When Lina watched Kantemir Balagov’s film “Dylda,” where the main character Iya suddenly froze, having lost touch with the world, the girl experienced catharsis. For the first time in her life, she saw a person with the same strange behavior as her. But Iya was shell-shocked in the war, and, apparently, the cause of the heroine’s stupor was a head injury. And Lina didn’t know why sometimes her brain seemed to be disconnected from the network.
“Have you seen people pretending to be statues for money? “I could easily make money like that,” Lina jokes. —
But they probably don’t feel pain, but I feel it every time I freeze. At these moments, my body seems to be paralyzed by a spasm, and I can’t do anything about it. It’s as if a person is under anesthesia, but still feels like his stomach is being ripped open.”
The girl cannot guess at what moment her body will stop functioning again, and the real world will collapse into one point. Lina laid carpets in the apartment and wrapped all the sharp corners of the furniture in case of a fall (although this never happened in two years).
Freezing is only one of the signs of catatonic syndrome. Sometimes a person becomes flexible and soft, like wax, and he can be given a certain position in which he “freezes” for a long time, like a mannequin. Symptoms of catatonia also include a complete lack of speech (mutism), involuntary duplication of the words of others (echolalia), repeated aimless actions (stereotypes), resistance to attempts to move the person (negativism), and maintenance of an uncomfortable position (catalepsy).
What is catatonia
Catatonia, or catatonic syndrome, is a condition in which a person becomes unresponsive to external stimuli and loses the ability to move and speak normally.
Until the beginning of the 20th century, it was believed that this only happened in schizophrenia. But then scientists found out Catatonia: pathophysiology, diagnosis and modern approaches to treatment that more than 50% of cases of catatonia appear in bipolar disorder, about 10–15% occur in schizophrenia, and 21% are not associated with mental illness at all.
Catatonia is similar Catatonia is the evolution of views and modern ideas (literature review) on mental disorders and other diseases, so it is difficult to recognize. For example, with it, as with a stroke, a person may respond with incomprehensible phrases or stop talking altogether. Urgent help is needed in both cases, but it will be different.
Catatonia can develop rapidly or gradually over several days. In the first case, the symptoms are usually strong and obvious; pressure or temperature surges are added to motor and speech disorders. This can lead, for example, to a stroke. In the second option, the symptoms are barely noticeable, and this is the most dangerous: in 3–4 days complications may appear: Catatonia or the person will die.
Imagine a grandmother who suffers from dementia. She often sits on the edge of the bed and looks out the window. But suddenly she spends the whole day like this. Then the grandmother stops talking and reacting to others, but continues to sit. Then she refuses food and water.
The body is exhausted, and 2-3 days after the first symptoms appear, blood clots form in the legs from a long immobile position. At some point they break off and clog the vessel. The man dies. But they would have been able to save him if dangerous symptoms had been noticed on the first day.
History of disease research
Since its initial description, catatonia has remained a poorly defined clinical condition characterized by impaired motor behavior originally described in the presence of another severe mental illness. It is a complex syndrome that has undergone significant evolution since it was originally described as a subtype of schizophrenia. The condition is now thought to result from a variety of medical and psychiatric conditions and may be more related to mood disorders than schizophrenia.
It is noted that one of the main reasons for the frequent misdiagnosis of catatonia is the persistent misconception that it is synonymous with schizophrenia. However, this proposal was not universally accepted, and much debate arose regarding the most appropriate classification of catatonia.
It was Carl Ludwig Kahlbaum who first saw the connection between psychomotor symptoms and mental disorders in 1874. And this year he coined the term “Die Katatonie” to describe the syndrome “with a cyclical alternating course in which the mental symptoms are successively the following: melancholy, mania, stupor, confusion and, ultimately, dementia.”
He also combined 17 movement disorders into a single syndrome in patients with a variety of disorders, including mood disorders, psychosis, neurosyphilis, tuberculosis and epilepsy.
In 1899, Emil Kraepelin proposed that catatonia should be classified phenomenologically along with other forms of dementia precoxa or dementia precoxa (the obsolete name for schizophrenia): hebephrenia and paranoia. And by 1913, catatonia had become “1 of 8 subgroups into which schizophrenia was divided.
Thus, in the works of Kraepelin and Bleuler, catatonia became synonymous with behavioral immobility and abstinence, a symptom often associated with schizophrenia, and was subsequently classified as schizophrenia, although not all authors of that time shared this point of view.
