
- It is advisable to determine the level of serum alpha-fetoprotein in the blood serum before 20 weeks, but this procedure is not necessary.
- A thorough anatomical ultrasound to identify possible fetal defects should be performed at 16–20 weeks.
- Invasive testing methods (amniocentesis) to determine the level of alpha protein and acetylcholinesterase in amniotic fluid are not recommended unless specifically indicated.
- It is not necessary to determine the level of anticonvulsants (free and bound) in the blood plasma, but for some of them (lamotrigine, levetiracetam, oxcarbazepine) it is still advisable to do this monthly.
- From 36 weeks of pregnancy, prophylaxis with vitamin K is recommended to prevent hemorrhagic disease in the newborn, although such prophylaxis is often given only to newborns after birth.
Trial of childbirth
Childbirth is a very serious burden on the female body. They may be accompanied by excessive fatigue, which in turn can lead to cramps (1-2% of cases). Women suffering from epilepsy, regardless of whether they take medication or not, should be under constant close supervision during childbirth by a whole team of specialists - an obstetrician-gynecologist, a neurologist, an anesthesiologist, a pediatrician who are aware of the disease of the mother in labor and have experience in managing childbirth in such patients. .
The optimal type of pain relief for a woman suffering from epilepsy is epidural anesthesia. Pain medications (such as pethidine) may trigger seizures.
The presence of epilepsy is not an indication for cesarean section, so most patients with this diagnosis can give birth naturally. The choice of delivery method will depend on the general condition of the mother and fetus, as well as the presence of other indications or contraindications from both. Caesarean section is performed in women who have had frequent seizures during the last weeks of pregnancy.
With the onset of labor, it is necessary to determine the level of anticonvulsant medication in the blood serum. If levels are low, the woman may be offered an additional dose of the drug or intravenous benzodiazepines or phenytoin. Benzodiazepines can cause respiratory dysfunction in the mother and newborn, so constant monitoring of both is necessary.
Status epilepticus is an extremely rare condition during childbirth. If other possible causes of seizures have been excluded, treatment is carried out according to the protocol, regardless of pregnancy, although the condition of the fetus is constantly monitored. In some cases, an emergency caesarean section is indicated.
In general, the modern state of medicine allows a woman suffering from epilepsy to safely bear and give birth to a healthy child.
Share link:
- Click to share on WhatsApp (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Skype (Opens in new window)
- Send this to a friend (Opens in new window)
- Click to print (Opens in new window)
By
Features of the labor period in women with epilepsy
Women with epilepsy have a higher risk of bleeding, weak labor and preeclampsia (the risk of the latter is 2 times higher than in the population), placental abruption, premature birth; obstetrics are 2 times more likely to be carried out by vacuum extraction of the fetus or cesarean section. To reduce the risk of complications, it is necessary to establish complete control over attacks.
The likelihood of an epileptic seizure during labor and within 24 hours after birth is higher than the likelihood of an epileptic seizure during other periods of pregnancy. First of all, this is due to skipping an AED dose.
Epilepsy is not a contraindication for natural delivery, and drug management of labor and pain management do not differ from generally accepted standards. In most cases, long-term epidural analgesia can be used.
Indications for cesarean section are increased frequency of epileptic seizures, convulsive seizures more often than once a week. in the last trimester of pregnancy, serial or status epilepsy in the prenatal period, fetal hypoxia, weakness of labor, convulsive attack during childbirth.
Epilepsy in pregnant women
Conservative therapy
When developing medical tactics, the risk of worsening epileptic disease in the current gestation, the mutagenic and teratogenic potential of the prescribed anticonvulsants, and the patient’s age are taken into account.
