What is cerebral edema
Physiologically, the maintenance of intracranial pressure is ensured by a constant volume of blood and cerebrospinal fluid. Changes in atmospheric pressure, compensation for different volumes of circulating blood are compensated by the inflow or outflow of cerebrospinal fluid. The appearance of additional formation inside the brain, hematoma, inflammatory processes, traumatic brain injury (TBI) leads to compression of cerebral structures. An increase in intracranial hypertension causes the death of parenchyma. Features of symptoms depend on the strength and location of the pathological focus.
Pathological cerebral edema leads to an increase in the size of brain tissue through excess accumulation of fluid. An increase in the amount of water is accompanied by death (if prompt decompression is not carried out in a timely manner). A gradual increase in the volume of brain tissue initially leads to neurological disorders. Psychoses and disturbances in the functioning of internal organs gradually develop.
Classification
Brain edema occurs due to increased cerebral fluid content. In the pathogenesis of edema development, three forms are conventionally divided: cytotoxic, vasogenic and interstitial, or a combination thereof.
Vasogenic edema
Vasogenic edema is the most common form caused by disruption of the blood-brain barrier. Plasma proteins penetrate beyond the blood vessels, causing osmotic pressure to force fluid into the interstitial space of the brain. For example, endothelial growth factor, glutamate and leukotrienes locally increase the permeability of cells around the tumor. It is this, along with the weakness of the vascular walls, that leads to the entry of fluid with proteins into the parenchyma of the white matter. Swelling near tumors in 65% leads to cognitive impairment in patients due to displacement of brain structures.
Vasogenic edema is provoked by impaired vascular permeability and changes in perfusion pressure against the background of the following diseases and conditions:
- brain abscess;
- stroke;
- hypercapnia;
- encephalopathy due to hypertension;
- hepatic encephalopathy;
- metabolic disorders;
- diabetic ketoacidosis;
- lead poisoning;
- mountain sickness
Pathogenic microorganisms in meningitis disrupt the permeability of the blood-brain barrier to proteins and sodium ions. This leads to the accumulation of fluid in the intercellular space, as well as cell swelling due to passive hypoxia. Increased intracranial pressure disrupts connections between neurons.
Cytotoxic edema
Cellular or cytotoxic edema occurs within cells without damage to the blood-brain barrier. Pathology develops after a stroke or traumatic brain injury with damage to glial tissue, neurons and endothelial cells. The hemostatic mechanism in the cells is disrupted, and sodium accumulates in them, and the release of ions outside the membrane is disrupted. Anions try to restore neutrality on the surface of the membrane, which leads to swelling inside the cell.
Cytotoxic is associated with a change in the ion balance on the surface of cell membranes as a result of several reasons:
- hypoxic ischemic brain injury (drowning, cardiac arrest);
- brain injury;
- metabolic disorders of organic acid metabolism;
- hepatic encephalopathy;
- Reye's syndrome (acute liver failure);
- infections (encephalitis and meningitis);
- diabetic ketoacidosis;
- intoxication (aspirin, ethylene glycol, methanol);
- hyponatremia, or excess water intake without electrolytes.
Interstitial edema
One of the main causes of interstitial edema is obstructive hydrocephalus. Interstitial edema develops due to the leakage of cerebrospinal fluid from the ventricles of the brain into the interstitial space of the brain. Patients with hydrocephalus or meningitis are predisposed to this pathology. Increased pressure in the ventricles causes the contents of the ventricles to be forced out, resulting in swelling of the white matter.
Classification of cerebral edema according to ICD 10
Clinical gradation of cerebral edema according to pathogenesis:
- Filtration;
- Interstitial;
- Cytotoxic;
- Vasogenic.
Depending on the location of fluid accumulation, symptoms are distinguished. Vasogenic lesions lead to disruption of the heart, vision pathology, and kidneys. Any organs that have an intensive blood supply are damaged.
The interstitial variety is characterized by compression of most structures of the central nervous system. The intervening fluid initially does not lead to tissue death, since it occupies free space. Lack of nutrients and oxygen leads to cell death. The speed of onset of the effect is determined by the degree of compression.