This has led to ongoing controversy in the Diagnostic and Statistical Manual of Mental Disorders (DSM). Thus, in the DSM-I and DSM-II and in the International Classification of Diseases (ICD), catatonia was classified as a type of schizophrenia, and this assumption was formalized throughout the life of the DSM-III classifier.
This began to change in the 1970s, when researchers noticed that catatonia was more closely associated with mood disorders and idiopathic or primary disorders than with schizophrenia.
For example, Fink and Taylor argued that catatonia should not be associated exclusively with schizophrenia. This led to the 1994 DSM-IV recognizing catatonia as a disorder that could either complicate general health or be a feature of mood disorders. At the same time, debate continued to support catatonia as a separate diagnostic category.
The development of rating scales and more effective screening procedures led to the discovery that 9% to 17% of patients in psychiatric institutions and emergency departments met criteria for catatonia—even more among patients with mood disorders or toxic conditions than among patients with schizophrenia.
It has also more recently been suggested that catatonia is relatively common among patients diagnosed with autism, particularly in autistic children.
In addition, there is increasing recognition of “secondary” catatonia, which develops due to organic causes such as neurological diseases (including tumors), drug intoxication or withdrawal, and other metabolic disorders, including paraneoplastic syndromes.
On a larger scale, catatonia has been associated with other neuropsychiatric syndromes such as delirium, serotonin syndrome, and neuroleptic malignant syndrome.
In a review, Wijemann and Jankovic emphasized 2 subtypes of this disorder: malignant and periodic. Malignant catatonia is the most severe form of this syndrome and is more common in the presence of organic disease, illicit or therapeutic drug toxicity, or other metabolic encephalopathy.
Intermittent catatonia is characterized by repeated episodes of illness lasting 4 to 10 days, which can occur over many years. This condition appears to be less common than the malignant form and is reported as an autosomal dominant disorder. Intermittent catatonia is often noted among patients with bipolar disorder, in which the patient oscillates between stupor and agitation.
Why does catatonia occur?
Catatonia was first described in detail in 1874, but its causes have not yet been established. Scientists have several theories about catatonia: pathophysiology, diagnosis and modern approaches to treatment, which approximately explain what changes in the body lead to the appearance of symptoms of catatonia.
Some researchers believe that the problem lies in a disruption in the transmission of nerve impulses in those areas of the brain that are responsible for muscle contractions. Others associate catatonia with a change in the balance of neurotransmitters - substances that are produced by neurons in the brain and are involved in transmitting signals from cell to cell and many biochemical processes. Still others blame the excess or lack of certain hormones of the hypothalamus and pituitary gland, the production of antibodies to brain proteins.
Such disturbances in the functioning of the body appear in many diseases:
- psychiatric Borisova P. O. Nosological dilemma and clinical polymorphism of the phenomenon of catatonia. , for example bipolar disorder, schizophrenia, autism, depression, anorexia nervosa;
- endocrine: Cushing's syndrome, hyperthyroidism, Sheehan's syndrome and others;
- neurological, for example epilepsy, multiple sclerosis, Parkinson's disease, brain tumors, dementia;
- metabolic - this is when substances accumulate in the body that have a bad effect on the brain: this happens with Wilson-Konovalov disease, an increase and decrease in sodium concentration in the blood, kidney failure and other diseases;
- autoimmune, for example systemic lupus erythematosus, antiphospholipid syndrome;
- Catatonia caused by psychoactive substances: alcohol, antipsychotics, sedatives, drugs;
- infectious Catatonia: HIV, typhoid fever, tuberculosis, meningoencephalitis, herpes and others;
- vascular, for example thrombosis of the arteries and veins of the brain, stroke, cerebral hemorrhage.
What are the symptoms of catatonia?
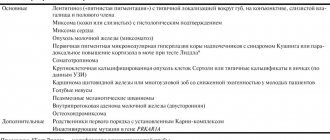
Catatonia has many symptoms. In the DSM-5 reference book, which is used by psychiatrists all over the world, 12 main Catatonia are identified. But doctors add other symptoms to them:
- Remaining motionless (stupor).
- Long-term maintenance of the posture given to the body (catalepsy). If you plant or stand a person, he will not move.
- Prolonged silence (mutism). The person does not respond, even if addressed by name. On the contrary, he will most likely turn away.
