general characteristics
There are true and false hallucinations.
True hallucinatory images have the qualities of objectivity, integrity, structure, and constancy. They are assimilated to the real situation, that is, they interact with existing objects, for example, an ax lies on the table. Pseudohallucinations are present in a conditional, imaginary space and often do not have a clear structure. Common options are voices in the patient’s head or visual images hovering in the air. The origin of pseudohallucinations is interpreted by the patient as artificially caused by another person. According to the content, hallucinations can be elementary, simple, or complex. Elementary ones have incomplete objectivity, are unimodal, are represented by individual non-speech sounds and simple images like causeless flashes. Simple hallucinatory phenomena are objective, static, sometimes move, but do not change shape. They are unimodal - they use one analyzer. Complex hallucinations are formed with the participation of several analyzers; the images are dynamic and often have semantic content. Example: the smell of poisons combined with voices behind the wall, deciding to poison the patient.
Hallucinations are varied - single and multiple images, randomly arising or connected by a common plot, neutral in relation to the patient or frightening, commanding, commenting, amusing. According to the key analyzer involved, they are divided into visual, olfactory, auditory, tactile, gustatory, visceral, motor, complex. Regardless of the cause and modality, the general characteristic is that the images are always perceived by the patient as really existing.
Effects of hallucinogens on the physical body
At the physical level, absolutely all narcotic substances reduce the level of body vibrations. The central nervous system and brain are primarily affected. Even if it is not noticeable at first, studies have shown that the clinical picture of marijuana addiction, for example, is similar in many patients. A clouded, confused, deconcentrated look into the depths of oneself, sluggish, apathetic movements, facial features are smoothed out, acquiring a characteristic appearance, by which one can say that the person is frankly becoming dumber.
Followers of the doctrine of reincarnation believe that because a person actively destroys his body in this life, he will receive a disability in the next. And since the mechanisms for working out karmic processes are accelerated, the chances of becoming disabled, or simply getting into a situation that will lead to this, increase significantly.
How does this manifest itself in practice? Yes, it's elementary. A drug addict under the influence of LSD goes out onto the road and gets hit by a car. So he is disabled. And it seems like there is no addiction, and the drug is some kind of drug, and not even really a drug, but the consequences are obvious.
And how many deaths, suicides, how many crippled destinies, ending up in prison. All this is precisely the consequence of a distortion of the work of the subtle bodies; first of all, it is this reason that influences the fact that people, having become involved with any drugs, begin to destroy themselves.
Causes of hallucinations
Hallucinations can completely change behavior, emotions, feelings and thoughts. The brighter the images, the more they control a person, “obscuring” reality. Their content and frequency vary depending on the etiological factor. The causes of hallucinations can be divided into four large groups: states of physiological or psychological stress, mental illness, neurological pathologies and substance poisoning.
Extreme conditions
Hallucinatory sensations appear in extreme situations for the body, which are often accompanied by the risk of death and are associated with a pronounced deficiency or excess of chemicals, information, and physical influences. Such phenomena cause a state of acute mental or physiological stress, and hallucinations are formed based on changes in biochemical processes in the brain. Their possible reasons:
- Overheat.
Unreal images, sounds, voices occur when body temperature rises to 41-42° C. This condition is observed with fever, severe heat stroke. Characterized by psychomotor agitation, delirium, and confusion. - Hypothermia.
Extremely low temperatures can also provoke a delusional-hallucinatory state. Symptoms develop already at a mild stage of hypothermia, when the body temperature drops below 35 ° C. A person feels chills, the functions of internal organs are inhibited, coordination of movements is impaired, and perception is distorted. - Lack of food.
Lack of nutrients creates a shortage of energy, which is necessary for the functioning of the brain and other organs. Hallucinosis appears on days 7-9 of fasting, when ketone bodies become the main energy source. The person looks detached, indifferent, and shows no interest in close people or current events. - Lack of air.
Oxygen is essential for normal brain function. When the supply of air stops, brain tissue uses oxygen reserves for 4-5 minutes, after which hypoxic changes gradually increase, and hallucinatory images are formed. The reasons for the lack of oxygen are intentional suffocation, being in an unventilated room, and ischemic brain damage. - Extreme fatigue.
Prolonged physical and mental overload can cause hallucinatory experiences. Distortion of perception occurs as a result of exhaustion of the nervous system, or more precisely, a violation of its selective function, the ability to distinguish the real from the imaginary. - Sleep deprivation.
Lack of sleep can be the result of insomnia, serious illness, forced wakefulness due to overload at work. Sometimes a state of sleep deprivation is created purposefully to achieve altered consciousness. Regardless of the cause, a person experiences vivid hallucinations, heightened perception of the senses, and a feeling of the unreality of what is happening. - Sensory deficiency.
The nervous system functions normally under constant exposure to a variety of stimuli. If the volume of incoming sensory information decreases significantly or its arrival stops altogether, the brain compensates for this by creating its own stimuli - images of various modalities. Astronauts experience similar conditions. For therapeutic purposes, sensory deprivation chambers are used to stimulate the creativity and deep emotions of patients. - Social isolation.