Classification of intracerebral edema by etiological factors:
- Postoperative;
- Traumatic;
- Malignant (tumor);
- Hypertensive;
- Ischemic;
- Inflammatory;
- Intoxicating.
Standardization of the disease according to ICD 10 allows you to correctly determine the nosological form:
- Nervous diseases – “G0-99”;
- Other nervous system disorders – “G90-99”;
- Various brain injuries – “G93”;
- Cerebral edema – “G93.6”;
- Unclassified cerebral edema – “R60”;
- Localized – “R60.0”;
- Generalized – “R60.1”;
- Unspecified - "R60.9".
Perifocal vasogenic appearance occurs due to increased permeability of the vascular wall. The penetration of blood through the wall leads to the destruction of the blood-brain barrier. The perifocal form occurs at the site of surgery, around the tumor, near the inflammatory focus.
The intoxicating cytotoxic variant develops mainly in the white matter during poisoning with carbon monoxide, cyanides, ischemic conditions, and viral infections. Viral infections provoke cytotoxic changes gradually, leading to the destruction of neurons.
The osmotic variety is formed when the osmolarity of tissues changes. Destruction of the blood-brain barrier is formed during hypoxia during childbirth, sweating through the destroyed walls of the cerebrospinal fluid. The condition is provoked by metabolic encephalopathies (for example, in diabetes mellitus).
Pathogenesis
Brain swelling is a stepwise process in which acute injury results in the formation of cytotoxic, ionic, or vasogenic edema. What is edema? This is a combination of pathogenetic mechanisms. Cytotoxic edema is characterized by depletion of intracellular adenosine triphosphate (ATP), which impairs the active transport of osmolytes across cell membranes. Sodium and water ions accumulate in cells.
On the surface of cell membranes, the pressure and ratio of ions are disrupted, which leads to the movement of fluid into the extracellular space of the brain parenchyma from the vessels. This mechanism is also called ionic. During brain contusions, the activity of the Sur1-Trpm4 ion channel in endothelial cells increases, which leads to fluid accumulation.
A separate form of cytotoxic edema is vasogenic. The pathology develops due to increased permeability of the blood-brain barrier of the brain after a bruise, the release of inflammatory substances during infection and an increase in free radicals. As a result, fluid is released outside the cell along with blood plasma proteins.
As brain contusion develops, these mechanisms replace and complement each other, leading to swelling. It is believed that edema is preceded by an increase in intracranial pressure due to the fixed volume of the closed cranial cavity. At the same time, capillary perfusion - blood pressure in the vessels of the brain - decreases. The tissues do not receive enough nutrients and oxygen, and hypoxemia develops.
Causes of cerebral edema
If a person’s brain swells, the etiology of the disease is first established. Main causes of the disease:
- Hemorrhage inside the skull during hypertensive crisis;
- Traumatic brain injury after a fall, traffic accident, blow from above;
- Malformations of the central nervous system in newborns;
- Inflammatory diseases - toxoplasmosis, meningitis, encephalitis, purulent limited destructive cavities (abscess);
- Change in atmospheric pressure (stay above sea level over one and a half kilometers);
- Carbon monoxide poisoning;
- Birth injury;
- Ischemic or hemorrhagic stroke.
Other etiological factors are less common, but are characterized by similar pathogenetic mechanisms.
Features of cerebral edema in newborns
The structure of the brain of a newborn and infant differs from the structure of the skull of an adult. The baby has instability of anatomical structures. Mechanisms for compensating for increased intracranial pressure have not been developed; there is no redistribution of cerebrospinal fluid and blood to level out hypertension. An increase in fluid inside the skull in an infant is accompanied by acute symptoms. An increase in intracranial hypertension leads to bulging of the cartilaginous tissue of the fontanelles and soft bones.
Immediately after birth, it is necessary to exclude risk factors in children to prevent nosology. Diseases can be identified after the first signs appear:
- Muscle cramps;
- Drowsiness and inhibition of brain activity;
- Restless behavior;
- Bulging of the fontanelle when the child is resting;
- Difficulty feeding from the breast;
- Frequent gag reflex.
