Related news
Clinical recommendations for vaccination of pregnant women against influenza and pneumococcal infection
How to stop pneumococcus? Interview with N. I. Briko
How to prevent pneumococcal infections in adults?
Prevention of pneumococcal infection
Experts advocate for stronger protection against pneumococcus
Alexander Chuchalin: “Vaccine prevention is the optimal strategy to combat pneumonia”
Vaccination of adults against pneumococcal infection: world experience
Additional materials
Seminar: “Pneumococcal infection: status, problems and opportunities for prevention”
Where have all the ear infections gone?
Humanity against pneumococcus - a story of struggle and victories
General information
Worldwide, diseases caused by Streptococcus pneumoniae (S. Pneumoniae or pneumococci) and related to pneumotropic infections represent one of the most serious public health problems.
There are invasive and non-invasive forms of pneumococcal diseases. Invasive pneumococcal infection (IPI) includes a number of severe and life-threatening diseases: bacteremia without a visible focus of infection, meningitis, pneumonia, sepsis, pericarditis, arthritis. Non-invasive forms of pneumococcal infection are bronchitis, community-acquired pneumonia, otitis media, sinusitis, conjunctivitis.
According to statistics, up to 70% of all pneumonias, about 25% of otitis media, 5-15% of purulent meningitis, about 3% of endocarditis are caused by pneumococcus S. Pneumoniae.
Pneumococcal infection is usually a complication of other infections. Examples are pneumococcal pneumonia, inflammation of the middle ear (otitis) in children after or against the background of influenza, or measles, or any other respiratory viral infection.
Pneumococcal disease is spread through respiratory droplets such as coughing (especially through close contact). The source of infection can be a person without any clinical manifestations. Information about seasonality for diseases caused by S. Pneumoniae is quite contradictory. However, a number of authors note an increase in incidence in the autumn-winter period, which is characteristic of a number of other pneumotropic infections.
Children of the first years of life are the main carriers of pneumococci, infecting adults. While the usual carrier frequency in adults is 5–7%, among adults living with children it reaches 30%.
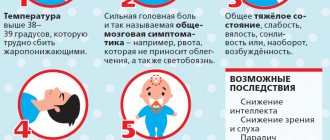
Symptoms of the disease
Signs of the disease are infectious, meningeal and cerebral changes. The main symptoms of the pathology are:
- weakness of the body, lethargy;
- high temperature, which is difficult to relieve with antipyretics;
- complete aversion to food, anorexia, reluctance to drink;
- decreased heart rate, atony, drop or increase in blood pressure;
- the spread of blood poisoning is accompanied by urticaria on the epidermis, regression of the rash occurs at a slow pace;
- bursting pain in the head area;
- localization of pain in the temples and frontal region;
- vomiting not associated with meals, which does not bring relief to the patient;
- protrusion of the network of veins in the eyelids and head;
- impaired awareness, uncontrolled motor activity, followed by complete apathy (possible coma);
- convulsive manifestations, epileptic paroxysms;
- in newborns there is a noticeable divergence of the sutures of the skull, swelling of the fontanel zone, a monotonous, sharp cry;
- oculomotor and respiratory disorders.
A specific symptomatology is the forced position of the patient, attempts to change which are accompanied by involuntary reflexes. The patient is in the fetal position, lying on his side with his head tilted back. Any touch or tactile influence causes unbearable suffering. Even light clothing brings severe discomfort. There is a strong reaction to light. The patient cannot independently straighten the limbs in the joints. If the doctor attempts to bring the head to the chest, the patient unconsciously brings the bent legs to the stomach. The limbs bend synchronously, which does not allow manipulation on only one leg. When palpating the zygomatic area or upper eyelids, severe pain is noted.
Infants have specific symptoms when held in an upright position. The child unconsciously pulls his legs towards the abdomen. There is also a tendency to keep the head thrown back. Total shell signs are rarely observed.