Indications for medical abortion are a pharmacoresistant form of the disease with frequent paroxysms, a status type of epilepsy, pronounced characterological changes or psychotic disorders that pose a threat to the woman and the fetus. The issue of termination of pregnancy is decided by a committee of an obstetrician-gynecologist and a neurologist-epileptologist, taking into account the opinion of the patient. When deciding to continue gestation, women with compensated epilepsy in remission are recommended to be examined by an epileptologist every 2 months; in the presence of partial seizures, consultation is carried out at least 1-2 times a month. At the 19-20th week, a pregnant woman is usually hospitalized in a hospital for a comprehensive examination and preventive therapy. A standard treatment regimen for active epilepsy usually includes:
- Anticonvulsants
. Basic monotherapy is carried out with retardated antiepileptic drugs in the minimum effective dosage using therapeutic drug monitoring. Carboxamide and valproic acid derivatives are recommended. If attacks become more frequent, tranquilizers may be prescribed. - Folic acid preparations
. To reduce the risk of teratogenesis and spontaneous miscarriage, provoked by disturbances of the folate cycle under the influence of anticonvulsants, folic acid is prescribed to pregnant women before the 13th week of gestation. Even more effective is the use of combination drugs, which also include iron and cyanocobalamin. - Vitamin K1
. Products containing phylloquinone are used from the 36th week to prevent erythroblastosis of newborns. Due to its influence on the synthesis of prothrombin, factors VII, IX, X, proteins C, S, Z, vitamin K increases blood clotting. Phylloquinone also improves the interaction between vitamin D and calcium, which helps strengthen bones and prevent osteoporosis.
Therapy is supplemented with phytosedatives, vitamin-mineral complexes containing B vitamins, zinc, selenium, magnesium, omega-3 acids. Surgical methods for treating the disease during pregnancy are not used.
Childbirth with epilepsy
Patients suffering from epilepsy are recommended to be hospitalized in a specialized obstetric hospital at 38-39 weeks of gestation. With complete clinical-electroencephalographic remission, the preferred method of delivery is natural birth with epidural anesthesia and monitoring the concentration of antiepileptic drugs in the blood. Indications for a cesarean section, in addition to obstetric complications, are an increase in seizures at the end of pregnancy and the occurrence of status epilepticus.
Due to changes in metabolism and a woman's weight loss in the early postpartum period and during the first 3 months after birth, antiparoxysmal therapy must be adjusted. If the baby does not have skin rashes, severe sedation, irritability, or other complications, breastfeeding is allowed against the background of antiepileptic treatment.
Management of the postpartum period in women with epilepsy
The patient should be warned about the need to carefully follow the AED regimen during this period, since there is a risk of decompensation of epilepsy in the postpartum period due to physical overexertion, stress, increased drug load, and increased estrogen activity.
Also, after delivery, symptoms of an AED overdose may appear due to a decrease in the mother’s body weight, blood loss during childbirth, and metabolic changes. If symptoms of neurotoxicity appear - drowsiness, diplopia, nystagmus, ataxia, an urgent study of the concentration of AEDs in the blood is necessary. If the dosage of the drug was increased during pregnancy, it is advisable to return to the daily dose used before pregnancy. If the mother has no seizures and the child has no side effects from AEDs, changing the dose is not advisable. Another danger lies in the increased frequency of attacks due to child care and night awakenings.
Breastfeeding a newborn is quite possible, since the dose of AEDs that enter the child’s body with milk is not comparable to the amount of the drug entering the fetus’s body through the placenta. An exception should be made for phenobarbital and lamotrigine. The mechanisms for their elimination from the body of a newborn are unformed, which can lead to the accumulation of the drug [1].
AEDs acted on the fetus throughout pregnancy, and their content in breast milk was significantly lower than in the blood of a pregnant woman. In addition, you can reduce the amount of the drug in milk by taking AEDs after feeding.
The most common complication in newborns is skin manifestations in the form of allergic reactions. Cases of hemorrhagic complications (increased bleeding) have been described. The use of phenobarbital during pregnancy can lead to both sedative symptoms (drowsiness, weak sucking, muscle weakness, lethargy, lethargy) and withdrawal syndrome (motor agitation, restless sleep, frequent causeless crying), if for some reason breastfeeding milk stops.