Early detection is necessary, since late verification of cerebral edema in a child often ends in death.
Features of intracerebral edema in alcoholism
Metabolites of ethyl alcohol lead to the destruction of the vascular wall, increasing the permeability of the wall. Alcohol abuse in adults provokes chronic vasogenic edema. The condition leads to psychosis (delirium tremens, withdrawal symptoms). The longer the abuse of ethyl alcohol, the more irreversible the changes inside the brain.
All organs react to exo- and endo-harmfulness with a limited number and quality of pathological reactions. For the brain, this means oxygen starvation and a disorder of liquorodynamics, various manifestations of cerebral edema. Spongiosis (spongiosis) of brain tissue, its gray matter, is much less common than white matter. It is believed that this is almost the only morphological sign of a slow viral infection. Moreover, it is the gray matter that K. Taidushek (1989) emphasizes. The basis was the study of kuru and CJD as diseases of humans and animals. It is believed that in the chronic form of Vilyui meningoencephalomyelitis, foci of spongiosis also occur (P.R. Petrov, 1987). In the acute form of this apparently viral genetic disease (only Yakuts get sick), the brain reacts with meningoencephalitis - inflammation. Spongiosis is expressed very modestly (the archive of Academician A.L. Avtsyn, by the way, also K. Taidushek receives this material).
In ICD-9, spongiform, subacute (viral) encephalopathy is coded in two ways: 046.1 and 331.5.
In mental illnesses (schizophrenia, senile cerebral amyloidosis, vascular encephalopathy), the phenomenon of spongiosis in the gray matter is observed rarely, in limited areas. In the white matter of the marginal layer of the cortex and subependymal spongiosis (cribrosity - fr.
sieve, honeycombing) is an obligate phenomenon. Moreover, it was intravital, which was established by CT and NMR tomography and then verified by us posthumously. This method of studying a living brain sometimes also reveals in subcortical formations what tomographers call leukoaraiosis (white discharge of X-ray and resonance density). Moreover, sometimes errors occur when a decrease in the density of brain matter due to the formation of softening cysts (lacunae) is interpreted as leukoaraiosis. Histopathological verification makes it possible to clarify such ideas, rejecting both demyelination and necrosis - we are talking about types of focal cerebral edema (persistent - V. A. Morgunov et al., 1980). This is especially common in interstitial dropsy of the brain, which accompanies amyloidosis and atrophy, as a result of obstacles to liquor dynamics, since senile plaques (balls) develop pericapillary.
Even more often, to one degree or another constantly, one can see spongiosis of the white matter of the brain perivascularly (vasogenically) in the form of cribricity, which in fact, one to one, is equal to sponginess and is characteristic of vasogenic cerebral edema. CT and NMR studies have shown that this is not only focal, but also diffuse cerebral edema (and not fatal if not accompanied by dislocations). Moreover, we were able to observe the disappearance of leukoaraiosis after intensive dehydration therapy. And this is confirmation that the phenomenon is not a destructive process, but a reversible one, which pushes the bundles of myelin fibers apart, compresses them, but does not destroy them. Spongiosis in the white matter of the brain is a microscopic phenomenon (X 100), although the tomogram allows one to see macroscopic lesions (at least 1 x 1.5 cm), although paraventricularly one can see a zone of leukoaraiosis that is thinner than in the subcortical formations.
Belgian ultramicroscopists (J. Flaman-Duran et al., 1979) also started talking about spongiosis at the EM level. However, one must remember the difficulties of comparing biopsy and post-mortem material, especially after perfusion of the animal brain. So far we have not touched on the possible interpretation of “polyospongiosis”, its morphogenesis, as a result of virogenic lysis of cortical neurons. B. M. Zhdanov (1990) directly indicated that virogenic lysis occurs where virions multiply. A.F. Bykovsky (1973) believed that the reproduction of viruses in a cell entails its death. The cytopathic pathology on which these conclusions are based is based on the study of the cytology of cells in culture. We are trying to compare cultural data with those known from the histopathology of the human brain, when the virus is integrated into the genome and does not replicate at all. In this situation, the death of neurons or gliocytes is possible and does not occur en masse, except for shadow cells.
