Meningitis is characterized by inflammation of the meninges of the spinal cord and brain. The disease is classified as infectious. Meningitis affects adults and children. In children, meningitis often occurs in a fulminant or acute form. Adults are more likely to suffer from meningitis caused by meningococcal infection; women are sick less often than men.
The Yusupov Hospital diagnoses and treats meningitis. In the laboratory you can undergo a number of tests for the causative agent of the disease, and experienced doctors provide consultations in the hospital. Meningitis can have a fulminant course, in which case qualified assistance should be provided immediately. With meningitis, it is very important that the diagnosis be made in the first days of the disease.
Causes of meningitis
Meningitis can be of infectious or non-infectious origin. The infectious form of the disease develops as a result of the penetration of microorganisms into the body: bacteria, viruses, fungi and parasites. Non-infectious meningitis develops in patients as a result of taking certain medications and the formation of tumors.
In medicine, classification is used according to the type of pathogenic microorganisms. It is important for a modern person to know how to recognize meningitis and what types of disease exist:
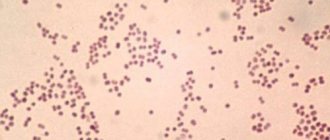
- bacterial meningitis is most often caused by streptococci, meningococci, pneumococci and Haemophilus influenzae, which are transmitted by airborne droplets;
- viral meningitis. The most common form of the disease. This type is characterized by the least severity. The causative agents of viral meningitis are enteroviruses;
- fungal meningitis develops as a result of the activity of certain types of fungal microorganisms;
- parasitic meningitis.
The list of therapeutic measures for meningitis is determined by the factors that caused the development of the disease. Thus, when treating bacterial meningitis, antibiotics are prescribed, which are ineffective for viral meningitis. If a person knows how to recognize meningitis, then the likelihood of diagnosing the disease at the initial stage and the effectiveness of therapeutic measures are high.
To determine the causes of meningitis, specialists at the Yusupov Hospital use modern diagnostic equipment. An important advantage of examinations at the Yusupov Hospital is that patients do not need to wait in lines, since appointments with specialists can be made in advance.
Expert opinion
Andrey Igorevich Volkov
Neurologist, Candidate of Medical Sciences
For several years in a row, infectious diseases have been among the causes of the development of pathologies of the nervous system. Meningitis accounts for 30-40% of cases. Modern drugs and high-quality diagnostics do not guarantee the absence of death. Mortality is explained by late seeking of medical help. Doctors associate this with the atypical course of meningitis, when the symptoms are not specific for a long time.
It is not possible to determine meningitis on your own. The clinical picture of the disease is varied. Signs differ according to the etiological factor. The initial symptoms of meningitis are often mistaken for cold symptoms. As the infection spreads, the condition worsens sharply. The high risk of death due to meningitis persists for 1-2 days from the onset of the first pathological symptoms. Delayed diagnosis and therapy lead to the development of severe, life-threatening complications. Therefore, it is important to immediately consult a doctor if you suspect the development of meningitis. At the Yusupov Hospital, the examination takes a minimum amount of time. The treatment plan is determined in accordance with the identified pathogen.
Risk group
Children and the elderly are at risk for meningitis. In addition, this disease is often diagnosed in people with an absent spleen and immunodeficiency.
The spread of meningitis, like all other infectious diseases, is more active in crowded places, closed groups, for example, in kindergartens, schools, student dormitories, barracks, since it is easier to get meningitis if you are in the company of asymptomatic carriers.
Most often, meningitis is transmitted by airborne droplets. This mechanism of infection transmission is considered the most common and characteristic of meningitis of viral origin. The infectious agent is transmitted through coughing, sneezing, kissing and sexual contact.
Newborn babies can become infected from an infected mother through the birth canal. The likelihood of infection is especially high in children born by caesarean section. Bacterial and viral meningitis can be transmitted this way.
Infection with meningitis can occur through the oral-fecal route: through dirty food or untreated water.
