Epilepsy refers to diseases that manifest themselves with different symptoms and have different origins. The clinical picture of the disease is described in many manuals, and there are more than 65 types of epileptic diseases in the world. This is due to various factors that provoke the appearance of specific seizures, which in turn become permanent.
Epilepsy is a chronic non-infectious disease that forms in the brain tissue and provokes the release of neurons into the body, resulting in uncontrolled seizures, convulsions, loss of consciousness, etc. Each type of pathological lesion has different manifestations. In particularly difficult cases, an epileptic seizure is accompanied by loss of orientation in space, fainting and uncontrolled urination. Often an attack is caused by profuse salivation, which is popularly defined as “foaming at the mouth.”
However, medicine, in the course of its development, has formed a specific therapy for each type of disease, but even with such diversity and possibilities, there remain certain forms of the disease that are not amenable to drug therapy. For example, a pharmacoresistant form, in which the affected areas of the brain do not respond to the components of the drugs, and the clinical picture remains unchanged. A person continues to have seizures, his condition worsens due to constant exhaustion of the body - the tension of muscle tissue during seizures is several times higher than normal. In such cases, surgical treatment is used, aimed at partial or complete removal of the affected cells or their direct stimulation.
Benefits of use
Surgical interventions for such pathologies have been practiced for more than 100 years. Thanks to the developed branch of neurosurgery and innovative developments in the field of medicine, their effectiveness is 80%. People who undergo surgery manage to completely get rid of chronic seizures and return to a full life. Modern technologies make it possible to create a detailed map of the areas of the brain that are responsible for the vital functions of the body - speech, movement, memory and coordination. This approach to therapy allows you to reduce the risk of complications after manipulation to a minimum.
Indications for surgical treatment
It is known that this disease is as diverse as the factors that provoke it. Therefore, in each individual case, therapy is selected solely based on the patient’s medical history and test results, CT or MRI diagnostics, as well as EEG. There are two types of treatment for this pathology:
- medicinal;
- surgical.
Epilepsy surgery is an intervention on the brain in which the doctor removes or isolates the area where the seizure occurs. The doctor chooses the type of surgery depending on how and in which zone the epileptic impulse spreads. It is the location of the affected areas that largely determines the methods of intervention and the use of specific equipment. The possibility of surgical treatment is discussed when a number of conditions are met:
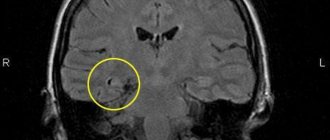
- The disease has a focal (focal) character. The epileptogenic region of the brain is precisely determined, the removal of which will relieve the patient from seizures.
- Weighing the risks. Any surgical activity should not lead to a deterioration in the person’s quality of life due to neurological or neuropsychological deficits.
- The form must be exclusively pharmacoresistant, that is, at least two drugs have no effect on the affected areas.
Since the operation is prescribed in special cases, preparation and preliminary procedures before the intervention also require attention. Through proper diagnosis and examination, a complete picture of the onset and development of the disease in the patient is often restored.
Examination and tests before surgery
The high effectiveness of such radical treatment can only be achieved with strict adherence to all standards of preparatory examinations carried out before the day of surgery. They include:
- MRI according to the epileptic scanning program;
- EEG video recording, which is mandatory for any form of pathology;
- a detailed description or video of attacks that were recorded at home;
- study of the patient’s neuropsychological profile to confirm pre-existing deficits in mental functions;
- analysis of possible risk factors and complications that may arise during and after surgery;
- consultation with an epileptologist.
Surgical manipulations are carried out only in specialized centers and specialized clinics with the mandatory presence of resuscitation equipment.
Surgical treatment in adults and children is carried out according to a similar protocol, except for cases of pathological formations in the brain, when the presence of a histologist and oncologist is necessary. The best results are achieved when the manipulations are performed by a neurosurgeon specializing in the treatment of epilepsy.
