Epilepsy is a chronic brain disease that manifests itself as uncontrollable seizures. They arise as a result of a pathologically enhanced impulse in the cerebral cortex. The disease is characterized by a wave-like course - after an attack there comes a period of remission. Clinical manifestations of the disease depend on the location of the lesion, the severity and type of seizures. At the Yusupov Hospital, neurologists diagnose epilepsy using the latest methods. For complex therapy, modern medications are used that are effective and have a minimal range of side effects.
Causes
One of the main causes of epilepsy is considered to be a hereditary predisposition: if parents have a history of seizure symptoms, then the child is more likely to develop them. Epilepsy also develops under the influence of the following reasons:
- Traumatic brain injury;
- Cerebrovascular accidents;
- Cerebral vascular dysplasia;
- Volumetric formations in the cerebral cortex;
- Neurosurgical intervention;
- Infectious diseases of the central nervous system;
- Previous ischemic or hemorrhagic stroke.
The occurrence of epileptic attacks is caused by the presence in the cerebral cortex of a stable focus with epileptic activity. Convulsive activity from the primary focus can spread through commissural fibers, cortical neuronal complexes, and the centrencephalic system of the brain. In the presence of increased convulsive activity over a long period of time, secondary lesions arise. They can, under the influence of certain factors, become independent and independent. As a result, the attack in the primary focus fades, but not in the secondary. This picture is observed in patients after two years of illness. Over the course of some time, tertiary foci of seizure activity may develop in the cerebral cortex.
Epilepsy can develop under the influence of the following provoking factors:
- Hormonal imbalances;
- Alcoholism and drug addiction;
- Chronic stress;
- Excessive emotional stress;
- Chronic fatigue.
Secondary attacks of epilepsy occur in patients suffering from brain tumors, cerebral vascular pathology, after hemorrhage in the head, due to poisoning with toxic substances.
It is very important to identify the disease early to reduce the likelihood of complications. Which doctor treats epilepsy? For quality therapy, it is necessary to be observed by a neurologist, epileptologist, or psychotherapist. As clinical symptoms progress, assistance from a physiotherapist or pharmacologist may be required.
Causes
Epilepsy is a polyetiological disease. Among the main causes of the development of the disease are the following conditions:
- Hereditary burden. If one family member is diagnosed with epilepsy, subsequent generations of relatives are at risk.
- Excessive alcohol consumption. Alcohol abuse increases the risk of developing seizures. Irreversible pathological changes occur in the brain that lead to seizures.
- History of traumatic brain injury. Epilepsy is considered a complication of brain injury.
- Cerebrovascular accident. Most often, epilepsy after a stroke occurs in older people.
Other predisposing factors include:
- intrauterine infection;
- birth injury;
- tumor formation of the brain;
- excessive fatigue and psycho-emotional arousal.
Expert opinion
Author: Daria Olegovna Gromova
Neurologist
Epilepsy is one of the common and dangerous neurological diseases. The first seizure can occur at any age. In children, seizures are recorded starting at 4-5 years of age. According to statistics, every 20th person has experienced an attack of increased brain activity at least once in his life. Doctors do not identify the exact causes of seizures. The first attack of epilepsy can be triggered by various factors.
The Yusupov Hospital uses modern medical equipment to diagnose epileptic conditions. With its help, it is possible to determine the localization of the pathological focus. Timely detection of epilepsy allows the initiation of correct treatment. Properly selected and high-quality therapy helps achieve stable remission. Experienced neurologists at our hospital prescribe proven medications with proven effectiveness. Medications are included in the list of the latest European recommendations for the treatment of epilepsy. To minimize relapse, each patient is provided with preventive recommendations developed on an individual basis.
Frequency of epileptic seizures
The frequency of attacks can vary from once every 2-3 months to single or multiple daily. A seizure can be triggered by sleep disturbances, stress, excessive alcohol consumption, long stays in a stuffy room, sudden flashes of light, etc. At the moment, the specific factor influencing the increase in the frequency of seizures is not yet known.
Expert opinion
Author: Daria Olegovna Gromova
Neurologist
Epilepsy has been considered one of the most dangerous and common diseases for many years. According to WHO statistics, 4-10 people per 1000 population suffer from seizures. Doctors note an annual increase in cases of onset of epilepsy. Thanks to numerous clinical studies, it has been proven that the disease is registered 2-3 times more often in countries with low and medium levels of development. This is due to the presence of a greater number of provoking factors, such as infections and a high level of injuries. According to statistics, 80% of patients with epilepsy live in such conditions.
The exact causes of seizures are still unknown. Doctors distinguish several types of seizures, as well as the factors that cause them. When selecting therapy, neurologists and epileptologists at the Yusupov Hospital take into account all the data. If you follow the rules of prevention and take anticonvulsants, about 70% of patients can live for a long time without seizures. An individual epilepsy treatment plan is developed for each patient at the Yusupov Hospital. The drugs used meet European quality and safety standards. In addition, patients are provided with personalized preventive recommendations that minimize the risk of epilepsy relapse.