- Changing the position of the limbs, like a plasticine figurine (wax flexibility). Some patients easily obey and can follow any command, like robots.
- Passive and strong resistance to any attempts to change the position of the arms and legs (negativism). Sometimes it is physically impossible to bend or straighten the limbs.
- Maintaining an awkward posture (posing). For example, a person can bend over on the bed without touching the pillow with his head, as if hanging in the air.
- Pretentiousness of movements (manneriness). Someone with catatonia may gesticulate strangely and inappropriately.
- Repetitive monotonous movement (stereotypy). Remember how in horror films the possessed constantly sway, tap their fingers, or move their mouths creepily. Most likely they are having an episode of catatonia.
- Excessive arousal without external stimuli. A person can rush around the room, show aggression, and rush at others.
- Involuntary movements of the lips and eyebrows. Grimaces that are not made to amuse others.
- Repeating someone else's words (echolalia). Moreover, speech often becomes incoherent, monotonous, words and phrases are spoken continuously, sometimes for a very long time.
- Copying other people's movements (echopraxia).
Additionally, symptoms may occur Neznanov N. G., Kuznetsov A. V. Clinical and psychopathological aspects of the pathomorphosis of catatonic disorders associated with disruption of the autonomic nervous system. With catatonia, the temperature rises, thirst increases, saliva flows, blood pressure rises and the pulse quickens. Patients often refuse water and food.
When a doctor makes a diagnosis, he looks for a combination of several signs. But medical attention is needed even if one symptom appears. Otherwise, you can miss not only catatonia, but also a stroke, the onset of schizophrenia, a complication of meningitis or another disease.
Symptoms and manifestations of catatonic syndrome
According to the DSM-5, at least three of the twelve symptoms must be present to diagnose catatonia. These include the following signs:
- Catalepsy: passive induction of postures held against gravity.
- Waxy flexibility: characterized by the patient freezing for a long time in the position he has adopted or given to him, even if it is very uncomfortable.
- Stupor: lack of psychomotor activity and reaction to the environment.
- Agitation: does not depend on external stimuli.
- Grimacing: distortion of facial expression.
- Mutism: complete silence of the patient or minimal verbal response.
- Negativism: the patient's resistance or non-response to external stimuli, such as instructions.
- Posturing: spontaneously and actively holding a pose or position that goes against the force of gravity.
- Mannerism: extreme or strange caricatures of various actions and movements, spontaneous movements.
- Stereotypy: frequent, repetitive movements for no reason.
- Echolalia: frequent repetition of other people's words.
- Echopraxia: imitation of other people's movements.
- Proboscis sign: contraction of the muscles around the mouth, which consists of
- the lips are constantly extended forward with the jaws tightly clenched. Characteristic of catatonic stupor with numbness.
- Babinski's sign: extensor reflex of the big toe.
Other common symptoms include rigidity (lack of response or resistance to stimuli) or automatic obedience. If catatonia is associated with schizophrenia, the stupor may continue for a long period of time. This is in contrast to catatonia associated with other psychiatric conditions, where there may be long-term remissions.
How is catatonia treated?
If a person cannot move or does not respond to calls to him, an ambulance must be called. If the symptoms are mild, it is important to go to a therapist as soon as possible.
From the words of relatives or by analyzing a medical record, the doctor will determine whether there are mental illnesses, alcohol addiction or other pathologies that can cause catatonia. And if necessary, he will send you to a psychiatrist.
He will prescribe medication or electroconvulsive therapy as quickly as possible.
If there is no danger to the patient’s life, the Catatonia examination will help find the causes of catatonia:
- general blood analysis;
- biochemical research;
- analysis of blood electrolytes;
- liver function tests;
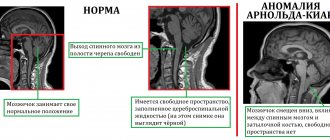
- or MRI of the brain.
An electroencephalogram will be performed if there is a suspicion of a brain tumor or seizures.
What medications are prescribed
To eliminate catatonia, the psychiatrist uses strong prescription medications. Taking them on your own is dangerous.
First of all, they give drugs Catatonia: pathophysiology, diagnosis and modern approaches to treatment from the group of second-generation anxiolytics based on benzodiazepine. They reduce muscle spasms, calm, and help remove the symptoms of catatonia. Benzodiazepines are effective Systematic review of catatonia treatment in 66–100% of patients.
