- general information
- Causes
- Symptoms
- Consequences
- How to avoid
- Treatment
- Conclusion
Attention! Drug use causes irreparable harm to health and poses a danger to life!
Ethanol and its metabolites have a toxic effect on neurons. Systematic abuse triggers degenerative processes in the central nervous system. Alcoholic epilepsy occurs in the absence of structural damage in the brain and is considered a severe consequence of chronic intoxication. A favorable prognosis is possible only if you completely abstain from alcohol and undergo a rehabilitation course.
general information
Alcoholic epilepsy is a pathological condition that develops in response to prolonged intoxication with ethanol and its breakdown products. The pathological condition is not always characterized by the occurrence of convulsive attacks.
Alcoholic epilepsy is a secondary neurological disorder (symptomatic). Chronic alcoholism leads to damage to neurons in the brain. Disruption of electrical conductivity between neurons causes convulsive paroxysms. The pathological condition often develops in patients with alcoholism. But there have been isolated cases where a single use of a large dose of ethanol led to a seizure.
The term alcoholic epilepsy was coined in 1883. The condition was characterized by the occurrence of convulsive seizures in alcoholics. The root cause has always been organic damage to brain cells due to the toxic effects of ethanol. Almost all patients have a history of traumatic brain injuries of varying severity.
Convulsive syndrome in alcoholism / V.V. Donskoy, N.S. Sukhanova, A.M. Gusev, M.V. Kolontai – Omsk Psychiatric Journal. — No. 2 (2). – 2014.
Almost 30% of chronic alcoholics suffer from alcoholic epilepsy. Frequency of seizures depending on the stage of alcoholism:
| Alcoholism stage | Probability of occurrence |
| I | 17 – 20 % |
| II–III | 60 – 64 % |
| III | 17 – 19 % |
In all cases, the attacks occurred against the background of prolonged and daily drinking of alcohol. But at the same time, there were no epileptic signs on the EEG.
In the international classification of diseases, alcoholic epilepsy is not assigned a code. This condition is considered within other categories or subcategories of diseases.
The term alcoholic epilepsy characterizes several pathological conditions:
- An epileptic seizure is a single or episodic reaction of the central nervous system, against the background of alcoholic excess in persons who do not suffer from alcoholism. The reaction occurs as a result of a post-intoxication state (hangover);
- Episyndrome – systematic attacks. Occurs as a result of chronic alcoholism;
- True alcoholic epilepsy is episodic or systematic seizures with convulsive or non-convulsive status.
Seizures with systematic alcohol abuse are considered harbingers of alcohol psychosis.
Get help now
Do any of your relatives or friends have an addiction? Have you tried in every possible way to help, but as a result the person still returned to his past life?
You are not the first to encounter this problem, and we can help you.
We guarantee anonymity, we will persuade you to undergo treatment, and we will help you choose a center.
Call us
+7
or
Call me
Treatment calculator
Field score:
Total score:
Patient age
Length of use
What he uses Has he previously undergone treatment Consent to treatment Concomitant diseases Employment
Waiting for values to be entered
The greatest likelihood of alcohol-induced epilepsy occurs in people with the following diseases:
- skull injuries;
- circulatory disorders;
- atherosclerosis;
- past infectious diseases;
- in the presence of neoplasms;
- with a genetic predisposition (a blood relative suffered from epilepsy).
How to avoid an epileptic attack from alcohol?
Alcoholic epilepsy develops only when there is a developed dependence on alcoholic beverages. To avoid seizures, it is necessary to carry out full treatment of alcoholism.
Causes
The root cause of alcoholic epilepsy is often organic damage to brain cells as a result of a “toxic attack.” This is preceded by a long “experience” of abuse or periodic use of surrogate alcohol.
But there are also risk factors that can cause an attack, regardless of the duration of alcoholism:
- History of traumatic brain injury;
- Cerebrovascular pathologies;
- Compounded hereditary history (epilepsy);
- Neuroinfections.
Alcohol seizures are considered to be quite rare and the most severe symptom of chronic alcoholism.
It is believed that a pathological symptom appears with a continuous history of alcoholism of at least 7–10 years. But there are known cases of seizures occurring after 1–2 years of systematic abuse.
Chronic alcoholism causes metabolic disorders in the central nervous system. Intracellular disorders are characterized by a failure in the transport of calcium and chlorine, as well as dysfunction of gamma-aminobutyric acid receptors. Pathological metabolic effects are temporary and disappear completely after alcohol withdrawal.
Clinical and neurophysiological features of epilepsy in alcohol abusers / V. O. Generalov, T. R. Sadykov, A. I. Fedin, Yu. V. Kazakova, L. P. Mishnyakova, E. V. Amcheslavskaya - Bulletin of the Russian State Medical University. - No. 5 - 2009. - 45 - 46 p.