Causes and symptoms of epileptic seizures
Convulsions occur in response to various negative factors. A single case of seizures is not a reason to diagnose a disease such as epilepsy. You can suspect it only if the seizures recur. They are also characterized by spontaneity, that is, they appear unexpectedly, for no apparent reason.
To answer the question of why epilepsy is dangerous and what its consequences are, it is necessary to understand what exactly triggered the development of the epileptic focus. The most common reasons include:
- heredity;
- traumatic brain injuries, concussions;
- cerebrovascular accidents (epilepsy can occur due to stroke);
- drug and alcohol addiction;
- pathological development of the fetus (if a woman has an epileptic attack during pregnancy, this can lead to serious consequences for the child, including the development of the same disease);
- parasitic diseases and brain tumors.
Factors that negatively affect the functioning of the brain lead to the appearance of an area that at any moment can give rise to an epileptic seizure. The cause could be anything from bright flashes of light, open flames, certain food additives and ingredients, certain medications, and more. At the time of an attack, a person is not able to control his actions, so the risk of injury is very high. As a rule, the first epileptic seizure occurs at an early age (before 18 years). In adults, epilepsy develops less frequently, but this makes its consequences no less dangerous. Unfortunately, at the moment there is no exact answer to the question of whether the disease is congenital or acquired.
Depending on the reasons for the development of the pathological focus, the most common types of disease are distinguished:
- Focal epileptic form. It is a hereditary disease that develops subsequently from congenital disorders.
- Symptomatic epilepsy. Hereditary predisposition also plays a role in the development of the disease, but most often it is provoked by external factors. In their absence, a person will never experience an epileptic seizure and will not face its consequences.
- Epileptiform syndrome. The occurrence of a convulsive epileptic attack as a result of a sharp external influence.
- Temporal lobe epilepsy. The most common form of the disease, characterized by the localization of the pathological focus in the temporal region of the brain.
Often, doctors cannot accurately determine which of the above conditions is observed in a patient. Therefore, during the examination, the mechanisms of epilepsy development are discussed in order to determine what consequences they may have on the brain.
Different types of epilepsy manifest themselves in their own way, and therefore the consequences of the disease are very diverse. However, for all forms there is a common number of characteristic symptoms. The number of damaged brain cells plays a key role in the intensity and duration of epileptic seizures. Symptoms of seizures range from mild convulsions to brief fainting. In addition, the nature of seizures can change over the course of the disease, and if left untreated, epilepsy will have serious consequences.
There are several constant characteristic features of epileptic seizures:
- Sudden onset. If a person suffers from epilepsy, it is impossible to accurately predict when the next seizure will occur. This feature is the main factor that has negative consequences for the psyche. A patient with epilepsy constantly arrives in anticipation of an attack and experiences nervous tension. At the same time, many people with this disease experience a so-called aura - a short-term condition accompanied by discomfort in the abdomen, the sensation of various odors, spots before the eyes, a feeling of anxiety, buzzing in the ears, etc. In this way, patients can recognize the onset of an epileptic attack and take measures aimed at eliminating its consequences.
- Non-duration. In epilepsy, a seizure lasts from a fraction of a second to several minutes. Depending on the form of the disease, the patient may behave differently: one freezes and does not even notice the seizure, while another may lose consciousness. There may also be several attacks. They come one after another, and this is the most dangerous condition for the patient.
- Abrupt cessation. Epilepsy attacks end as suddenly and unexpectedly as they begin. Often, stopping a seizure does not even require the use of medications. They are necessary only in the case of a series of attacks or in situations where the cause was a specific factor. Medicines should also be used for childhood epileptic seizures accompanied by high fever.
- Repetition of the same seizures. If an attack of one type occurs, its manifestation in the future will be the same. But if epilepsy is left untreated, the consequences of the disease will be more severe and severe seizures.
A disease such as epilepsy invariably leaves its mark on the lives of people suffering from it. It is impossible to get used to seizures, and after each attack a person feels broken and empty.
Expert opinion
Author: Olga Vladimirovna Boyko
Neurologist, Doctor of Medical Sciences
For many years, epilepsy has been considered a dangerous neurological disease. The prevalence of the disease is 4-8 people per 1000 population. According to statistics, 80% of patients with epilepsy live in countries with low or medium levels of development. The danger of seizures lies in their consequences. Attacks occur unexpectedly, which leads to falls and injuries. 30% of patients become disabled in groups 1 or 2.