A decrease or lack of opportunity to interact with other people provokes a loss of personal identity. A person ceases to understand who he is and what he is like, and feels the loss of himself as a representative of society. Hallucination becomes a defense mechanism that helps maintain mental balance and self-identity. Often it is represented by the voice of a “friend”, the image of one of the relatives. The causes of social deprivation are confinement in solitary confinement and serious illness.
Mental disorders
In psychiatric practice, hallucinations often manifest themselves as part of the hallucinatory-delusional syndrome. They are characteristic of psychoses - disorders accompanied by emotional and behavioral inadequacy, lack of a critical attitude towards oneself. As a rule, patients develop pseudohallucinations - visual, auditory, olfactory, gustatory, kinesthetic images that are formed without reference to real space, often accompanied by a feeling of imposition, suggestion by someone else. Causes of hallucinatory-delusional phenomena:
- Schizophrenia.
In schizophrenia, the development of hallucinations is classified as a first-rank symptom. Patients hear the sound of their own thoughts, contradictory, mutually exclusive and commentary voices. Somatic pseudoperceptions (movement, deformation of organs) are noted. Patients are confident that their ideas, feelings and impulses are being influenced, that their thoughts can be read and recognized by others. - Bipolar disorder.
Symptoms of psychosis are observed in severe bipolar affective disorder. A common psychotic manifestation is auditory and visual hallucinations. More often they unfold in a manic phase along with delusional ideas of greatness and omnipotence. The hallucination can be congruent or incongruent with the patient’s mood, supports manic tendencies or is not associated with them. - Symptomatic psychoses.
The causes of exogenous psychotic states are severe somatic diseases, infections, poisoning. They occur with temporary confusion of consciousness, from twilight to oneiroid. Acute psychosis usually lasts from several hours to 2-3 days, delirium with hallucinations often develops at night, and the emerging images frighten patients. In severe cases, delirium turns into amentia, in which confusion, incoherent speech, and chaotic movements predominate. - Organic delusional disorder.
In schizophrenia-like disorder, hallucinatory-delusional attacks are possible, accompanied by unmotivated actions, loss of control over behavior, and manifestations of aggression. Hallucinations are often visual, have religious, magical content, and call for action. The causes of organic delusional disorder are epilepsy, focal brain damage, and surfactant poisoning. - Organic hallucinosis.
A distinctive feature of organic hallucinosis is continuous hallucination caused by the influence of an organic factor. The images are stable and appear with clear consciousness, during periods of wakefulness. The most common is alcoholic hallucinosis, in which patients hear pointing or threatening voices.
Neurological diseases
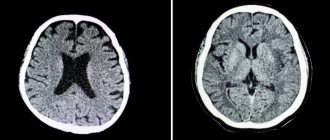
Another reason for hallucinatory images is organic damage to the parts of the brain responsible for processing perceived information. Pathological irritation of the cortical parts of the analyzer occurs, patients begin to see flashes, simple luminous objects, hear music, smell, taste in the mouth in the absence of real stimuli. Another neurological cause of hallucinations is the loss of the analyzer or its functions. Common factors in the development of hallucinatory symptoms in neurological pathologies include:
- Neurodegenerative processes.
Degeneration of nervous tissue leads to the development of dementia, a chronic progressive disease characterized by impairment of higher cortical functions, including memory, speech, and intelligence. Hallucinations are not a necessary symptom. Most often they are diagnosed in dementia with Lewy bodies, less often in Alzheimer's disease and Huntington's chorea. - Local brain lesions.
Hallucinatory visions and sensations are provoked by focal damage to the temporal, occipital or parietal lobes of the brain, hyperstimulation of the midbrain or brainstem. The immediate causes are tumors, strokes, vascular malformations, traumatic brain injuries, focal variants of epilepsy. True elementary and simple hallucinations are typical: flashes, noises, tactile sensations. - Neuroinfections.
In neuroinfections, the pathogen penetrates the tissue of nerve cells, causing both general somatic symptoms and damage to the central nervous system. Convulsions, disturbances of consciousness, a state of overexcitation, delusional-hallucinatory syndrome can occur during the acute course of purulent encephalitis and meningitis. - Loss of analyzer function.
When the analyzer loses the ability to receive external information, a state of forced sensory deprivation is formed. The hallucinatory sensation develops according to compensatory mechanisms, recreating images of a certain modality. A well-known example is Charles Bonnet syndrome - the vision of images in patients with acquired severe visual impairment. - Narcolepsy.
Patients with narcolepsy for no reason experience intermittent drowsiness and attacks of decreased muscle tone while maintaining consciousness. When falling asleep, hypnagogic hallucinations unfold, which prevent you from falling asleep completely, and when you wake up, hypnopompic hallucinations unfold, preventing you from correctly assessing the situation around you.
Substance use
Hallucinations can be provoked by taking drugs, alcohol, or certain medications. Following the use of a psychoactive substance, acute intoxication develops, accompanied by a disorder of consciousness, cognitive functions, perception, and emotions. The severity of psychotic symptoms depends on the type and dose of the psychoactive substance. A mental disorder is characterized by vivid hallucinatory images, false recognitions, and delusions of relation. Such conditions are provoked by the use of a number of substances:
- Hallucinogens.