First, the temperature rises sharply, vomiting, and a severe headache. The babies don't stop screaming. Consciousness is in a depressed state on the second or third day after the initial symptoms. Then convulsions and coma appear (3-4 days). If the extent of the edema is significant, displacement of the brain structures may occur with squeezing of the trunk into the foramen magnum. This condition often leads to death.
Infection of brain tissue can be assumed if there is parallel inflammation in other parts of the body. The subacute form manifests itself more quickly, which helps specialists suspect the disease in time and take the necessary measures. Low symptoms are fraught with delayed diagnosis and subsequent critical complications (including death).
Chance of getting sick
The highest incidence of severe pneumococcal infections is recorded in children under 5 years of age and among older people (over 65 years of age). Young children under 2 years of age, whose bodies are unable to resist infection, are especially defenseless against pneumococcus. For this age group, this is the No. 1 infection and the most common cause of severe forms of pneumonia, otitis media, and meningitis. Among the elderly, the most vulnerable are those who are permanently residing in aged care facilities.
In addition, risk groups for the incidence of pneumococcal infection include children and adults with chronic diseases of the cardiovascular, respiratory systems, diabetes mellitus, liver cirrhosis, chronic renal failure, Hodgkin's disease; children and adults with oncohematological diseases; HIV-infected; children and adults with cerebrospinal fluid leakage; children and adults after cochlear implantation; children and adults with sickle cell disease; with anatomical asplenia, or planning or having already undergone removal of the spleen. This should also include the so-called “organized” contingents (children attending kindergartens, students living in dormitories, military personnel, residents of nursing homes, prisoners and other adults and children living in overcrowded conditions). The presence of bad habits (alcohol, smoking) is also a risk factor.
Pneumococcal infection
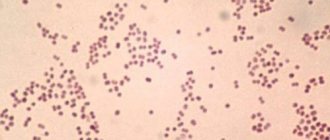
| S. pneumoniae under an electron microscope |
Pneumococcal infection is a group of human infectious diseases caused by pneumococcus (Streptococcus pneumoniae), which are widespread.
The source of infection is:
- patients with a clinically significant form of the disease
- carriers of pneumococci
The spread of bacteria occurs through coughing, sneezing or close contact between people, as well as through contact with objects that have come into contact with saliva (spoons, cups, toys). The danger of getting sick exists all year round. Children can easily get the bacterium from adult carriers, whose immunity can more easily cope with pneumococcus, or from other children in the family or children's group.
Pneumococcus enters the nasopharynx and can remain there for a long time without causing harm. This period is called carriage of the infection. In this case, the child can become a source of infection for family members, especially the elderly. The level of carriage of pneumococci in children is most often observed at the age of 4-5 years (up to 90% of cases). The maximum level of carriage is observed in organized groups - children's homes, orphanages (up to 86%), kindergartens (up to 72%). Under the influence of unfavorable factors, pneumococcus can suddenly cause pneumonia, or enter the bloodstream and cause sepsis (blood poisoning) or reach various organs, including the brain (meningitis), heart (endocarditis).
Pneumococci have little resistance in the external environment. They die from the action of conventional disinfectants; at a temperature of 60⁰C they die within 10 minutes. However, they are resistant to drying out. In dried sputum they remain viable for 2 months.
Today, there is a big problem of antibiotic resistance, that is, the resistance of pneumococci to a number of antibacterial drugs, which creates additional difficulties in treating the disease.
Risk groups for infection
- Children under 2 years of age whose immune cells are not able to fight the pathogen. Children in the first six months of life have maternal antibodies, the number of which greatly decreases after 6 months of life, and therefore the risk of developing infection increases
- Children and adults with immunodeficiency (chronic diseases of the respiratory system, cardiovascular system, diabetes mellitus, renal failure, cirrhosis of the liver; HIV infection, cancer, blood diseases)
- Age-related immunodeficiency (elderly people over 65 years old)
- Persons with tobacco and alcohol addiction
Unfavorable factors for the development of the disease: hypothermia, decreased local immunity as a result of frequent respiratory infections, stressful situations and overwork, hypovitaminosis.