Content:
- Why does the disease occur?
- Signs of violation
- Hidden epilepsy attacks
- Diagnostics
- First aid to a patient
- Treatment of alcoholic epilepsy in the clinic 6.1. Coding as a way to treat alcoholic epilepsy
As a result of taking high doses of alcoholic beverages, a person may experience signs of alcoholic epilepsy.
As a rule, they are non-convulsive, but are sometimes accompanied by convulsions. Typically, the disorder is diagnosed in people at the second and third stages of alcohol addiction. Only sometimes does it occur with occasional consumption of very high portions of alcohol. More often than others, men between the ages of thirty and forty experience it.
Symptoms
An attack of true alcoholic epilepsy is a harbinger of alcohol withdrawal. That is, a seizure always occurs as a result of alcohol withdrawal after prolonged or periodic ethanol intoxication. The pathological condition develops several days after withdrawal or against the background of a sharp decrease in the daily dose of alcohol.
During an alcoholic seizure, the clinical picture is homogeneous. But the severity of symptoms and the nature of manifestations may differ.
| Alcoholism stage | Probability of occurrence |
| I | 17 – 20 % |
| II–III | 60 – 64 % |
| III | 17 – 19 % |
An attack of alcoholic epilepsy occurs suddenly and without warning. Sometimes there is an atypical scenario of a non-convulsive seizure. A person falls into a kind of stupor, after which a disorder of speech and thinking occurs. The moment of the attack is completely amnesic.
Narcologists noted that in a state of alcoholic intoxication the convulsive threshold is high, so seizures do not occur. But with the formation of withdrawal syndrome, the convulsive threshold becomes significantly lower. Before an attack, anxiety increases, and visual or auditory hallucinations may occur. In isolated cases, before fainting, victims feel a second of numbness in the leg. The attack lasts on average 3 minutes and in most patients occurs while awake.
A severe form of epileptic seizure is considered to be a recurrence of a seizure after a short time interval - a transition to epileptic status.
After an epileptic seizure, the victim regains consciousness and feels overwhelmed. Sleep sets in for a few hours. In some patients, a full-blown attack does not occur. A day after stopping alcohol, only burning pain in the muscles occurs.
First group
This group of patients is the largest and makes up 85% of all patients with seizures of epilepsy who abuse alcohol.
Clinical features:
— convulsive attacks occur 6-48 hours after stopping alcohol consumption (withdrawal attacks);
- in all cases, attacks of alcoholic epilepsy are preceded by binge drinking from 2-3 days to several weeks;
- characterized by generalized tonic-clonic seizures.
- other types of seizures do not occur in such patients.
Diagnostics:
- when performing an EEG (electroecephalography) during sleep, while awake and during functional loads, epileptic brain activity is not detected.
Treatment:
— patients in this group often make the false conclusion that seizures are not associated with alcohol, since they appear only in sobriety when withdrawing from alcohol. As a result, patients perceive alcohol as a therapeutic factor that improves well-being and has an anticonvulsant effect.
— the doctor’s task is to show the patient a clear relationship between the end of the binge and the occurrence of seizures of alcoholic epilepsy and prescribe effective anti-alcohol treatment;
- when stopping a convulsive attack or treating a withdrawal condition, it is necessary to prescribe diazepam, vitamin B1 and potassium supplements;
— withdrawal seizures do not require specific anticonvulsant maintenance treatment; to prevent seizures, it is enough for this group of patients to be sober.
Consequences
Alcoholic epilepsy is not characterized by personality changes of the epileptic type. But chronic alcoholism, as a rule, leads to degradation. Therefore, attacks aggravate existing changes in personality traits and cognitive sphere (deviant behavior, irritability, anger, decreased intellectual abilities).
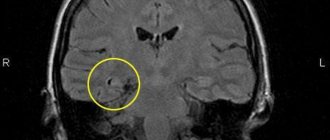
When epileptic seizures with convulsive syndrome occur, in 100% of cases, patients are diagnosed with alcoholic encephalopathy, which is characterized by irreversible degenerative changes in the brain.
Complications:
- Traumatic brain injury during a seizure;
- Development of psychotic disorders;
- Retraction of the tongue during an epileptic attack or aspiration of vomit;
- Stopping breathing;
- Cognitive changes;
- Disability.
The frequency of seizures in alcoholic epilepsy does not exceed 2–3 episodes per year. But its danger lies in its transition to a chronic form. Attacks no longer occur against the background of intoxication, but even during a long period of sobriety. This is due to the formation of a pathological focus of excitation in the brain, which causes an epileptic attack.
In chronic alcoholism, epileptic activity is detected on the EEG. That is, the mechanisms of epileptogenesis were launched in the hippocampal parts of the brain - a carrier of epileptic activity. Continuation of alcoholism will lead to the manifestation of unprovoked epileptic seizures.