To date, doctors have not been able to determine the exact causes of epileptic seizures. At the Yusupov Hospital, diagnostics are carried out using European medical equipment: CT, MRI, EEG. Modern drugs are used to treat epilepsy and its consequences. They are included in the list of the latest world standards for the treatment of epileptic seizures. An individual therapeutic plan is developed for each patient - experienced neurologists and epileptologists take into account the characteristics of the development of the disease, the patient’s age and concomitant conditions. Specialists at the Yusupov Hospital provide preventive recommendations that reduce the risk of recurrent attacks. If medical prescriptions are followed, most patients go into long-term remission.
Precursors of epileptic seizures
The first harbinger of epileptic seizures is an aura. It is individual for each patient. Thanks to the constant warning signs, patients can warn others about the onset of an attack or independently move to a safe place.
There are the following types of aura that precede the onset of an epileptic attack:
- Hallucinations;
- Sharp contraction of the muscles of the upper or lower extremities;
- Repeating the same movements;
- Burning, crawling or tingling sensation in various parts of the body;
- Sharp deterioration in mood.
The duration of the aura is several seconds. During this time, patients do not lose consciousness.
Types of seizures in epilepsy
Depending on the cause of occurrence, the following types of epileptic seizures are distinguished:
- Idiopathic – occurring in the presence of epilepsy in close relatives;
- Symptomatic – occur after a traumatic brain injury, infectious or tumor lesion of the brain substance;
- Cryptogenic – the causes of occurrence cannot be determined.
The external manifestations of a convulsive syndrome are determined by its type. If the pathological focus is localized in one hemisphere of the brain, simple or complex seizures occur.
Make an appointment
Simple partial seizures
Against the background of simple convulsions, the patient does not always lose consciousness. Clinical symptoms depend on the location of the pathological focus in the cerebral cortex. The average duration of simple partial seizures is two minutes.
Neurologists identify the following main signs of the disease:
- Emotional lability;
- Hallucinations of various types;
- Twitching in various parts of the body;
- Cardiopalmus;
- Feeling of nausea;
- Frequent feelings of deja vu;
- Difficulty understanding and reproducing words.
Complex partial seizures
The duration of complex partial seizures is one or two minutes. An aura appears before the attack begins. There is uncontrollable crying and screaming, repetition of words, and performance of certain movements. At the end of the seizure, patients are not oriented in space and time. A simple partial seizure of epilepsy can develop into a complex seizure.
Generalized seizures
Generalized seizures occur against the background of total brain damage. They are as follows:
- Tonic;
- Clonic;
- Tonic-clonic;
- Atonic;
- Myoclonic.
With tonic spasms, unconscious muscle contractions occur. Patients are bothered by severe pain in the muscles of the back, upper and lower extremities. Tonic convulsions rarely lead to fainting. The attack lasts no more than twenty seconds. Tonic seizures can occur during sleep.
Patients with epilepsy are less likely to experience clonic seizures. They manifest themselves as uncontrolled paroxysmal muscle contractions. During convulsions, foam is released from the patient's mouth. He loses consciousness. Paralysis may develop. Clonic seizures occur due to severe stress, traumatic brain injury, cerebrovascular accident, or brain tumor. During an attack, short-term muscle tension is replaced by relaxation. The attacks quickly follow each other.
The most typical and characteristic of an epileptic attack are tonic-clonic convulsions. Their duration varies from 1 to 3 minutes. If tonic-clonic seizures persist for a longer period of time, calling an ambulance is recommended. Neurologists distinguish tonic and convulsive phases in the course of an attack. In the tonic phase, the patient loses balance and consciousness, in the convulsive phase, involuntary muscle contractions occur. After the attack is over, patients do not remember what happened.
Tonic-clonic seizures may also be accompanied by the following symptoms:
- Increased salivation;
- Sweating;
- Involuntary tongue biting;
- Injury as a result of uncontrolled actions;
- Involuntary urination or defecation;
- Blueness of the skin.
Atonic seizures occur after a traumatic brain injury, stroke, infectious inflammatory processes, or in the presence of a brain tumor. During an attack, the patient loses consciousness for a while and falls. In some cases, convulsions can be expressed by twitching of the head. The attack lasts about 15 seconds. At the end of it, the patient does not remember what happened.
Myoclonic seizures are characterized by rapid jerking of various parts of the body. The attack resembles jumping inside the body. Most often, muscle contractions occur in the upper half of the body, the area of the upper and lower extremities. Myoclonic spasms can occur when falling asleep or waking up. A symptom of an attack may be hiccups. The duration of the attack is several seconds. During myoclonic seizures, patients do not lose consciousness.
Causes of acquired epilepsy
This pathology is secondary, formed under the influence of a large number of unfavorable factors associated with the transfer of a certain type of disease. Acquired epilepsy manifests itself immediately or after some time. Experts advise timely treatment of disruptions in metabolic processes, viral diseases, and in case of a head injury, seek professional help at a clinic.