Incubation period: from the moment of infection to the development of the disease - from 1 to 3 days.
Pneumococcal pneumonia
Pneumonia is characterized by high temperature - rising to high (febrile) numbers - 38-39 ° C, chills, severe weakness, muscle pain, shortness of breath, rapid heartbeat; Soon a wet cough with mucopurulent sputum (yellowish-greenish in color) appears, and sometimes chest pain occurs when coughing. Pneumonia due to pneumococcal infection can be lobar or focal. Lobar pneumonia is more severe; acute respiratory failure, abscesses, and pleurisy may develop.
Pneumococcal meningitis
| Mining syndrome |
Pneumococcal meningitis begins acutely with an increase in body temperature to 40°C, and a diffuse headache of a bursting nature appears. Most patients experience repeated vomiting and increased sensitivity to all types of irritants a little later. During the first 12-24 hours from the onset of meningitis, a detailed picture of meningeal and cerebral syndromes is formed: stiff neck, Kernig's sign, Brudzinski, consciousness is initially preserved, and then gives way to a state of stupor, stupor, coma.
Pneumococcal otitis media
Pneumococcal otitis is characterized by fever, pain in the ear, and hyperacusis (distorted perception of sounds, in which relatively weak sounds are perceived as overly intense). Pneumococcal sepsis
Pneumococcal sepsis
manifested by infectious-toxic syndrome (fever, weakness, headaches), enlarged spleen, symptoms of damage to various organs and systems (lungs, heart, intestines, kidneys, meninges).
After suffering a pneumococcal infection, a low-strength, short-term immunity is formed, which does not protect against re-infection with another serotype of pneumococcus.
If you or your child experiences one of the above symptoms, contact a medical facility immediately!
Prevention
- nonspecific (isolation of patients, maintaining immunity, vitamin prophylaxis, timely treatment of acute respiratory infections, playing sports, hardening, giving up bad habits)
- specific - vaccination, especially for young children and adults over 60 years of age.
Several years ago, vaccination against pneumococcus in Russia was not a mandatory preventive measure, and was carried out only in certain cases: for example, children suffering from various chronic diseases (bronchitis, heart disease, etc.), diabetes mellitus, HIV-infected children, etc. .d. However, against the backdrop of an increase in the number of diseases caused by pneumococcus, as well as the deterioration of the epidemiological situation in the country, it was decided to include vaccination against infections caused by pneumococci in the National Vaccination Calendar starting in 2014. It should be noted that mandatory immunization against pneumococcus is a normal practice for most developed countries, and can significantly reduce the risk of serious diseases, primarily in children.
Everyone decides for themselves whether or not to get vaccinated.
Be healthy!
Paramedic of the prevention department
S. Ryazanova
Print Email
Symptoms
Symptoms of pneumococcal infection, which causes pneumonia, include fever, cough, shortness of breath and chest pain. Symptoms of pneumococcal purulent meningitis are a stiff neck, severe headache, fever, confusion and disorientation, and photophobia. The initial manifestations of pneumococcal bacteremia (blood poisoning, the most severe form with a mortality rate of up to 50%) may be similar to some symptoms of pneumonia and meningitis, and may also include joint pain and chills.
In this regard, doctors again and again warn about the dangers of self-medication! You should not try to cope with the disease on your own, using commercials for various drugs and their availability in pharmacy chains as a methodological guide.