In addition, meningitis can develop as a result of the bite of an insect or animal that carries an infectious agent.
Expert opinion
Andrey Igorevich Volkov
Neurologist, Candidate of Medical Sciences
Meningitis of any origin is a dangerous infectious disease that affects adults and children. Without timely treatment, death occurs in 80% of cases. It has been proven that, despite the initiation of therapy, 10% of patients die within the first day from the onset of pathological symptoms. Meningitis most often affects children. Viral etiology accounts for 60–70% of cases. Fungal meningitis accounts for 1–3%. It is not possible to diagnose and treat an infectious disease at home. Therefore, it is necessary to seek medical help soon after the first signs of the disease appear.
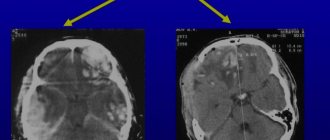
The most informative method for diagnosing meningitis is lumbar puncture. The causative agent of the disease is sown in the cerebrospinal fluid. To identify the localization of the pathological focus in the brain area, neurologists at the Yusupov Hospital prescribe MRI and CT. Etiotropic therapy is selected depending on the results obtained. Symptomatic treatment is aimed at alleviating the general condition. Vaccination is considered the only reliable means of preventing meningitis.
Symptoms of meningitis in adults
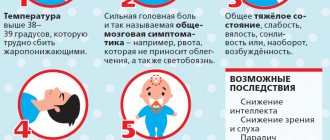
Meningitis usually has a sudden onset. The first symptoms of meningitis in adults are: fever, headaches, vomiting (the so-called meningeal triad). However, these pathological signs of meningitis also accompany other infectious diseases, so it is important to know the features of the manifestation of meningitis.
Meningitis is characterized by rapid development with pronounced signs of intoxication:
- headache;
- high fever and chills;
- confusion and loss of consciousness;
- convulsions;
- skin rash;
- muscle weakness;
- drowsiness;
- photophobia, increased skin sensitivity, reaction to sound;
- stiff neck;
- loss of appetite, nausea, vomiting;
- conjunctivitis;
- increased heart rate.
In patients with meningitis, the first sign of the disease is often a rash on the skin and mucous membranes. The rash is initially hemorrhagic in nature, sometimes spots and papules appear on the skin. The rash is considered an allergic reaction to medication.
Over the next few hours, hemorrhagic elements of various sizes and shapes appear. They may look like small spots or stars. Elements of the rash may merge and form spots.
Make an appointment
Headache
A severe headache should alert you. Headaches caused by meningitis feel different from other types of pain. Their intensity is much higher than that of headaches associated with dehydration or migraines. Taking over-the-counter pain medications does not provide relief.
Nausea and vomiting
Nausea and vomiting that occur with a headache are not absolute signs of meningitis. These symptoms may accompany other diseases, such as migraine. Close attention should be paid to other conditions that occur along with vomiting and nausea.
Vomiting with meningitis rarely occurs once, most often it is repeated, repeated, and is not associated with food intake.
Heat
An increase in body temperature, like other symptoms, may indicate the development of meningitis. With this disease, the temperature is usually much higher than with acute respiratory infections. In addition, taking antipyretic drugs for meningitis is ineffective - it is very difficult and short-term to reduce the temperature.
Pain in the neck
Quite often, patients with meningitis complain of pain and a feeling of tension in the neck, and it is difficult for them to turn or raise their head. This is due to pressure from the inflamed membranes of the brain. This symptom can also be observed when the neck muscles are strained or injured from a sudden movement of the head.
The suspicion of meningitis can be confirmed by bending the patient's hips in a horizontal position - the occurrence of pain in the neck while performing this movement is a sign of meningitis.
Difficulty concentrating
Inflammation of the meninges during meningitis is associated with perception difficulties in patients. It is difficult for them to read an article to the end, concentrate on a conversation, or complete the task at hand. The degree of confusion may worsen as brain swelling increases. In addition to lethargy and confusion, patients experience a drop in blood pressure, shortness of breath, and noisy shallow breathing.