If these drugs do not help, the treatment regimen is changed. Sometimes alternative drugs with sedative, anticonvulsant and muscle relaxant effects provide the best effect. For example, lithium drugs Catatonic syndrome: From detection to therapy will not allow a recurrence of an attack of catatonia.
Medicines from the group of neuroleptics are prescribed Catatonia: pathophysiology, diagnosis and modern approaches to treatment rarely: it is impossible to guess how the patient’s body will react. On the one hand, drugs can relieve muscle spasms. But at the same time, they can cause neuroleptic malignant syndrome. This is a condition when the temperature and blood pressure rise and the symptoms of catatonia intensify.
In what cases is electroconvulsive therapy used?
Electroconvulsive therapy is a treatment that uses electric current through the brain. It suppresses areas that emit abnormal impulses and helps relieve muscle spasms and cramps.
Is electroconvulsive therapy an evidence‑based treatment for catatonia? A systematic review and meta-analysis if benzodiazepines are ineffective or if the patient can Is electroconvulsive therapy an evidence-based treatment for catatonia? A systematic review and meta‑analysis to die.
Sometimes, after using electroconvulsive therapy, attacks of catatonia completely stop. But there is a risk. Is electroconvulsive therapy an evidence‑based treatment for catatonia? A systematic review and meta‑analysis of side effects: headache, amnesia, confusion.
Diagnosis of catatonic syndrome
All patients with suspected catatonia should undergo EEG testing as a screening for other neurological conditions. It tends to exhibit epileptiform activity in nonconvulsive status epilepsy and slowing in cases of encephalopathy.
The EEG in catatonia is usually normal unless there is an underlying condition that may be causing the abnormality.
Given that catatonia can develop in the context of a wide range of neurological conditions, brain imaging, preferably MRI, is recommended. In cases of catatonic stupor, immobility usually allows these tests to be carried out easily.
Laboratory studies should include a complete blood count, blood urea nitrogen, creatinine, muscle and liver enzymes, thyroid function tests, electrolytes, blood glucose, and urinalysis to evaluate associated conditions, causes, or complications of catatonia.
Marked dehydration is not uncommon in catatonic patients and should be addressed.
Vital signs should be assessed frequently because hypertension and fever (often accompanied by elevated creatine phosphokinase, decreased serum iron, and leukocytosis) may herald the occurrence of malignant catatonia or neuroleptic malignant syndrome if the patient has been receiving antipsychotic medications.
Unfortunately, the nature of catatonia makes certain aspects of physical and neurological examination impossible. Components of the neurological examination that can typically be assessed include pupillary response, eye movements, corneal reflex, response to pain, presence of drooling, immediate response to threat, response to light or sound, tendon reflexes, and plantar response.
How successfully is catatonia treated?
The sooner catatonia is treated, the better for the patient. Quick help helps to avoid complications and save life.
But not everyone recovers. According to Catatonia statistics, 12–40% of patients are successfully cured. The prognosis is poor in children and adolescents with schizophrenia, as well as in older adults. They may require Catatonia ongoing psychiatric care.
If a person has long suffered from kidney failure, alcoholism, Parkinson’s disease or other pathology, then the disturbances in brain function are already chronic. Therefore, at any moment, catatonic syndrome can recur. Catatonic syndrome: From detection to therapy. In order not to be late with help, you need to remember the dangerous symptoms and follow the doctor’s recommendations.
How to avoid getting catatonia
Scientists have not yet learned how to prevent catatonia, like other mental illnesses or brain tumors. But, taking into account the causes of the syndrome, we can advise the following:
- Reduce alcohol consumption, and if you have symptoms of addiction, get treatment.
- Never use drugs.
- Don't ignore symptoms of depression.
- Do not take sleeping pills, sedatives, or antipsychotics without a specialist’s prescription. Catatonia: pathophysiology, diagnosis and modern approaches to treatment.
- See a doctor if you have headaches, dizziness, or spots in your eyes.
- Treat kidney and liver diseases in a timely manner.
- Avoid casual sex to protect yourself from HIV and syphilis.
- Monitor your weight and avoid stress so as not to worsen the condition of your blood vessels.
- Pregnant women should register on time and follow the doctor’s recommendations so that the birth goes smoothly.
- Try not to injure your head.