The main causes of the symptomatic variety of the disease:
- head injuries, concussions, bruises and skull fractures, which violate the integrity of internal structures and can spur the onset of a seizure;
- infectious diseases such as meningitis, encephalitis and abscess;
- prolonged fever, when body temperature significantly exceeds acceptable levels;
- tumor-like neoplasms in the head;
- vascular disorders;
- presence of multiple sclerosis;
- intoxication with narcotic substances;
- alcoholism;
- drug overdose;
- birth injuries in a child associated with hypoxia, head contusion.
Researchers have proven that endogenous substances, more precisely amino acids, polypeptides, monoamines and acetylcholines, play an important role in the development of seizures. All of them perform mediator functions of various directions. Glycine and taurine are responsible for the inhibitory function of the nervous system, and acetylcholine and glutamic acid are responsible for the excitatory function. During the formation of a paroxysmal focus, the balance between these substances is disrupted, which leads to the appearance of corresponding symptoms.
Currently, there is a lot of controversy about the congenital predisposition of a person to the appearance of convulsive activity.
Is acquired epilepsy inherited? Most scientists believe that it is not epilepsy itself that is inherited, but only a certain degree of convulsive readiness. That is, the predisposition itself, which, under the influence of a large number of (external or internal) unfavorable factors, can spur further growth of the paroxysmal focus.
Expert opinion
Author: Georgy Romanovich Popov
Neurologist, Candidate of Medical Sciences
Every year there is an increase in the number of people suffering from seizures. WHO provides the following data: 4-10 people per 1000 population have epilepsy. In Russia, the incidence rate accounts for 2.5% of cases. Epileptic seizures occupy one of the first places in the structure of disability. In the absence of timely treatment, patients become disabled in groups 1 or 2. When studying the causes and factors leading to relapse of seizures, doctors established a certain pattern. Epilepsy is diagnosed several times more often in countries with low and middle levels of development. According to statistics, 80% of patients live in such conditions.
Epilepsy is divided into several types. Acquired is not detected as often as compared to other forms of pathology. Doctors at the Yusupov Hospital are paying attention to finding out the possible causes of the disease. Thanks to this, it is possible to choose effective treatment. It has been proven that if the rules of prevention are followed and anticonvulsants are taken, 70-80% of patients can live for a long time without relapse. An individual epilepsy treatment plan is developed for each patient at the Yusupov Hospital. The drugs used meet European quality and safety standards. Personal preventive recommendations provided to all patients help minimize the risk of recurrence of epileptic seizures.
Clinical picture
During the occurrence of seizures, neurons work to the maximum, expending their energy. This enhances oxidative processes in brain cells. The consequence of this is relative hypoxia, when the organ does not receive enough oxygen; it is observed in different parts and is expressed unevenly.
As attacks progress, oxygen deficiency increases due to increased contractility of the muscular system. Generalized paroxysms that continue for a long time can lead to cerebral edema. Changes occur in vasomotor reactions, blood flow in the vessels is weakened. All this contributes to the appearance of acute disorders in neurons and cells of small vessels.
Seizures result in single or multiple damage to nerve fibers, which over time causes cell necrosis and hemorrhage. Subsequently, morphological changes in the brain contribute to a decrease in its volume.
Patients with severe disease are at risk with a high mortality rate. It is very important to provide timely assistance to such patients, since morphological changes during a prolonged attack may be incompatible with life.
Can epilepsy be acquired? Everything will depend on the cause of its occurrence; in adulthood, the development of symptomatic pathology is associated with the influence of unfavorable factors: numerous diseases, poisoning, drug overdose, head injuries.
Nocturnal epilepsy
In one third of patients, epilepsy attacks occur at night. Pathological signs may appear when falling asleep, during sleep, or during awakening. Nocturnal epilepsy occurs under the influence of the following factors:
- Hereditary predisposition;
- Suffered traumatic brain injury;
- Excessive consumption of alcoholic beverages;
- Sleep disorders;
- Prolonged psycho-emotional stress.
The duration of a nocturnal epilepsy attack varies from a few seconds to five minutes. Most patients do not remember the seizures that occurred. Some people clearly describe the sensations they experience. An epileptic attack that occurs during a dream is accompanied by the following manifestations:
- A sharp, causeless awakening;
- Feeling of nausea, which may result in vomiting;
- Severe headache;
- Tremor;
- Pronunciation of unusual sounds;
- Speech impairment.
During a nocturnal epilepsy attack, patients may perform rash actions. They get down on all fours or pretend to ride a bicycle. You can suspect the presence of a nocturnal attack based on the following indirect attacks:
- Tongue bite:
- Traces of blood on the pillow after waking up;
- Bruises and abrasions on the body;
- Painful muscle syndrome;
- Wet bed due to loss of urinary control;
- Uncontrolled urination;
- Waking up in an unusual place (on the carpet, on the floor).