Lethargy, drowsiness
Patients become unable to act independently, they develop drowsiness and lethargy. This condition occurs as a consequence of general intoxication of the body or cerebral edema. Bacterial meningitis can be accompanied by a sharp depression of consciousness and even coma.
Photophobia
A manifestation of photophobia in patients with meningitis is severe pain that occurs in bright light. The appearance of pain and sensitivity of the eyes, as a reaction to light, is considered an alarming signal, as it is a characteristic sign of meningitis.
Convulsions
Convulsions, sometimes with involuntary urination and disorientation in space, are observed in 20% of patients with meningitis. Their course is similar to epileptic, or the appearance of tremor of individual muscles and individual parts of the body is observed. The occurrence of seizures (generalized and local) is associated with irritation of the cortex and subcortical structures of the brain.
Characteristic rash
A hemorrhagic rash on the skin and mucous membranes is not a specific symptom of meningitis. It appears in 25% of patients with bacterial meningitis and is most often observed in diseases of a meningococcal nature, since it is meningococcus that causes damage to the internal walls of blood vessels. The appearance of skin rashes is usually observed 15-20 hours after the onset of the disease. In this case, the rash is polymorphic - it can be roseolous, papular, in the form of nodules or petechiae. The rashes have an irregular shape and may protrude above the skin level.
Psychomotor agitation, anxiety
Anxiety, agitation and disorientation occur in patients with a form of the disease such as meningoencephalitis at the onset of the disease. With the bacterial form of meningitis, similar symptoms may appear 4-5 days after the onset of the disease. After psychomotor agitation, patients may experience loss of consciousness or coma.
At the beginning of the disease, as well as in later stages, patients with meningitis may develop symptomatic psychosis, manifested by agitation or, conversely, lethargy, delirium, visual and auditory hallucinations.
Delusions and hallucinations can occur in patients with lymphocytic choriomeningitis and meningitis, which is caused by the tick-borne encephalitis virus.
If you have at least one of the above symptoms, you should immediately consult a doctor, since it is impossible to check meningitis yourself. To identify this disease and immediate treatment, qualified medical care is required.
The Neurology Clinic of the Yusupov Hospital offers high-quality diagnostics and treatment of meningitis of any form. The hospital's doctors use an individual approach in their work. Treatment tactics, developed individually for each patient, are explained to him in detail during the consultation process and are implemented as accurately as possible during therapeutic measures.
Expert opinion
Tatyana Aleksandrovna Kosova
Head of the Department of Rehabilitation Medicine, neurologist, reflexologist
Infectious diseases have been among the causes of death among the population for a long time. Meningitis is registered in 30–40% of cases. Unfortunately, despite the quality of the treatment, the possibility of death cannot be ruled out within the first 24 hours after the onset of clinical symptoms of the disease.
Among the etiological factors of meningitis, sinusitis is distinguished. The accumulation of purulent contents in the sinuses without proper treatment can lead to the spread of infection to the meninges. In such cases, meningitis is considered as a complication of sinusitis. The effectiveness of treatment for sinus inflammation depends on the quality of the diagnosis.
The Yusupov Hospital conducts a full range of examinations necessary to detect sinusitis and meningitis. The clinic’s doctors select the correct therapy based on the data obtained and the nature of the pathology. Doctors advise not to delay seeking medical help if symptoms of sinusitis develop and not to self-medicate. Without proper treatment, pus quickly spreads beyond the sinuses and penetrates into the brain area. An examination by a doctor will reduce the risk of a complicated course of the disease.
Meningitis
Encephalitis
Fungus
Vomit
Rubella
Measles
23459 07 June
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Meningitis: causes, symptoms, diagnosis and treatment methods.
Definition
Meningitis is an infectious inflammation of the meninges of the brain and spinal cord, accompanied by intoxication, fever, increased intracranial pressure syndrome, meningeal syndrome, as well as inflammatory changes in the cerebrospinal fluid.