If a newborn exhibits low activity, lethargy during feeding, gastrointestinal disorders and other symptoms suspicious of intoxication, then it is better to switch to artificial feeding.
Determining the concentration of the drug in breast milk has no practical meaning. It is much more important that the child has clinical manifestations of the effects of AEDs. The dose of the drug that reaches the baby through breast milk depends on the amount of milk sucked. In children over 6 months of age who have already been introduced to complementary foods, the dose of the drug received decreases as the child grows.
For children at high risk of seizures, an exemption from preventive vaccinations is provided. Vaccination is undesirable in the acute phase of infectious diseases accompanied by an increase in body temperature. Routine vaccination is postponed until the end of acute manifestations of the disease. It is possible to deviate from DTP vaccination or replace it with ADSM.
Women with epilepsy should breastfeed while lying on the bed or sitting on the floor, preferably in the presence of relatives. This will minimize the risk of injury to the mother and/or baby during an attack.
Preeclampsia and eclampsia in patients with epilepsy
Eclampsia is considered a condition characterized by the development of one or more generalized seizures in a woman with preeclampsia. In half of the cases, eclampsia develops before childbirth; the frequency of its occurrence during childbirth and in the postpartum period is approximately the same.
Preeclampsia is characterized by arterial hypertension with proteinuria and edema in the second half of pregnancy. The diagnosis of severe preeclampsia is made when one of the following criteria is present:
increase in systolic blood pressure more than 160 mm Hg. Art. or diastolic blood pressure more than 110 mm Hg. Art., registered twice with an interval of more than 6 hours;
loss of protein in urine more than 5 g/day or a sharply positive result of a rapid urine test for protein;
oliguria (urine amount below 400 ml/day);
severe headache (due to cerebral edema) or blurred vision (due to retinal edema or spasm of the retinal arteries);
signs of pulmonary edema and cyanosis.
Severe preeclampsia is an indication for immediate delivery. Seizures in eclampsia should be regarded as provoked, occurring against the background of acute brain damage. Encephalopathy in eclampsia develops as a result of impaired autoregulation of cerebral blood flow and increased capillary permeability. This leads to cerebral edema, the development of multiple microhemorrhages and disseminated intravascular coagulation, which is the cause of attacks. The risk of eclampsia is not always proportional to the severity of arterial hypertension. In young primiparous women with initial arterial hypotension, eclampsia can develop with an average blood pressure of 120–130 mm Hg. Art. Therefore, effective antihypertensive therapy is required in all cases of preeclampsia, although this does not have a significant effect on the transition to eclampsia. Among antihypertensive drugs, vasodilators should not be prescribed, since they have the ability to enhance the increase in perfusion cerebral edema.
Another area of therapy is seizure control. In the past, benzodiazepines and phenytoin were used to relieve attacks. Currently, a solution of magnesium sulfate is considered the most effective remedy. As a prophylactic agent for severe preeclampsia in the antenatal period, magnesium sulfate can be administered intramuscularly, or intravenously in the presence of seizures. The drug is administered intravenously in a slow stream at a dose of 4 g (16 ml of a 25% solution), and then 1 g (4 ml of a 25% solution) every hour during the day. On the first day, additional administration of 2–4 g of magnesium sulfate may be necessary if attacks continue. Subsequently, they switch to intramuscular administration of the drug.
During therapy, monitor the level of urine output (more than 100 ml/h), the frequency of respiratory movements (more than 12 per minute) and the preservation of tendon reflexes. A change in these indicators indicates the toxic effect of magnesium sulfate. To adjust the dosage, intravenous bolus injection of 10 ml of a 10% calcium gluconate solution is used. Calcium channel blockers (nifedipine) should not be prescribed together with magnesium sulfate due to the common mechanisms of action of these drugs.
If therapy with magnesium sulfate is ineffective, additional administration of a diazepam solution of 10 mg 1–2 times/day is used. The lack of effect of such therapy indicates the need for intravenous barbituric anesthesia.