These symptoms are individual for each patient. They appear with one degree or another. Therefore, neurologists believe that nocturnal epilepsy attacks are very difficult to diagnose.
Rolandic epilepsy
Epilepsy of this type is focal and genetically determined. It manifests itself in rare attacks at night, they affect one half of the face with the tongue and pharynx. The Rolandic type is characterized by partial epileptic seizures without loss of consciousness.
The first sign of onset is tingling or numbness on one side of the face, lips, gums, or tongue. Afterwards motor paroxysms develop.
Make an appointment
Symptoms of nocturnal epilepsy
Epileptic seizures during sleep occur in 30% of patients with this type of pathology. In this case, seizures are most likely the day before, during sleep or just before waking up.
Sleep has fast and slow phases, during which the brain has its own peculiarities of functioning.
During the slow phase of sleep, the electroencephalogram records an increase in the excitability of nerve cells, the index of epilepsy activity, and the likelihood of an attack. During the fast phase of sleep, the synchronization of bioelectrical activity is disrupted, which leads to the suppression of the spread of electrical discharges to neighboring parts of the brain. This generally reduces the likelihood of an attack occurring.
When the fast phase is shortened, the threshold for seizure activity decreases. Sleep deprivation, on the contrary, increases the likelihood of frequent seizures. If a person does not get enough sleep, he becomes drowsy. This condition is very similar to slow sleep phase, which causes abnormal electrical activity in the brain.
Seizures are also triggered by other sleep problems, for example, even a single sleepless night can cause someone to develop epilepsy. Most often, if there is a predisposition to the disease, development is influenced by a certain period during which the patient had a clear lack of normal sleep. Also, in some patients, the severity of attacks may increase due to disturbances in sleep patterns, too sudden awakenings, from taking sedatives or overeating.
The symptoms of nocturnal epilepsy attacks, regardless of the patient’s age, can be varied. Most often, nocturnal seizures are characterized by convulsions, tonic, clonic seizures, hypermotor actions, and repetitive movements. With frontal autosomal nocturnal epilepsy, during attacks the patient may walk in his sleep, talk without waking up, and experience fear.
All of the above symptoms can appear in all sorts of combinations in different patients, so there may be some confusion when making a diagnosis. Sleep disturbances are typical manifestations of various pathologies of the central nervous system, not just epilepsy.
Alcoholic epilepsy
This type of epilepsy develops in patients who abuse alcohol. Seizures occur due to irreversible pathological processes in the cerebral cortex. Epilepsy attacks caused by alcohol intoxication most often occur in patients suffering from the following concomitant diseases:
- Atherosclerosis;
- Consequences of traumatic brain injury;
- Brain tumors;
- Residual effects of previously suffered infectious and inflammatory diseases of the brain.
The cause of the disease may be aggravated heredity. The symptoms of alcoholic epilepsy have some peculiarities. The disease does not necessarily begin with a convulsive syndrome. Initially, the following pathological signs appear:
- Increased salivation;
- Marked weakness throughout the body;
- Paleness of the skin;
- Blueness of lips;
- Dizziness;
- Strong headache;
- Loss of consciousness;
- Nausea, vomiting;
- Uncontrolled urination;
- A spasm of the vocal cords that causes a person to emit a high-pitched scream.
An attack of alcoholic epilepsy can result in respiratory arrest and death.
Clinical picture of epilepsy
In the epilepsy clinic they talk about three periods:
- ictal (moment of attack);
- postictal (the moment following the attack; during this period, the symptoms of the disease may be completely absent, except for those symptoms that clearly indicate epilepsy: ischemic stroke, traumatic brain injury));
- interictal (time between attacks).
In addition to periods of epileptic seizures, there are several types of auras that accompany a partial epileptic seizure, among these auras: motor, speech, vegetative, mental, sensory.
Among the most typical symptoms of epilepsy are:
- nausea;
- headache;
- dizziness;
- general weakness;
- a feeling of squeezing in the throat and chest;
- numbness of lips and tongue;
- feeling of constant drowsiness;
- sound hallucinations;
- feeling of a lump in the throat;
- paroxysms of an olfactory nature.
As is known, partial seizures of a complex type most often occur with the performance of so-called automated movements, which are characteristic of patients with epilepsy. In such cases, it will not be possible or quite difficult to communicate normally with the patient.
Epilepsy of newborns
Up to one year, a baby may experience the following types of epilepsy seizures: small, large and nocturnal. During a minor attack, the child throws back his head and freezes in one position. His gaze is directed to one point. The baby does not respond to stroking and sound and rolls his eyes. His body temperature may rise.