The meninges are connective tissue membranes that cover the brain and spinal cord. There are dura mater, arachnoid and pia mater.
The dura mater of the brain has a dense consistency and thickness of 0.2-1 mm; in places it fuses with the bones of the skull. The arachnoid membrane is a thin, translucent, non-vascular connective tissue plate that surrounds the brain and spinal cord. The soft shell is a thin connective tissue plate directly adjacent to the brain, corresponds to its relief and penetrates into all its recesses. In its thickness is the vascular network of the brain.
The most common inflammation is inflammation of the pia mater, and the term “meningitis” is used.
Causes of meningitis
The meninges can be involved in the inflammatory process primarily and secondary. Meningitis that occurs without a previous general infection or disease of some other organ is called primary. Secondary meningitis develops as a complication of an existing infectious process. Secondary ones include tuberculous, staphylococcal, pneumococcal meningitis. The primary ones are meningococcal, primary mumps, enteroviral meningitis and others.
The disease is transmitted by airborne droplets, household contact or nutrition.
Purulent inflammation of the meninges can be caused by various bacterial flora (meningococci, pneumococci, and less commonly, other pathogens). The cause of serous meningitis is viruses, bacteria, fungi.
According to the forecast, the most dangerous is tuberculous meningitis, which occurs when there is a tuberculous lesion in the body. The development of the disease occurs in two stages. At the first stage, the pathogen, through the bloodstream, infects the choroid plexuses of the ventricles of the brain with the formation of a specific granuloma in them. In the second, inflammation of the arachnoid and soft membranes is observed (as a rule, the membranes of the base of the brain are affected), which causes acute meningeal syndrome.
The development process of meningococcal meningitis also consists of several stages:
- contact of the pathogen with the mucous membrane of the nasopharynx;
- entry of meningococcus into the blood;
- penetration of the pathogen through the blood-cerebrospinal fluid barrier, irritation of pia mater receptors by toxic factors and inflammation.
The course of the infectious process depends on the pathogenic properties of the pathogen (the ability to cause disease) and the state of the human immune system.
Previous viral diseases, sudden climate change, hypothermia, stress, concomitant diseases, therapy that suppresses the immune system can be significant for the occurrence and course of meningitis.
Classification of the disease
According to the type of pathogen:
- Viral meningitis (influenza, parainfluenza, adenovirus, herpes, arbovirus (tick-borne), mumps, enterovirus ECHO and Coxsackie).
- Bacterial meningitis (meningococcal, tuberculous, pneumococcal, staphylococcal, streptococcal, syphilitic, brucellosis, leptospirosis).
- Fungal (cryptococcal, candidiasis, etc.).
- Protozoal (toxoplasmosis, malaria).
- Mixed.
According to the nature of inflammation:
- Serous.
- Purulent.
According to the mechanism of occurrence:
- Primary.
- Secondary.
With the flow:
- Spicy.
- Subacute.
- Fulminant.
- Chronic.
By severity:
- Easy.
- Medium-heavy.
- Heavy.
According to the prevalence of the process:
- Generalized.
- Limited.
According to the presence of complications:
- Complicated.
- Uncomplicated.
Symptoms and syndromes of meningitis
There are a number of syndromes common to all meningitis:
- meningeal syndrome - manifested by rigidity (increased tone) of the neck muscles and long back muscles, hypersthesia (increased sensitivity) of the sensory organs, headache, vomiting, changes in the cerebrospinal fluid;
- cerebral syndrome - manifested by drowsiness, impaired consciousness, nausea, vomiting, dizziness, psychomotor agitation, hallucinations;
- asthenovegetative syndrome – manifested by weakness, decreased ability to work;
- convulsive syndrome;
- general infectious syndrome - manifested by chills and fever.
Meningococcal meningitis ranks first among purulent meningitis.