Complications after an illness
Pneumococcal meningitis is particularly severe, the incidence of which is about 8 per 100 thousand children under 5 years of age. On average, about 83% of cases occur in children under 2 years of age. Despite the fact that the pneumococcus Streptococcus pneumoniae ranks third after Haemophilus influenzae type b (hemophilus influenzae type b) and Neisseria meningitidis (meningococcal infection) as an infectious agent responsible for the development of this disease, the prognosis for pneumococcal meningitis is much more serious. Complications in the form of mental retardation, impaired motor activity, epilepsy and deafness occur significantly more often than in the outcome of bacterial meningitis of other etiologies.
Pneumonia caused by pneumococcus S. pneumoniae is most often complicated by pulmonary empyema (accumulation of pus in the pleural cavity, causing a decrease in the respiratory surface of the lung tissue), which leads to death (up to 2/3 of cases for empyema). In Russia, out of 500 thousand cases of pneumonia per year, 76% have pneumococcal etiology in adults and up to 90% in children under 5 years of age. The frequency of pneumococcal pneumonia among children under 15 years of age is 490 cases per 100 thousand, in children under 4 years of age - 1060 cases per 100 thousand.
Pneumococcal bacteremia in most cases (up to 80%) occurs with symptoms of fever without a focus of infection. The incidence of bacteremia caused specifically by S. pneumoniae is 8-22% in young children. It is pneumococcal sepsis with the development of severe shock damage to organs that is the most severe and life-threatening form of pneumococcal infection. The frequency of this nosological form in children under 5 years of age averages 9,000 cases per year; the mortality rate reaches 20-50%.
According to world statistics, the proportion of pneumococcal otitis media ranges from 28 to 55% of all registered cases. Pneumococcal acute otitis media is characterized by a more severe course and a high risk of otogenic complications, including a tendency to perforation of the tympanic membrane. Pneumococcal otitis media is the most common cause of hearing loss in children.
Risk of developing pneumococcal infections:
- In healthy people, the risk is 8.8 per 100,000.
- In patients with diabetes mellitus – 51.4.
- In adults with chronic lung diseases – 62.9.
- In patients with chronic heart disease – 93.7.
- for those suffering from cancer – 300.4.
- For HIV-infected people – 422.9.
- In patients with oncohematological diseases - 503.1 per 100,000.
Pneumococcal meningitis
It is customary to distinguish two main forms of pneumococcal meningitis: 1) acute, with a variant of the malignant syndrome of the Uterhouse-Fridrichsen type (fulminant form); 2) protracted and its variety - recurrent. Acute forms of pneumococcal meningitis occur mainly in older children and adults. They are characterized by a sudden onset with an increase in temperature to 38°, less often to higher numbers, severe initial toxicosis with cerebral phenomena (impaired consciousness) and encephalitic reactions (tremor of the limbs, convulsions). In some cases, in the first days of the disease, paresis of the cranial nerves, most often the abducens and oculomotor, is detected. Mono- and hemiparesis occur occasionally.
The onset of the disease is acute. Characterized by a sharp rise in body temperature to 39-40°C, a rapid increase in intoxication: general weakness, pale skin, periorbital cyanosis, refusal to eat and drink. Anxiety, severe headache, and repeated vomiting appear. Young children are characterized by a monotonous moaning cry; the large fontanelle bulges and is tense, the sutures of the skull may diverge with an increase in head circumference. On days 2-3 of the illness, meningeal symptoms are detected, with neck stiffness especially pronounced. In most patients, pneumococcal meningitis from the first days of illness proceeds as meningoencephalitis. Characterized by rapid depression of consciousness, repeated convulsions, the appearance of focal symptoms in the form of hemiparesis, oculomotor disorders, hyperkinesis, and ataxia. Gradually, by the 3-4th day of illness, a convulsive-comatose status develops with an increase in symptoms of dislocation and herniation of the brain stem.
With the development of sepsis, damage to other organs may occur: hemorrhagic rash on the skin (like meningococcemia), pneumonia, endo- and pericarditis, arthritis, etc.