A major seizure of epilepsy is manifested by the fact that the child stretches out, bends his legs and assumes a fetal position. Convulsions, loss of consciousness and respiratory arrest occur.
During a night attack, the baby suddenly awakens and screams. His face changes. After an attack, the child cannot fall asleep for a long time. Children suffering from epilepsy may lag behind their peers in development, their memory is impaired, and mental health problems occur.
Pediatric epilepsy
Epilepsy in children is manifested by the following symptoms:
- Tonic-clonic seizures;
- Absences (minor seizures);
- Myoclonic convulsions with and without disturbance of consciousness.
This condition occurs due to the immaturity of the child’s brain, when processes of excitation, burdened heredity or organic brain damage predominate. Initially, warning signs of a seizure occur: headache, irritability, and a feeling of fear. In the generalized form of the disease, the child groans, screams and loses consciousness. All his muscles tense, his jaw clenches, breathing stops, his pupils dilate, his face becomes cyanotic.
The child's legs stretch and his arms bend at the elbows. After the completion of the tonic phase of the seizure, clonic convulsions occur. The child's breathing becomes noisy and foam comes out of the mouth. He bites his tongue. Involuntary urination and defecation occur. Minor seizures do not last long.
Absence epilepsy
This is idiopathic generalized epilepsy that occurs in preschool children. Characteristic symptoms: short-term loss of consciousness during the daytime, less often at night. This does not affect neurological status or intelligence in any way.
The attack begins suddenly, the child seems to freeze and does not react to any stimuli, his gaze is directed to the side. This condition lasts no longer than 15 seconds and is rare in isolated form. More often it is supplemented by throwing the head back, rolling the eyes, and possibly repeating some actions: stroking hands, licking lips, repeating words or sounds. The child does not remember what he did.
If severe fatigue, drowsiness are added to the symptoms, and the attack lasts for a long time, then this indicates an unfavorable course of the disease.
Epilepsy: how it happens
Death from attacks not classified as SUDEP can be caused by a number of factors, including:
- a fall
- inhalation of vomit
- drowning in several tens of centimeters of water, for example, in a bath
- concussions, head injuries, or brain bleeding
- breathing problems
Although the cause of sudden death syndrome in epilepsy is by definition unknown, there are theories to suggest why death occurs. Pausing breathing can cause oxygen levels in the brain or blood to decrease in a life-threatening manner.
An attack can compress the airways, leading to suffocation.
Other causes are centered around the heart. Some experts suggest that cardiac arrhythmia or cardiac arrest may lead to SUDEP. SUDEP can also occur due to a combination of cardiac and respiratory factors.
Other types of epilepsy
Temporal lobe epilepsy
It is characterized by the localization of the focus of epileptic activity in the temporal lobe of the brain. It manifests itself in simple and complex partial epileptic seizures. As the disease progresses, secondary generalization occurs. The patient experiences mental health disorders.
Structural focal epilepsy
The onset of the disease occurs in individuals of various age groups. The lesion is located in the temporal zone of the brain. The patient feels time speeding up or slowing down. He perceives a familiar environment as new, and a new incident as something that has been experienced for a long time.
An epileptic seizure is manifested by the following symptoms:
- Preserved consciousness;
- Turning the eyes and head towards the localization of the focus of increased activity;
- The appearance of gustatory and olfactory paroxysms;
- The presence of auditory and visual hallucinations;
- Systemic dizziness.
The patient complains of pain in the heart, stomach, nausea, heartburn, and suffocation. There is a disturbance in the rhythm of cardiac activity, an increased feeling of fear, chills, and pale skin. As temporal lobe epilepsy progresses, a secondary generalized form of the disease develops. The attack is manifested by tonic convulsions in all muscle groups, loss of consciousness.
Post-traumatic epilepsy
Develops as a result of meningitis, encephalitis, traumatic brain injury, asphyxia. The disease is more often diagnosed in children. The attack is not accompanied by loss of consciousness or occurs with impaired consciousness. If the patient loses consciousness, they may experience a secondary generalized seizure. The muscles of the foot and upper limbs are involved in the convulsive process.
Why is an epileptic seizure dangerous?
During a tonic-clonic seizure, breathing stops, and in all other seizures with convulsions, additional trauma is possible due to hitting the head on a hard surface. Falls from one's own height and loss of consciousness are also dangerous. Each seizure that occurs damages the neurons of the brain, which subsequently leads to a decrease in cognitive and mental abilities, and changes in the psyche.
This does not prevent patients with epilepsy from leading an active life. However, some aspects are limited - it is prohibited to drive a car and work in production in workshops, with open fire or at height, as well as in work that requires frequent switching of attention. Properly selected therapy can increase the interictal period by months or even years.
Make an appointment
Conclusions:
- Patients with epilepsy should avoid sleep deprivation, irregular sleep patterns, and remember to take medications regularly.