Its incubation period ranges from 1 to 10 days, with an average of 2-4 days. The disease usually begins acutely against the background of complete health or shortly after nasopharyngitis. Patients can indicate not only the day, but also the hour of illness; they are worried about chills, body temperature above 38℃, severe bursting headache, aggravated by any noise and movement of the head. Patients may experience pain in various parts of the body, and touching causes excruciating sensations. Vomiting is not associated with food intake and does not bring relief. Soon, stiffness of the neck and long back muscles sets in. Patients take a “meningeal” position. Infants cry constantly, they may experience bulging fontanelles and gastrointestinal disorders. Pneumococcal meningitis, as a rule, is observed in young children against the background of an existing pneumococcal process (pneumonia, sinusitis).
With streptococcal meningitis, hepatolienal syndrome (enlarged liver and spleen), renal failure, adrenal insufficiency, petechial rash (hemorrhages due to damage to the capillaries, as a result of which blood, spreading under the skin, forms round spots, the size of which does not exceed 2 mm).
Purulent meningitis caused by Pseudomonas aeruginosa and fungi are rare. The diagnosis is established only after additional laboratory tests.
Serous tuberculous meningitis is characterized by a gradual onset, although in rare cases it can manifest itself acutely. At the onset of the disease, patients complain of fatigue, weakness, irritability, and sleep disturbances. The temperature is usually no higher than 38℃, and there is an intermittent moderate headache. On the 5-6th day of illness, the temperature rises above 38℃, the headache intensifies, nausea, vomiting, and drowsiness appear. Unconsciousness develops quickly. A divergent strabismus, a low position of the upper eyelid in relation to the eyeball, and pupil dilation may be observed.
When diagnosing mumps meningitis, it is important to identify recent contact with someone with mumps.
Clinical manifestations of damage to the meninges may develop even before the enlargement of the salivary glands.
Enteroviral meningitis is characterized by two- and three-wave fever with intervals between waves of 1-2 or more days. Other manifestations of enterovirus infection are almost always observed (muscle pain, skin rash, herpangina).
For the diagnosis of measles and rubella meningitis, an indication of contact with a patient with these diseases, as well as typical clinical symptoms of measles or rubella, is of great importance.
Diagnosis of meningitis
To confirm the diagnosis of meningitis, the doctor may prescribe a set of laboratory and instrumental studies:
- clinical blood test with determination of hemoglobin concentration, number of erythrocytes, leukocytes and platelets, hematocrit and erythrocyte indices (MCV, RDW, MCH, MCHC), leukoformula and ESR (with microscopy of a blood smear in the presence of pathological changes);
Sinusitis and meningitis: the relationship of diseases
Meningitis develops as an independent disease and can be a complication of pathological processes. Sinusitis and meningitis are interrelated, since the accumulation of pus in the maxillary sinuses can cause inflammation of the lining of the brain. It is important for people at risk to know how sinusitis turns into meningitis and what symptoms the patient experiences. The development of sinusitis by contact occurs against the background of an existing infectious process. Infection accumulated in the paranasal sinuses can cause inflammation of the meninges.
The development of complications with sinusitis is rare, since modern specialists use effective treatment methods. However, if treatment is untimely and ineffective against the background of reduced immunity, the patient may develop meningitis. If a patient suspects meningitis or their health has sharply worsened, it is necessary to consult a general practitioner or neurologist, who will prescribe an examination and determine the cause of the problem.
At the Yusupov Hospital, patients are provided with a wide range of medical services, which include examinations, therapeutic measures, disease prevention and recovery after illness. If meningitis is suspected, patients are urgently hospitalized.
The most important and revealing test for suspected inflammatory processes in the membranes of the brain and spinal cord is a lumbar puncture. It is necessary to examine the cerebrospinal fluid to identify the cause of inflammation and prescribe adequate therapy.
Symptoms of viral meningitis
The incubation period for viral meningitis usually lasts 2-4 days. The disease begins acutely, with high fever and general intoxication. In patients with high body temperature, malaise increases, muscle and joint pain, nausea and vomiting, abdominal pain, and diarrhea appear. Slight drowsiness and stupor are often associated. More severe signs of meningitis (impaired consciousness, stupor and coma) are not typical for inflammation of the meninges caused by viruses and require a more in-depth examination of the patient.