Here a very common phenomenon comes to mind - the so-called pericellular edema (general pathologist, academician A.M. Wichert chuckled at neuromorphologists: - They still have perivascular and pericellular edema; yes, that’s right - cerebral edema is a constant phenomenon and an artifact you can't name him). Only the degree of expression varies, even after perfusion of the animals' brains. Still, with paraffin embedding, there is some doubt about pericellular edema. It’s easier with myelin, which is hydrophobic and therefore the cerebrospinal fluid is more spatially outlined here, in particular in “drainage” oligodendrogliocytes (P.E. Snesarev), this is interfascicular glia. To avoid the reproach of artificiality, it is necessary to gradually dehydrate and delipidate the pieces of the brain until the alcohols of the wire are completely transparent from the turbidity with distilled water (emulsion test). Since even tiny pieces for EM are capable of leaving ultrastructural traces of the presence of interstitial cerebrospinal fluid, it should be recognized that brain fluids are not only structured (astrocyte processes, surrounding neurons and capillaries) with proteins, but are also “free” between brain lipids, which are also prevalent in myeloarchitecture both cortex and white matter.
And yet, it is not possible to trace the lysis of a neuron that has become hyperchromic in the pericellular vacuole. Thus, the state of neurons in pericillary vacuoles is opposite to what we saw during karyocytolysis and shadow cell formation. One argument is quite important: in acute toxic encephalopathy (and hyperthermia) in fatal schizophrenia, a pattern of cytocidal neuronal lysis is observed.
It is unproven to regard cortical lesions of spongiosis as a result of neuronal death. This is a manifestation of liquor stasis, edema, and not a softening cyst (L. I. Smirnov, 1949). With them, accumulations of pigments of hematogenous origin (blue, green, brown) are observed, but the main thing is that the cavity is delimited by the proliferation of glial fibers and connective tissue. As ephemeral as the histopathology of spongy encephalopathy is, the picture of encephalitis is so self-evident (however, not always). Their classification is based on extensive experience in clinical and anatomical comparisons and belongs mainly to neurologists. But psychiatrists also put their fundamental experience in the study of progressive paralysis into this “library”. Using this example of cerebral syphilis, one can understand the spread of serous encephalitis throughout the cortex, which has no equal in severity; only purulent meningoencephalitis is accompanied by the same violent reaction. Thanks to antibiotics, P/P has become a rarity, but, presumably, only temporary - a new outbreak of untreated (or untreated) syphilis is coming. The disappearance of Economo's encephalitis is more difficult to understand. Or the absence of a pronounced inflammatory reaction during parainfluenza (A.P. Avtsyn, personal communication).
In those cases when, unexpectedly for psychiatrists, diffuse, serous polyencephalitis is histologically detected, then all paths of immunological identification are cut off and, as a rule, the etiology remains only the subject of a search in literary sources. The second scourge - identification of the nature of even clinically obvious encephalitis - is a late autopsy, which also cuts off the possibilities of immunomorphology. Immunopathology in vivo is also not always indicative, since the presence of AT to a number of viral Ags in mentally ill patients is just a background and the “population” of the brain with a number of persistent viruses (measles, herpes, cytomegalovirus, rubella, etc.). From our point of view, the most important thing is that latent viral infection of the human brain has no morphology, or it is non-inflammatory, immunodeficiency. This applies to virulent viruses, but as for “non-infectious” ones, this is completely surprising. For example, an epileptogenic focus, where perivascular lymphoid couplings are sometimes found (V. A. Klein, 1983). Usually, no inflammatory phenomena, either histologically or especially EM, are noted here.