With timely and adequate treatment, improvement occurs in the first week, and reverse development of meningeal and cerebral symptoms occurs within 2 weeks. However, cerebrospinal fluid sanitization occurs no earlier than 2-4 weeks. A protracted or recurrent course is often observed. In most cases, the prognosis is unfavorable - half of the children remain with severe neurological defects and impaired psychophysical development. Death is observed in 28-50% of cases, more often in the first three days of the disease, due to cerebral edema.
Pneumococcal meningitis, which occurs against the background of an existing primary source of inflammation (purulent otitis, mastoiditis, sinusitis, pneumonia), begins subacutely, has few symptoms, but is characterized by a particularly severe course and more often than primary pneumococcal meningitis ends in death. With a septic course of the disease, a hemorrhagic rash may appear on the skin, similar in nature and localization to meningococcal rash. However, at the beginning of the disease, the rash can be roseolous-papular and only in the subsequent days of the disease transform into hemorrhagic. Unlike meningococcal rash, with pneumococcal meningitis it is more persistent and slowly develops back. Unfavorable outcomes of this course of the disease are usually due to late diagnosis and late started etiotropic treatment. This explains the frequency of relapses of the disease characteristic of pneumococcal meningitis, as well as the fact that 22–24% of children after the disease remain with neurological complications in the form of distinct neurological symptoms: deafness, blindness, amnesia, paralysis, and other signs of central nervous system damage.
The outcomes of pneumococcal meningitis largely depend on timely diagnosis and adequate treatment. If these rules are not followed, the disease takes a protracted course and often ends in death. There are three groups of causes of death. The main cause of death is meningoencephalitis with pronounced signs of cerebral edema and swelling. Another reason is severe pulmonary heart failure, which developed against the background of damage to the central nervous system. And the third reason is a septic process with the development of thrombohemorrhagic syndrome against the background of central nervous system damage.
The clinical picture of meningitis is manifested by general infectious, cerebral and meningeal syndromes; laboratory - inflammatory changes in the cerebrospinal fluid.
General infectious syndrome. Typical is the acute onset of the disease with an increase in body temperature to febrile levels, often hyperthermia, chills, lethargy, pale skin, refusal to eat and drink. From the cardiovascular system - muffled heart sounds, changes in heart rate, instability of blood pressure.
General cerebral syndrome . Characteristic symptoms: - intense headache, diffuse (bursting in nature) or predominant in the frontotemporal region; - vomiting is repeated or repeated, not associated with food intake, and does not bring relief; — disturbance of consciousness (psychomotor agitation, doubtfulness, stupor, coma); - convulsions (from convulsive twitching of individual muscles to a generalized convulsive seizure); - pronounced venous network on the head, eyelids; - dilatation of veins in the fundus.
In young children: monotonous, “brainy” cry; bulging and tension of the large fontanel; divergence of the sutures of the skull; “sound of a cracked pot” upon percussion of the skull (Matseven’s symptom).
Meningeal syndrome . The most important symptoms are: - forced position of the child in bed (head thrown back, arms bent at the elbows; brought to the body, legs bent at the knees and hip joints); - rigidity of the neck muscles (passive flexion of the patient’s head to the chest is not possible due to tension in the muscles that straighten the head); - Kernig's sign (a patient lying on his back bends his leg at a right angle at the knee and hip joints; passive extension of the leg at the knee joint with a bent hip is not possible due to tension in the posterior thigh muscles); — Brudzinski’s symptom I (studied simultaneously with stiff neck: when the patient’s head is passively flexed while lying on his back, the legs bend at the knee and hip joints); — Brudzinski’s sign II (the same bending of the legs when pressing on the symphysis pubis); - Brudzinski's symptom III (studied simultaneously with Kernig's symptom; when trying to bend the leg at the knee joint, the second leg is bent at the knee and brought to the stomach); - Lessage's symptom (an infant is taken by the armpits with both hands, holding the head from the back with the index fingers, and raised, an involuntary pulling of the legs towards the stomach occurs due to their flexion at the hip and knee joints); - Mondonesi symptom (pressure on the eyeballs through closed eyelids is painful); - Bekhterev's symptom (local pain when tapping along the zygomatic arch); - general hyperesthesia, hyperacusis, photophobia.