- Nutrition for epilepsy does not differ from the diet of healthy people.
- Mental, mood and thinking disorders occur in 20-25% of patients with epilepsy (i.e. only 1/4 of patients), and in most cases they are not severe.
- Patients with epilepsy can and should engage in sports (or physical therapy), observing certain rules and restrictions.
- Patients with epilepsy can watch TV and work on the computer, following a number of rules for photosensitivity forms.
- Flights, as a rule, do not provoke attacks if the sleep/wake pattern is not disrupted. When preparing for your trip, take the necessary set of medications and a card with your details and doctor’s contact details.
- Alcohol increases the frequency and severity of attacks. Drinking alcohol is not allowed!
- Some medications can trigger seizures in people with epilepsy, so always talk to your doctor before taking any new medication!
Diagnostics
Diagnosis of the disease occurs by taking an anamnesis. The specialist listens to complaints, on the basis of which a preliminary diagnosis can be made.
After this, the patient is sent for laboratory and hardware examinations, which makes it possible to differentiate epileptic seizures from other pathologies, allows one to find out the cause, the nature of the changes, determine the form and prescribe treatment.
The diagnosis is made by neurologists and epileptologists who determine the causes of epilepsy in adults using indications obtained from a comprehensive comprehensive examination.
Instrumental diagnostic methods
The safest hardware diagnostics is an EEG. It has no contraindications; it can be used to detect areas of paroxysmal activity. These can be sharp waves, spikes, slow waves. Modern EEG makes it possible to identify the exact localization of the pathological focus.
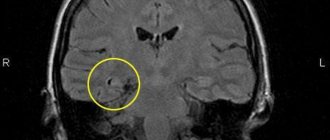
The most informative neuroimaging method is brain MRI. The study allows us to identify the initial cause of the deviation and determine the location of the lesion in the central nervous system.
Laboratory diagnostic methods
Epilepsy occurs under the influence of various reasons; in order to identify the presence of infection, inflammation, hormonal imbalances, genetic defects, the patient needs to take a general blood test, biochemical, molecular genetic, and check the tumor marker.
When to ask for help
At the first attack, you should immediately consult a doctor for a diagnosis. Once the doctor has made a diagnosis and treatment plan, the patient must be monitored regularly.
If attacks become more severe, more frequent, or change in any way, the patient should talk to their doctor again.
If a patient wants to stop taking anticonvulsants, they should also consult with their doctor to discuss the benefits and risks.
First aid for seizures
Proper care for an epileptic seizure reduces the risk of complications and injuries. The person who happens to be next to the patient should catch him and prevent him from falling. You also need to do the following:
- Place a blanket, pillow or cushion of clothing under your head;
- Free your neck and chest from constricting objects and clothing (tie, shirt, scarf);
- Carefully turn the patient's head to the side to minimize the risk of inhalation or passive reflux of vomit or own saliva;
- Open your mouth and put a cloth or handkerchief in it to prevent the patient from biting his tongue;
- Do not forcefully open your mouth;
- If breathing stops for a long time, perform artificial ventilation from the mouth to the nose or mouth.
During an attack, the patient may experience involuntary urination or bowel movements. This manifestation of epilepsy should not cause fear in others. After an attack, patients usually experience drowsiness and severe weakness.
Treatment
Neurologists at the Yusupov Hospital provide complex treatment for epilepsy. It is aimed at reducing the frequency of epileptic seizures and stopping medications during remission. According to statistics, in 70% of cases, adequately selected treatment helps to almost completely relieve paroxysmal activity in patients.
To achieve optimal results in treatment, patients are prescribed drugs for epilepsy of the following properties:
- anticonvulsants – help relax muscles, they are prescribed to both adults and children;
- tranquilizers - allow you to remove or reduce the excitability of nerve fibers; the drugs have shown a high degree of effectiveness in the fight against minor attacks;
- sedatives – help relieve nervous tension and prevent the development of severe depressive disorders;
- injections - used for twilight states and affective disorders.
Idiopathic focal epilepsy is benign. It requires symptomatic treatment. In focal forms with seizures that appear in series 2-3 times a month and are accompanied by an increase in mental disorders, neurosurgeons perform surgery.
Is epilepsy curable?
Before starting treatment, a diagnosis should be determined, because loss of consciousness and various convulsions can occur due to a sharp drop in blood sugar, anemia, poisoning, high fever, cerebrovascular accident, calcium deficiency and other conditions. Antiepileptic drugs cannot be prescribed to such patients immediately. The diagnosis of epilepsy is made only when epileptic seizures recur.
With adequate treatment, according to generalized statistics, a good therapeutic effect is achieved in 80-85 percent of patients, and in 60-70 percent of patients seizures can be eliminated completely. And this is a very good reason to stop antiepileptic drugs.