Lastly, viral inclusions (nuclear and cytoplasmic). EM did not add very much to this (we are talking about cadaveric material, where time is a decisive factor in such research). The main achievements in the ultrastructure of viruses were obtained at the cultural level, which is perceived with distrust in postmortem material of the human brain. The “intactness” (histological) of the brain in mental illnesses (so-called “functional” psychoses) is, of course, a very convenient myth for psychiatrists. In modern times, this is the result of a complete lack of fundamentals of neuromorphological education. Brain structures are a refuge not only and not so much for the well-known virulent viruses (let’s add neurotropic ones), but also psychotropic ones that have so far escaped identification. The role of endogenous viruses responsible for the etiology of psychovirological diseases has been proposed, clearly by analogy, to be the same retroviruses that play a major role in oncogenesis and neuro-oncology, in particular, also in AIDS, which has already been instrumentally proven. Moreover, with it there is no (according to the descriptions of microgliosis) real encephalitis, but there is also no spongiosis. Our own, very limited, experience in studying encephalitis has shown that spongiosis is not an obligate manifestation of viral encephalitis. Conversely, foci of polyospongiosis in the cerebral cortex of the deceased do not provide any basis for the diagnosis of encephalitis. As for leukospongiosis, this picture is so common that it should without hesitation be attributed to a violation of liquor dynamics.
Let us conclude the problem of the influence of viruses on the cell with reference to S. Luria et al. (1970). The authors identify 3 types of effects exerted by animal viruses on host cells (p. 279): 1. Destructive, cytolytic, occurring after many morphological changes; 2. Transformation of a cell infected with a virus, which occurs as a result of integration of the virus by the cell; 3. The inductive effect of the virus on the cell, with the formation in the infected cell of substances determined not by the virus, but by the altered cellular genome. It is this third option that we believe refers to the genome containing endogenous viruses. The authors present a table - “Typical cytotoxic changes in cells infected with animal viruses.” Here, nuclear pyknosis comes first, then the appearance of eosinophilic substances in the cytoplasm, destructive changes in cells, fusion of cell nuclei with the appearance of giant and multinucleated cells (see inset). We had to observe megakaryocytes in the spleen in Werlhof's disease, a disease of completely unclear origin. In addition to the brain of an oligophrenic (P.B. Kazakova), such multinucleated cells were observed in the brain of a necrotic lesion in herpes encephalitis. While pyknosis of the nuclei and cytoplasm of pyramidal neurons of the cortex is an ordinary phenomenon to a greater or lesser extent. Such cells are called “sclerosis” or hyperchromatosis, as well as neuronal shrinkage. This phenomenon was continuous in the cerebral cortex during the death of young people with schizophrenia and dying from tuberculosis. But now, in gerontopsychiatric material, they are found scatteredly and with... pericellular edema, which is often attributed to a filling artifact. Ultrastructure has answered this riddle - such cells are surrounded by swollen electronically empty processes of astrocytes. But there were so many opinions about the genesis of the wrinkled neuron!
The pathological anatomy of encephalopathies is full of mysteries of its genesis. When the nature of the “pathy” is revealed, it becomes obvious that sometimes we are talking about viruses (epileptogenic focus) or another genetic cause.
Pathogenesis of cerebral edema
The initial stage of the pathology is accompanied by impaired microcirculation. Perifocal changes are located near the tumor, inflammatory focus, at the site of bone-destructive injuries to the skull.
A consistent increase in changes, the accumulation of copious amounts of fluid is accompanied by a disorder of vascular regulation, an increase in the size of the cerebral arteries, and subsequent intracranial hypertension.
Swelling of brain tissue, generalized swelling is characterized by circulatory and vascular edema. Multiple injuries cause massive death of neurons. The fluid squeezes out intracerebral structures, and the disposition of anatomical formations is formed. The situation increases the risk of death due to the likelihood of the brain being wedged into the foramen magnum. Death occurs due to damage to the center of thermoregulation, respiration, and cardiovascular activity.
Treatment
Brain swelling is treated in two ways: non-surgical and surgical. Non-surgical methods include the introduction of a large dosage of drugs that remove fluid from the body: hormonal drugs improve the functioning of the system, limiting the entry of certain substances into the tissue, and reduce the permeability of brain vessels. Anticonvulsants are prescribed only when seizures occur. Surgical methods include opening the cranial cavity to create a defect in the skull bones, which quickly reduces intracranial pressure.