From the first or second day of the disease, doctors determine a clearly defined meningeal syndrome:
- severe headache;
- repeated vomiting;
- lethargy and drowsiness, sometimes agitation and anxiety.
Patients may complain of cough, runny nose, sore throat and abdominal pain. Often, patients with viral meningitis develop skin hyperesthesia (increased sensitivity to various irritants). Upon examination, rigidity of the neck muscles and signs of severe hypertensive cerebrospinal fluid syndrome are revealed. During a lumbar puncture, clear, colorless cerebrospinal fluid flows out under pressure. An increased content of lymphocytes is determined in the cerebrospinal fluid, while the levels of protein, glucose and chlorides are within normal limits. After 3-5 days, body temperature normalizes. Sometimes a second wave of fever appears.
In patients with viral meningitis, the following meningeal signs are determined:
- Kernig's symptom - the patient cannot straighten the leg bent at a right angle;
- Brudzinski's symptom: lower (when trying to straighten one bent leg, a reflex flexion of the second leg occurs), and upper - when bending the head, involuntary flexion of the lower limb occurs;
- Babinski's symptom - dorsiflexion of the first toe occurs with streak irritation of the plantar surface of the foot.
In most adults, viral meningitis occurs without complications. Some recovering patients complain of headaches for several weeks or months. They have mild intellectual impairment, asthenia or impaired motor coordination. The prognosis for newborns and infants is unclear. They may have persistent complications in the form of intellectual impairment, learning difficulties, and hearing loss.
Diagnosis of meningitis
The diagnosis of meningitis can be made based on the results of additional studies - laboratory and instrumental:
- detailed blood test;
- fundus examination;
- X-ray examination of the skull;
- heart electrocardiograms;
- electroencephalography;
- computer and magnetic resonance imaging.
Doctors at the Yusupov Hospital confirm or refute the diagnosis of meningitis using a study of cerebrospinal fluid. A lumbar puncture is performed immediately after examining the patient. Normal cerebrospinal fluid is transparent, colorless, and flows out under a pressure of 130-180 mm during puncture. water Art. It detects from two to eight cells in one microliter. In serous meningitis, the cerebrospinal fluid is colorless, clear or opalescent. During cerebrospinal puncture, it flows out under a pressure of 200-300 mm. water Art. at a speed of 60-90 drops per minute. In the cerebrospinal fluid, from 200 to 800 cells are determined in 1 μl, 80-100% are lymphocytes. The amount of protein and glucose is increased. After the puncture, the patients' condition improves significantly.
With serous-bacterial meningitis, the cerebrospinal fluid may be colorless or yellow, opalescent. During puncture, it flows out in a stream under a pressure of 250-500 mm of water column. The number of cells increases to 800-1000 in 1 μl, they contain the same number of lymphocytes and neutrophils. Protein levels are increased and glucose concentrations are significantly decreased.
The liquor in purulent-bacterial meningitis is cloudy, whitish or greenish-brown. Due to the high viscosity and blockage of the liquor pathways, it often flows out in rare drops under high pressure. The number of cells in one milliliter of cerebrospinal fluid exceeds 1000; they consist mainly of neutrophils. Protein concentration varies from 600 to 16,000 mg/l, glucose levels are reduced.
To confirm the diagnosis of meningitis, doctors use bacteriological examination of mucus from the nasopharynx and cerebrospinal fluid. During bacterioscopic examination of cerebrospinal fluid, smears are stained with Gram or methylene blue. To exclude fungal meningitis, the specimen containing cerebrospinal fluid is stained with ink. Laboratory assistants isolate a pure culture on media with the addition of normal horse serum or cattle serum and identify it by biochemical activity and antigenic structure.