When using psychotomimetics, such as LSD, mescaline, ecstasy, mental and behavioral abnormalities develop. In the acute period of intoxication, uncontrollable laughter, crying, euphoria, depersonalization, and derealization are observed. The hallucinatory experience is usually vivid, dynamic, and multimodal. The tendency to hallucinosis may persist, manifesting itself in the future when taking alcohol or sleeping pills. - Cannabinoids.
Crushed flowers and leaves of hemp, and preparations made from them lead to drug intoxication. Hallucinogenic, stimulating and sedative effects are noted. Hallucinatory visions are the result of acute intoxication, the simultaneous use of high doses of a substance. Speech becomes slurred, complex motor functions are impaired, and coordination deteriorates. - Amphetamines.
These synthetic substances cause mental arousal, a feeling of well-being, and emotional closeness to other people. The administration of large doses provokes the development of panic attacks, hallucinosis, and paranoia. Hot temper, impulsiveness, and aggressiveness worsen without any reason. Long-term drug use increases the risk of amphetamine psychosis, which is symptomatically similar to schizophrenia. - Substance abuse.
The group of toxic substances includes paint solvents, adhesives, and varnishes. Intoxication is accompanied by a loss of the ability to critically assess what is happening. Hallucinatory sounds and visions, confusion, and vomiting may occur. When substances are removed from the body, the headache intensifies and weakness appears.
Examination and treatment of patients is carried out under the guidance of a psychiatrist
Visual hallucinations in schizophrenia
Visual hallucinations can be represented by photopsies: stars, lights, sparks, smoke, flames, etc. This occurs both in healthy people, for example, with neuroses, overwork, or at the moment of falling asleep and waking up, and in patients with exogenous psychoses (for example, poisoning).
Visual pseudohallucinations in schizophrenia are most often fantastic or fictitious in nature and fit into the general structure of delusion. They are often associated with rituals, magic, and possession by a powerful spirit. The images are complex, elaborate and often hostile.
Visual hallucinations may accompany the paranoid type of schizophrenia. Cosmic vivid images of unusual structure and content are found in patients with a catatonic form of schizophrenia during the period of psychosis.
Most often, hebephrenic and catatonic types of schizophrenia begin in childhood.
Other types of hallucinations in schizophrenia
Olfactory hallucinations in schizophrenia are less common than others and are represented by any unpleasant or unusual odors. Often such patients refuse to eat, believing that poison was added to their food or that the environment smells of “rot or corpses.”
Tactile hallucinations are felt as “worms crawling inside the skin,” “burning from a fire,” a sensation of grasping and other unusual manifestations.
Visceral and muscular hallucinations manifest themselves in the form of the detection of “microcomputers inside the body” that “examine all the insides of the patient,” the connection of various external devices, “exposure to rays” and other supernatural things.
Hallucinations in schizophrenia, no matter how they manifest themselves, are always associated with the patient’s main delusional ideas and have an obsessive nature that worries the patient.
Diagnostics
The subjective nature of experiences with perceptual disorders complicates the diagnostic process. Pathopsychological assessment of patients' condition is based on the clinical experience of a psychiatrist. The assumption of the presence of hallucinations is possible by observing the patient’s behavior and analyzing the general picture of the disease (anamnestic, follow-up information). The standard diagnostic process includes three procedures:
- Clinical survey.
The peculiarity of hallucinations is that they are perceived by patients as part of reality; a critical attitude is possible only in rare cases. Therefore, direct questions about the symptom are ineffective. Hallucinatory-delusional syndrome is identified in the process of communicating with patients, when they begin to talk about implausible or implausible events - “exposure to waves”, “mind reading”, “suggestion with a glance”. The doctor receives more objective clinical information from family members. - Observation.
The behavior and emotional state of the patient reflect the content and nature of hallucinations. He can peer into the space in front of him, at an empty wall, while experiencing fear, surprise, joy. With auditory hallucinations, patients often listen to voices and sounds; they can engage in dialogue, swear, laugh, or joke. Tactile sensations make them scratch, rub their skin, ask a doctor to examine them, and remove “insects.” - Provocative tests.
There are a number of tests to identify hidden perceptual disorders and predisposition to them. When performing the Aschaffenburg test, the patient is asked to talk on a switched off phone; if a conversation is started or the patient hears something, the presence of hallucinations of the auditory modality is assumed. To detect visual hallucinations, the Reichardt test (looking at a blank sheet of paper) and the Lipman test with pressure on the eyelids are used.
Treatment
To eliminate hallucinations caused by taking psychoactive drugs, it is often enough to stop using drugs. If vital substances and conditions are deprived, return them to their previous level: normalize body temperature, restore proper nutrition, sleep and rest, resume social contacts. Hallucinatory symptoms in mental and neurological diseases are relieved with the help of antipsychotics. They reduce mental and motor arousal and prevent the formation of productive psychotic symptoms.