Alcoholic epilepsy / V.O. Generalov, T.R. Sadykov, Yu.V. Kazakova, V.G. Amcheslavsky, E.V. Amcheslavskaya, S.A. Likhachev, E.V. Veevnik - a manual for doctors. – Moscow – Minsk. – 2014. – 6 – 13 p.
Common symptoms of alcoholic epilepsy
This disease is chronic and is expressed in a predisposition to the occurrence of convulsive attacks. During a seizure, there is a risk of injury to the head, back, limbs, and chest due to a sharp fall. During an attack, the body of a sick person bends in an unusual way. Breathing becomes hoarse , head throws back. An alcoholic seizure of epilepsy has the following symptoms:
- loss of consciousness;
- a sharp change in complexion (pallor gives way to blue around the mouth);
- loss of motor self-control;
- foam at mouth;
- muscle cramps;
- eye rolling.
During an attack, a person may bite their tongue. The attack is often preceded by loss of appetite, insomnia, anger, and headache. Alcoholic epilepsy has different consequences, including the risk of an attack while sober, not while drinking alcohol.
Alcoholic epilepsy may be accompanied by visual, auditory and tactile hallucinations due to a sharp deterioration in mental health as a result of addiction to ethyl drinks. The visions are nightmarish.
Features of alcoholic epilepsy
After an attack, withdrawal symptoms such as depressive mood, psychosis, and insomnia are pronounced. A person becomes more aggressive , gets offended over trifles, and looks for reasons for quarrels. Deterioration of behavior occurs due to personality degradation. A tendency to epilepsy makes a drinker more embittered and is fertile ground for despair. After an attack, a person may fall into a deep sleep and be bothered by disturbing thoughts. Sometimes there are specific symptoms in alcoholics prone to epilepsy, such as shuddering, talking during sleep, sleepwalking.
During an attack, some patients experience a state of alcoholic absence seizure . It is a type of epileptic attack, which is characterized by non-convulsive paroxysms. There is muscle relaxation, lack of tone and unfocused gaze. Seizures can be single or multiple. Frequent convulsions begin with a stonic phase, which lasts up to 20 seconds. Afterwards it gives way to clonic (approximate duration 120 seconds).
Treatment
An epileptic seizure can occur at any stage of alcoholism. It is impossible to cope with the disease on your own. A generalized attack of alcoholic epilepsy is a life-threatening condition. Therefore, treatment is carried out only in a hospital setting.
There is no specific therapy for alcoholic epilepsy. Drug treatment is carried out to maintain the functioning of vital organs and systems. And also to reduce the risk of secondary complications. The main condition for a favorable prognosis is complete abstinence from alcohol.
Symptomatic therapy:
- Stopping a convulsive attack. Systematic use of anticonvulsants to increase the seizure threshold;
- Prevention of cerebral edema and cardiovascular pathologies - forcing diuresis;
- Muscle relaxants;
- Maintaining water and electrolyte balance;
- Rehabilitation therapy – vitamins, nootropics.
After stabilization of the condition, it is recommended to undergo comprehensive rehabilitation in specialized institutions. With timely treatment of alcoholism, the prognosis is usually favorable.
One of the most important stages of alcohol addiction rehabilitation is psychotherapeutic correction. Its tasks and specific techniques change at each stage of the treatment process. It is especially important that the patient acknowledges his problem and the need for treatment.
Fundamentals of narcology: textbook. Benefit /M. M. Burkin, S. V. Goranskaya. – Petrozavodsk. : Karelia, 2002. – 71 – 73 p.
First attack, help and treatment
The symptoms and frequency of attacks may not worsen for a long time, even without treatment. Seizures do not in all cases progress to the next stage of the disease, which is more severe. If a person has an attack, you should immediately call an ambulance and perform the following actions.
- Place the patient on a soft surface to avoid injury. Hold the patient's head so that he does not injure himself due to seizures.
- Do not let the person leave, especially if there are any risk factors in the environment. It is important to calm him down as much as possible during seizures.
- Turn the patient's head to the side to prevent him from suffocating .
- If a person has clenched his jaw tightly, you should not forcefully try to open his mouth.
- Monitor the time of the attack, if after 5 minutes there is no improvement, immediately call an ambulance. Usually an epileptic seizure lasts no more than 2-3 minutes.
- If the patient's clothes are tight or it is difficult for him to breathe, you need to take them off, do not stand over him in a crowd, open the windows.
- Turned on side immediately after the end of the attack.
- Do not wake the patient if he has fallen asleep. You should call an ambulance so that doctors can determine further actions and begin treatment.
The difference with ordinary epilepsy is that in an addicted person, after stopping drinking alcohol, seizures can completely stop. By eliminating the provocateur in the form of alcohol, after the first attack it is possible to avoid the disease and further attacks.