Intracranial EEG recording
EEG (electroencephalogram) is a diagnostic test that patients with any damage or pathology of the brain must undergo. This method allows us to establish normal electrical activity and identify pathological potential of the brain and disturbances in its structure. EEG is widely used for:
- epilepsy;
- differential diagnosis of epileptic seizures;
- non-epileptic paroxysmal states.
EEG cannot be assessed as the main source of diagnosis. By its specificity, most of the indications are passive. Registration of EEG data in the absence of significant stimuli does not allow us to determine the reactivity of certain normal rhythms and obtain a detailed picture with reliable information about pathological activity.
Side effects from medications
As practice has shown, after a certain period after the selection and forced increase in doses of drugs, their side effects develop (toxic, allergic, metabolic, hematological), sensitivity decreases, refractoriness and other negative consequences appear (increased attacks, deterioration of mental activity, drug-induced illness).
Many of these conditions are caused by the consequences of brain injury (including birth) or certain disorders (including hereditary) of metabolic processes in the corresponding structures of the brain (amino acids, lipids, catecholamines, polysaccharides, etc.), causing the appearance of a multifocal epileptic complex, foci of congestive excitations that form “convulsive readiness,” as well as diffuse changes in the brain leading to the same consequences (without the possibility of strict local identification of the paroxysmal focus on the EEG).
Almost all such conditions and disorders are characterized by one or another severity and high variability of psychoneurological disorders, forcing patients to go to many medical institutions. Often, as a result, they receive huge quantities and large doses of drugs, very often without any noticeable and stable results.
Specialists more often encounter in practice such variants of paroxysmal conditions as epileptoid syndromes in various pathological conditions (including brain injuries) and genuine epilepsy (grand ta1 and petit ta1); Gilles de la Tourette's disease and syndrome; paroxysms in cerebral palsy, rheumatism, etc.
Types of surgical treatment
Surgical treatment in Russia is based on several techniques that are widely used throughout the world and have excellent success rates in practice. However, it is worth noting that 100% effectiveness is ensured not by the method of surgical intervention, but by other factors that determine the period of the disease, the degree of brain damage, the stage of development and the individual physical and neurological data of the patient. Therefore, it is almost impossible to select the most effective method. Main types of interventions:
- resection of the temporal lobe;
- lesionectomy;
- callosotomy of the corpus callosum;
- functional hemispherectomy;
- vagus nerve stimulation;
- multiple sublial dissections;
- implantation of the RNS neurostimulator.
The choice of a specific type of operation depends entirely on the doctor, who, based on existing data about the patient’s condition and test results, approves the method that is most effective in a particular example. In complex, atypical situations, a council with the participation of several specialized doctors gathers and a decision is made on a certain type of surgical therapy.
Temporal lobe resection
Removal of the temporal lobe of the brain or individual structures through a lateral approach. This surgery may involve removal of the amygdala/hippocampus. The introduction and use of EEG showed that the cerebral scar and the surrounding medulla are an epileptogenic focus that causes seizures of varying strength. As a result, this led medicine to the conclusion that temporal lobe epilepsy is an almost independent nosological form. Resection surgical methods are used in cases where the patient has undergone complete diagnostics and drug therapy, which has not yielded results.
Statistics from the Ministry of Health indicate that 50% of all cases of pathology are complex partial epilepsy. The results of various researchers in the field of medicine and neurosurgery show that after surgical treatment of this pathology, in 70–90% of patients, attacks are completely stopped or become rare. Based on these data, a modification of anterior lobectomy with resection of the lateral cortex exclusively was proposed. Over the course of many years of practice and healing, it was announced that resection of the affected parts of the temporal lobe makes it possible to completely get rid of epileptic seizures.
Lesionectomy
It is known that in epilepsy, brain tissue is mostly affected. Under strong pressure from the release of neurons, tissues quickly wear out, and healthy tissue begins to gradually disintegrate and is replaced by a structurally altered cell, which is an uncharacteristic node. Lesionectomy is a less popular therapy, but it is also effective in certain cases.