In children, complete meningeal syndrome is rarely observed. Dissociation of symptoms is characteristic: neck rigidity is most consistently detected, and Kernig's sign is somewhat less common.
Syndrome of inflammatory changes in the cerebrospinal fluid . Liquor is produced by the choroid plexuses (plexus chorioideus) of the 3rd and 4th ventricles (0.35 ml/min, 500-600 ml per day). Exceeding the production of cerebrospinal fluid (>1 ml/min) sharply impedes the outflow of cerebrospinal fluid through Pachyon granulations into the pia mater. Cerebrospinal fluid pressure is measured with a special monometer or a graduated glass tube and is expressed in millimeters of water (mmH2O). In the supine position, normal cerebrospinal fluid pressure during lumbar puncture is 100-150 mmH2O. Art. CSF pressure is often assessed by the number of drops flowing from the puncture needle within one minute (the norm is 40-60 drops/min).
Normally, cerebrospinal fluid is clear and colorless. Contains mononuclear cells (lymphocytes, monocytes), the number of which decreases with age and is: in newborns - 20-25 cells per 1 μl; at 6 months - 12-15 cells in 1 µl; from 1 year - 1-5 cells in 1 µl. An increase in the number of cells in the cerebrospinal fluid is called pleocytosis.
The protein content in cerebrospinal fluid ranges from 0.10 to 0.33 g/l, sugar - 0.45-0.65 g/l, chlorides - 7.0-7.5 g/l.
Inflammatory changes in the meninges are accompanied by the following signs in the cerebrospinal fluid: - increased cerebrospinal fluid pressure - flows out, as a rule, in a stream or frequent drops, possibly in rare drops (with an increase in protein content or blockage of the intrathecal space with inflammatory exudate); — possible change in transparency (cloudy) or color (white, yellow-green, etc.); - pleocytosis with a predominance of neutrophils, lymphocytes or mixed; - increased protein content; - changes in sugar and chloride levels.
Meningism syndrome . In the acute period of various infectious diseases, it is possible to develop a clinical picture of meningitis without inflammatory changes. cerebrospinal fluid. This condition is based on reflex dysfunction of the choroid plexus and increased production of cerebrospinal fluid. Most often, this syndrome occurs in children with an unfavorable premorbid background (hypertensive-hydrocephalic syndrome, minimal cerebral dysfunction, organic brain damage). A final diagnosis is possible only after a lumbar puncture and examination of the cerebrospinal fluid. The vast majority of patients have elevated cerebrospinal fluid pressure; the liquid is clear, colorless, the number of cells is normal; protein concentration is not changed. Characteristic is the rapid reverse dynamics of cerebral and meningeal symptoms (within 1-2 days) against the background of a decrease in intoxication and dehydration therapy.
Treatment
A global problem in the world is the increasing resistance of pneumococci to antibiotics - this means that treatment of pneumococcal infections with antibiotics is often ineffective. The main factor in the development of antibiotic resistance in pneumococcus is the irrational use of antibacterial drugs. When conducting monitoring in 2004-2005. 11% of pneumococcal strains were resistant to penicillins, 7% to macrolides, 40.8% to co-trimoxazole. But already in 2011-2012. a similar study showed that already 29% of S. pneumoniae strains have reduced sensitivity or are resistant to penicillin, 26% of strains are resistant to macrolides, 50% of strains are resistant to co-trimoxazole. According to the latest data, up to 10% of strains of pneumococcal infection have acquired resistance to combinations of broad-spectrum penicillin with β-lactamase inhibitors, which is extremely unfavorable prognostically, since due to the rapid development of the disease (2-3 days) there is no time to determine sensitivity to antibiotics , as a rule, no, and patients with severe pneumococcal infection often die, despite the introduction of standard antibacterial drugs.