The percentage of patients with epileptic seizures could be significantly lower if patients took medications regularly and did not stop treatment on their own. The decision to discontinue medications can only be made by a doctor, and not earlier than after 5 years of treatment, if during this time the patient has not had epileptic seizures. At the Yusupov Hospital, an epileptologist always monitors how the patient’s illness develops.
Epilepsy
Conservative therapy
All treatment methods for epilepsy are aimed at stopping seizures, improving quality of life and stopping taking medications (in remission).
In 70% of cases, adequate and timely treatment leads to the cessation of epilepsy attacks. Before prescribing antiepileptic drugs, it is necessary to conduct a detailed clinical examination and analyze the results of MRI and EEG. The patient and his family should be informed not only about the rules for taking medications, but also about possible side effects. Indications for hospitalization are: the first epileptic seizure in life, status epilepticus and the need for surgical treatment of epilepsy. One of the principles of drug treatment of epilepsy is monotherapy. The drug is prescribed in a minimum dose and then increased until the attacks stop. If the dose is insufficient, it is necessary to check the regularity of taking the drug and find out whether the maximum tolerated dose has been reached. The use of most antiepileptic drugs requires constant monitoring of their concentration in the blood. Treatment with pregabalin, levetiracetam, valproic acid begins with a clinically effective dose; when prescribing lamotrigine, topiramate, carbamazepine, it is necessary to slowly titrate the dose.
Treatment of newly diagnosed epilepsy begins with both traditional (carbamazepine and valproic acid) and newer antiepileptic drugs (topiramate, oxcarbazepine, levetiracetam), registered for use as monotherapy. When choosing between traditional and new drugs, it is necessary to take into account the individual characteristics of the patient (age, gender, concomitant pathology). Valproic acid is used to treat unidentified epileptic seizures.
When prescribing this or that antiepileptic drug, you should strive for the minimum possible frequency of taking it (up to 2 times a day). Due to stable plasma concentrations, long-acting drugs are more effective. A dose of the drug prescribed to an elderly patient creates a higher concentration in the blood than a similar dose of the drug prescribed to a young patient, so it is necessary to start treatment with small doses and then titrate them. The drug is discontinued gradually, taking into account the form of epilepsy, its prognosis and the possibility of resumption of attacks.
Surgery
Drug-resistant epilepsy (continuing seizures, ineffectiveness of adequate antiepileptic treatment) requires additional examination of the patient to decide on surgical treatment. Preoperative examination should include video-EEG recording of seizures, obtaining reliable data on the localization, anatomical features and nature of the spread of the epileptogenic zone (MRI).
Based on the results of the above studies, the nature of the surgical intervention is determined: surgical removal of epileptogenic brain tissue (cortical topectomy, lobectomy, hemispherectomy, multilobectomy); selective surgery (amygdala-hippocampectomy for temporal lobe epilepsy); callosotomy and functional stereotactic intervention; vagus stimulation.
There are strict indications for each of the above surgical interventions. They can only be carried out in specialized neurosurgical clinics that have the appropriate equipment, and with the participation of highly qualified specialists (neurosurgeons, neuroradiologists, neuropsychologists, neurophysiologists, etc.).
Forecast
The prognosis for epilepsy if you follow medical recommendations and take medications in a timely manner is favorable.
To do this, it is important for a person to maintain a careful attitude towards his health: maintain a daily routine, have adequate sleep, avoid overexertion, and completely give up bad habits such as cigarettes and alcohol. Loss of ability to work depends on the frequency of attacks: if they are episodic and occur at night, then there are no contraindications to performing work functions. Daytime attacks with loss of consciousness cause limited choice of work.
In most clinics, patients with epilepsy are seen by neurologists or psychotherapists, who sometimes find it difficult to understand the details of diagnosis and the intricacies of treatment of this disease. Just one EEG requires enormous experience and skills of a professional. Therefore, the Yusupov Hospital employs highly specialized epileptologists who can answer all your questions. You can make an appointment with them by calling the Yusupov Hospital.
Make an appointment
Prognosis for epilepsy
The patient's prognosis for recovery and future work will depend on the frequency of attacks. As practice shows, at the stage of remission, epileptic seizures rarely appear, most often at night. In most cases, the patient remains competent and able to work, and can return to his usual activities and live a normal life. For those who have had epilepsy, it is very undesirable to work at night and go on business trips. Periodically, daytime attacks may recur, which are accompanied by loss of consciousness, thereby limiting the person’s usual ability to work.
Epilepsy has a negative impact on all areas of human life, so today this disease is considered one of the most significant socio-medical problems of humanity.
A big disadvantage for modern medicine is the fact that very little is still known about the nature of epilepsy, which means it is also impossible to properly inform the patient.
The vast majority of patients who received correct and timely treatment continue to lead normal lives.