These manipulations are surgical interventions aimed at removing isolated non-functioning areas of the brain that have arisen as a result of trauma, cancer, malformation of blood vessels and other formations that provoke seizures. To a greater extent, this operation has an effect. Patients can be completely or partially relieved of attacks and then follow the doctor's recommendations to avoid stressful situations in everyday life.
Callosotomy of the corpus callosum
Callosotomy is a separate type of surgery used in the treatment of epileptic pathology. It involves cutting the corpus callosum, namely the structure responsible for connecting both hemispheres of the brain. Prescribed to patients who have generalized seizures and bilateral independent epileptic bursts in the frontal lobes. In addition, the category of patients for whom this therapy is recommended includes patients with frequent attacks, accompanied by a rapid loss of muscle tone (the person falls). Often during such seizures, injuries and damage to the musculoskeletal system occur, so such surgery should be performed at the first manifestations of epileptic cases. The operation itself involves neutralizing the rapid movement of convulsive activity from one lobe to another. Such interventions rarely provoke complications, so those operated on quickly go through the rehabilitation period and return to normal life.
Functional hemispherectomy
An option recognized throughout the medical world in the treatment of symptomatic forms of drug-resistant focal epilepsy in patients with malformations of the brain and some acquired lesions of one of its hemispheres. The prognosis for the effectiveness of this method depends on many factors, not the least of which are the age and physical condition of the patient. This method is considered the most risky because it has a lot of contraindications. Those who undergo the procedure face a long road to recovery as it is used to diagnose catastrophic epilepsy, which is accompanied by severe seizures with loss of consciousness and increased uncontrollable salivation.
This procedure is used to treat various seizure disorders when the source of the epilepsy is localized to a wide area of one hemisphere, especially Rasmussen's encephalitis. Surgical intervention is carried out during a “calm” period, when a person does not experience prolonged seizures that provoke complete exhaustion of the body. It is used when medications, other types of surgery, or less invasive procedures that significantly impair function or put the patient at risk for further complications have failed.
Vagus nerve stimulation
Unlike other listed methods, vagal stimulation is prescribed in cases where drug treatment does not produce results, and other operations cannot be performed due to certain reasons and contraindications. The vagus stimulator itself consists of a pulse generator with a battery and a connecting wire with platinum electrodes. They are attached under the left subclavian region, and the electrodes are fixed on the person’s cervical area. The introduction of a foreign body itself is carried out using two small incisions, so it is difficult to call this procedure a surgical intervention. It takes no more than 1–1.5 hours and is performed under general anesthesia. Operating principle:
- the generator sends electrical impulses at certain intervals;
- the frequency of stimulation and its activity is regulated by the doctor;
- carried out on an outpatient basis;
- the increase in intensity depends on the effectiveness of vagus nerve stimulation.
With some experience, a person can independently regulate the strength and intensity of stimulation. As an attack approaches, it is possible to prevent the spread of epileptic activity, thereby stopping the attack at the initial stage.
Multiple sublial dissections
This procedure makes it possible to control seizures that occur in areas of the brain where they cannot be safely removed. In medical practice, against the background of progression of lesions of an epileptic nature, there are cases where, in the course of work, damaged areas with an irreversible process of decay were removed. Patients experienced severe headaches, attacks increased and became more severe, which led to partial loss of sensation in the limbs.
The procedure itself looks quite simple and safe. The surgeon makes several small incisions in the brain tissue. These cuts significantly reduce the number of seizures, but do not affect normal brain activity, which preserves all the functionality of the body and intelligence. However, such manipulations require extreme concentration and care, since any unnecessary or excessively deep incision will provoke irreversible processes.
Implantation of the RNS neurostimulator
The RNS neurostimulator is designed to control the electrical activity of the brain in patients with epilepsy and prevent convulsive contractions by suppressing unnatural impulses in neurons. This device was developed by American scientists and is widely used in practice throughout the world. The use of this device stimulates:
- resumption of correct speech;
- memory and attention;
- ability to concentrate;
- performance;
- social activity.