In case of viral meningitis, in preparations prepared with Gram staining and ink, it is impossible to identify the causative agent of the infection. Cultivation of bacteria and fungi also gives negative results. By culturing cellular material with standard laboratory cell lines, a pathogen serologically identical to the measles virus can be isolated. Rubella virus is isolated using the co-cultivation method.
To identify oligoclonal immunoglobulins, the method of agarose gel electrophoresis or isoelectric focusing of cerebrospinal fluid gamma globulins is used. Immunoglobulins appear in a number of viral infections. As a result of immunological studies, viral antigens or antibodies are detected in the cerebrospinal fluid, and the nucleic acid of the virus is detected using the polymerase chain reaction method. The enzyme immunoassay method detects pathogen antigens in feces, urine or saliva. Express methods allow you to quickly and early determine the presence of the herpes simplex virus antigen in the cerebrospinal fluid and blood or the DNA of the virus (using the polymerase chain reaction method).
Laboratory diagnosis of meningitis using modern research methods can be performed at the Yusupov Hospital. According to indications, doctors determine changes in brain tissue using computer or magnetic resonance imaging. If the first signs of meningitis are present, adequate antibiotic therapy is started immediately after diagnosis.
Make an appointment
Viral meningitis
A neurologist can suspect viral meningitis based on the patient’s characteristic complaints, acute onset of the disease, and the presence of meningeal symptoms. To establish the viral nature of inflammation of the meninges, a lumbar puncture is performed with examination of the cerebrospinal fluid, PCR studies and isolation of the pathogen.
Analysis of cerebrospinal fluid in viral meningitis shows a slight increase in protein, normal glucose and leukocytosis. In the first 1-2 days, viral meningitis may be accompanied by neutrophilic leukocytosis of the cerebrospinal fluid, which is more typical of bacterial inflammation. However, the absence of the pathogen during microscopy of differently colored cerebrospinal fluid smears indicates a viral etiology of the disease. To confirm it, it is necessary to re-examine the cerebrospinal fluid after 12 hours, during which, in the case of viral meningitis, a decrease in the number of neutrophils and an increase in the number of lymphocytes is observed.
Analysis of cerebrospinal fluid allows one to differentiate viral meningitis from other types of inflammation of the meninges. Thus, with leptospirosis and tuberculosis etiology of meningitis, as well as with its tumor nature, lymphocytosis observed in the cerebrospinal fluid is combined with a decrease in glucose levels.
Isolating the virus is a very difficult task, since it is contained in small quantities in the cerebrospinal fluid, and in other sources (blood, urine, feces, nasopharyngeal swab) it can be found in carriers or after an infection without the development of viral meningitis. Therefore, the main modern method for diagnosing the pathogen in viral meningitis is PCR testing of cerebrospinal fluid. Serological tests for diagnosing viral meningitis are indicative only if their results are compared at the onset of the disease and after 2-3 weeks. Due to the long duration of such diagnostics, it can only be retrospective in nature.
Patients with viral meningitis are additionally subjected to a clinical blood test, biochemical liver tests, determination of the electrolyte composition of the blood, the content of glucose, creatinine, lipase and amylase. In case of an atypical course of viral meningitis and doubts in its diagnosis, electromyography, EEG, MRI and CT of the brain are possible.
How is meningitis treated?
At the Yusupov Hospital, patients can receive a full range of medical services for the detection and treatment of meningitis, rehabilitation after illness and prevention. Patients with meningitis can contact the neurologist clinic of the Yusupov Hospital every day for 24 hours to receive emergency care.
The staff of the Yusupov Hospital follows the tradition of attentive and respectful treatment of each patient, therefore they approach the treatment of each case individually. Neurologists inform patients at risk about how to distinguish meningitis from other diseases and prevent its development.
When patients are admitted to the Yusupov Hospital, a comprehensive diagnosis is carried out, including a number of examinations to identify the causes of meningitis, collection of complaints and symptoms. Patients with meningitis need inpatient treatment, so the Yusupov Hospital has created comfortable living conditions and ensures interaction with qualified personnel.