Effectiveness of vaccination
According to WHO, world experience has shown that mass vaccination reduces the incidence of pneumococcal meningitis and severe pneumonia in children by more than 80%, and the incidence of all pneumonia and otitis media by more than a third. The carriage of pneumococci in children is decreasing, and accordingly, unvaccinated children and adults get sick less. The World Health Organization projects that global use of pneumococcal vaccination will prevent 5.4 to 7.7 million child deaths by 2030.
Vaccination is the only highly effective way to significantly influence the morbidity and mortality of pneumococcal infections and reduce the level of antibiotic resistance in S. pneumoniae. With evidence of the safety and effectiveness of pneumococcal conjugate vaccines, WHO and UNICEF believe it is necessary to include these vaccines for children in all national immunization programs. At the same time, it should be noted that the maximum protective effect is achieved with routine vaccination of all children under 2 years of age, and not just patients in risk groups.
Specific vaccine prevention of pneumococcal infection
Vaccination is recognized as the most effective method of preventing PI. According to the WHO position, vaccination is the only way to significantly influence the morbidity and mortality from PI and reduce the level of resistance to ALD. Having confirmed the safety and effectiveness of pneumococcal vaccines, WHO and UNICEF experts consider it necessary to include pneumococcal vaccines with a proven safety and effectiveness profile in all national immunization programs.
When carrying out VP PI, it is necessary to be guided by the current regulatory and methodological documents on the organization of immunization, primarily the National Calendar of Preventive Vaccinations and the Calendar of Preventive Vaccinations for Epidemic Indications, as well as instructions for the use of immunobiological drugs.
In the Russian Federation, vaccination against PI of all adults over the age of 50 years and patients at risk (including HIV-infected patients) is currently included as a mandatory measure in clinical recommendations and standards of medical care for therapy, cardiology, neurology, oncology, oncohematology, nephrology, pulmonology, allergology, immunology, endocrinology and transplantology.
Vaccination against PI is aimed at preventing the occurrence of generalized forms of pneumococcal infection (iPI), pneumonia, reducing morbidity, disability and mortality of the population from these infections. According to WHO data for different countries, it has been convincingly shown that specific CAP is the most accessible and cost-effective way to prevent PI. This is also confirmed by the results of domestic research.
Vaccines
Vaccination has been used to combat pneumococcal infection for more than 30 years. Since 1981, the pneumococcal polysaccharide vaccine has been used. Since 2000, pneumococcal conjugate vaccines have been used in international practice for immunoprophylaxis of pneumococcal infection in young children.
To date, the following vaccines have been registered in Russia: two pneumococcal conjugate vaccines (10-valent and 13-valent - PCV10 and PCV 13) and one - polysaccharide 23-valent (PPV23). The latter is used in children over 2 years of age and adults. While conjugate vaccines are recommended for immunization of children from 2 months of age and adults aged 50 years and older. PCV13 is also registered in the US and EU for use in broader age groups (children 6 weeks to 17 years and adults 18 years and older). In the near future, the age indications for PCV13 are also expected to expand in Russia.
In 2013, the pneumococcal 13-valent conjugate vaccine Prevenar13 was awarded the Galen Prize as the best biotechnological product of the year.
More about vaccines
Latest epidemics
Most diseases are sporadic. Outbreaks of pneumococcal infection are uncommon, but can occur in closed communities, for example, in nursing homes, children's day hospitals and other similar institutions. However, large outbreaks of meningitis caused by serotype 1 have been reported in the African meningitis belt.
WHO estimates that of the 8.8 million children under 5 years of age who died in 2008, 476 000 (333 000 – 529 000) deaths were due to pneumococcal disease. Morbidity and mortality rates are higher in developing than in economically developed countries.