Treatment of the disease that caused cerebral edema:
- cerebrovascular accident - correction of blood pressure, drugs are prescribed that nourish the brain and improve blood flow;
- TBI – destroyed brain tissue and blood accumulations are removed; poisoning – toxin is removed from the blood; brain tumors – excision of the tumor; acute infectious diseases - taking antiviral drugs.
- treatment is always aimed at restoring normal oxygen metabolism in brain cells through a combination of surgical and medicinal methods. This improves the ability to remove swelling. Of course, the faster and more quickly the therapy was carried out, the less time it will take to restore the body, and it is possible to avoid serious consequences.
You can book your prescribed medications on our portal. The site interface is easy to use - minimum time and maximum pleasure with DOC.ua
Complications
Complications and consequences of this type of disease can be dislocation syndrome, in which part of the brain is limited inside the cranial cavity by relatively immobile structures, which leads to a complete lack of consciousness, disturbances in breathing rhythm, and a drop in blood pressure. Possible death. Brain edema in newborns and other patients cannot be predicted in any way, and there is no prevention for it, because the disease develops secondary, against the background of the underlying disease. It is known that in the presence of pathologies that can lead to cerebral edema, furosemide or magnesium sulfate is prescribed. These medications prevent the accumulation of excess fluid in the brain tissue.
The first signs of cerebral edema
Symptoms are determined by general and local disorders. It is impossible to determine what is primary, therefore an analysis of the initial signs of pathology is required:
- Severe pain or increasing chronic pain in the head;
- Cloudiness of consciousness;
- Fainting;
- Meningeal syndromes are disorders of conscious activity;
- Paresis and paralysis of half the body;
- Visual pathology;
- Coordination disorders;
- Reduced blood pressure;
- Constant muscle contractions (convulsive);
- Strabismus.
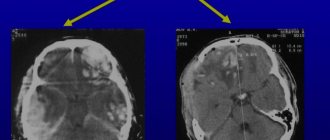
Mortality due to intracerebral edema is often observed, so it is important to identify at least one sign to prescribe additional diagnostic methods - neuroimaging (MRI and SCT of the head).
Consequences of cerebral edema
Dangerous complications of pathology are determined by a number of pathogenetic changes:
- An increase in the amount of fluid with an increase in the degree of compression of the cerebral parenchyma, the disposition of brain tissue. Mortality occurs when available space for water storage runs out;
- Early detection, drug elimination of the pathology with subsequent resorption of free fluid is a favorable prognosis. Timely delivery of people to the intensive care unit or toxicology department allows to remove toxins and eliminate other etiological factors;
- Removal of edema after disability occurs. Meningitis, meningoencephalitis due to traumatic brain injury lead to irreversible neurological disorders.
Even after timely surgery, complete relief from the consequences of the disease cannot be guaranteed.
Neurogenic consequences of cerebral edema:
- Memory disorders;
- Strabismus divergent;
- Severe headaches;
- Motor disorders;
- Depressive state;
- Epileptic seizures;
- Pathology of speech and attention;
- Facial asymmetry.
The consequence of the condition can be constant anxiety and chronic fatigue.
Diagnostics
To make a diagnosis, the doctor examines an analysis of the patient’s complaints and medical history. Finds out how long ago headaches, drowsiness and weakness began, whether there could be a head injury, poisoning, or whether there is a neurological pathology. A neurological examination is performed to determine the level of consciousness, and a search is made for signs of weakness in the limbs, strabismus, or facial asymmetry. A fundus examination is performed. Cerebral edema is characterized by swelling of the optic disc with unclear boundaries. Intracranial pressure is measured and a lumbar puncture of the spinal cord is performed. With swelling and pressure, cerebrospinal fluid flows out, and sometimes spurts out of the hole in the back. To view the structure of the brain layer by layer and identify signs of disease, an MRI of the brain is performed. A consultation with a neurosurgeon is possible.