The entire system consists of implantable and external components. In the first case, it is the neurostimulator itself; in the second, it is a laptop with an adapted program that allows you to monitor brain activity and the release of neurons. The RNS system also makes it possible to view the patient's electroencephalogram in real time.
What is post-traumatic epilepsy?
This type of epilepsy occurs in young people after suffering traumatic brain injuries.
The severity of post-traumatic epilepsy directly depends on the severity of the injury. The highest risk of developing this disease is in patients who have been unconscious for more than a day, with a cerebral hematoma, depressed injuries to the skull, penetrating gunshot wounds to the head, as well as in victims with damage to the temporal lobe of the brain and the mediobasal parts of the frontal lobe. Post-traumatic epilepsy is characterized by partial convulsive seizures, which occur as a result of damage to a local area of the brain, and can be simple or severe. With simple partial seizures, consciousness is not impaired in patients, with complex ones, consciousness is lost, with secondary generalized seizures, the appearance of a convulsive attack involving the entire muscle group is noted.
At the beginning of the development of partial seizures, convulsions appear that seize the muscles of the hands and feet, after which they spread to the entire limb. Sometimes cramps begin to appear in the facial muscles. Before the development of a seizure with loss of consciousness, the patient experiences the appearance of auditory and olfactory hallucinations, tachycardia, increased sweating, and frozen gaze.
Patients with post-traumatic epilepsy may experience memory loss, character changes, mood swings, and dementia. Post-traumatic epilepsy develops within 5 years after the injury, most often during the first two years, especially if the patient has suffered repeated trauma, drinks alcohol or is in a stressful situation.
For patients admitted with traumatic brain injuries, doctors at the Yusupov Hospital Neurology Clinic prescribe a comprehensive examination using modern diagnostic equipment (including metabolic neuroimaging, magnetic resonance imaging, video-EEG monitoring), and determine the prognosis of the disease given the existing risk of post-traumatic epilepsy. If the disease is detected, it is recommended to take modern antiepileptic drugs that help prevent seizures. Neuroprotective drugs are also effective.
Treatment of a patient with convulsive syndrome begins in the acute period after a traumatic brain injury, after which maintenance therapy is prescribed, which is continued for about a month. At the end of the course of treatment, a diagnosis is made and a prognosis for the likelihood of developing post-traumatic epilepsy is determined.
If the patient's condition improves and the prognosis is favorable, the medications are gradually discontinued over the course of a month. In case of an unfavorable prognosis, the patient will have to take antiepileptic drugs for a longer time.
Make an appointment
The effectiveness of surgical treatment for epilepsy
Surgical interventions, due to their specificity, always have areas of risk that are determined before the start of the procedure. To do this, a complete clinical picture of the pathology is collected and a decision is made to use one of the types of therapy that is most suitable for a particular patient. The effectiveness is also difficult to determine, since many factors depend on the individual and the extent of damage to healthy cells. Therefore, each type has its own advantages and disadvantages.
Even if the indications for surgery are the same in different people, this does not guarantee a similar result. Many people face problems that arise during the rehabilitation period. Each patient tolerates such manipulations in his own way, but even with such uncertain prognosis, medicine promises a positive result.
Forecast
After the operation, the patient must undergo a certain course of rehabilitation, constantly being under the supervision of a doctor. During this period, some examinations, tests and diagnostics will again be carried out. This is necessary to determine the preservation of functionality and the ability to think and make decisions quickly. A number of specific trainings are also carried out, during which stressful conditions are created and neurological processes in the cerebral cortex are observed. In other words, with correct and objective therapy, as well as consistent recovery after surgery, a person can count on a life without attacks and feelings of anxiety.
How is epilepsy treated?
Primarily antiepileptic drugs. The standard rule is that treatment should begin with one broad-spectrum drug. If the prescribed medicine is not effective enough, then another drug is prescribed taking into account the type of attack, form of epilepsy, and the presence of concomitant diseases. In the absence of attacks and serious side effects, treatment continues continuously for several years, after which complete discontinuation of the drugs is possible.
In severe cases, steroid hormones, a ketogenic diet, or neurosurgery are added to the basic drugs.