What it is?
Photo 1. Girl with Dandy-Walker syndrome
Dandy-Walker syndrome belongs to a group of incurable congenital defects that affect the functions of the nervous system. In the ICD-10 the disease is assigned code Q03.1: “Atresia of the foramina of Magendie, Luschki .
The defect was first described in 1921 by neurosurgeon Walter Edward Dendy. He studied the causes of hydrocephalus. Independently of each other, the study was also carried out by Arthur Earl Walker. In 1942, his article about the absence of ducts in Luschka and Magendie was published. The work of neurosurgeons is taken as the basis for the study of the defect.
Features of Dandy-Walker syndrome:
- formed during the period of intrauterine formation of the brain;
- the cause is considered to be chromosomal disorders;
- the defect is detected by ultrasound at 13–23 weeks of gestation;
- one case per 25 thousand fetuses and infants is diagnosed;
- the defect is more often detected in girls;
- in children with the syndrome, the skull may not be deformed;
- children with cerebellar anomalies are more likely to die at an early age;
- compression of the brain by a cyst affects the functions of internal organs through the nervous system;
- often accompanied by other congenital defects.
Photo 2. Signs of Dandy-Walker syndrome
Dandy-Walker syndrome is characterized by an anomaly in the structure of the cerebellum and hydrocephalus. The fourth ventricle of the brain expands. At the same time, a cyst with cerebrospinal fluid forms in the area of the posterior cranial fossa, since the circulation pathways (foramina of Luschka, Magendie) are narrowed or absent. An anomaly of the vermis is also identified: the connecting structure of the cerebellar lobes does not develop or is formed incorrectly.
As a result of Dandy-Walker syndrome, the circulation of cerebrospinal fluid is disrupted . The increasing volume of fluid inside the skull increases pressure, compressing brain tissue. This disrupts the functions of the organ, inhibits the child’s mental development, causes headaches and muscle spasms. The accumulation of cerebrospinal fluid from the inside expands the skull, puts pressure on the nuclei of the brain nerves, deforms the head, and impairs the functioning of the central nervous system. As a result of the disease, life expectancy decreases and the death of the child may occur .
Manifestations of the disease
The symptoms of Dandy-Walker syndrome are varied. Both practically normal development of the child after birth and severe neurological changes leading to severe disability and even death are possible. According to some data, normal development of intelligence occurs in half of the cases of isolated defect; it is even possible that the syndrome is accidentally discovered during examination of adults.
children with Dandy-Walker syndrome
The intrauterine course of the pathology is determined by the degree of brain damage, the increase in hydrocephalus, and the presence of other developmental defects. The prognosis is significantly worse when the syndrome is diagnosed before birth. With deep disturbances in the formation of the brain, hydrocephalic syndrome comes to the fore among other manifestations:
- Increase in head diameter;
- Bulging of the fontanel.
The increase in the diameter of the skull occurs mainly due to the occipital region, in which a cyst forms, causing thinning and stretching of the bone base. With severe hydrocephalus, the baby's head actively grows during the first two months, and at the same time, the sutures between the bones in the front or back part separate. In addition, it is characteristic:
- Increased nervous excitability (reflexes);
- Oculomotor disorders - nystagmus, strabismus;
- Attacks of respiratory arrest;
- Facial nerve paresis.
Symptoms of cerebellar disorders in newborns cannot be identified, and even a severe defect in the formation of cerebellar structures does not always cause significant signs of ataxia (motor disorders), which is recorded in only a third of patients.
Much more often than motor disorders, disorders of mental activity and intelligence occur, which manifest themselves against the background of general motor “awkwardness.” 25% of patients with a hypoplastic cerebellum have signs of autism, and therefore experts are trying to find a relationship between changes in the cerebellum and autism in children.
Children with hydrocephalus at an early age are restless, sleep poorly, are characterized by a monotonous cry, increased reflexes, floating eye movements and their rolling, pronounced vessels of the cornea, a noticeable subcutaneous venous network as the size of the head grows. Spontaneous motor activity of newborns may be weakened, convulsions and tetraparesis are possible due to muscle hypertonicity.
At an older age, a lag in mental and intellectual development becomes noticeable; children cannot learn, get tired quickly, and do not assimilate new information well, which makes the adaptation process extremely difficult. In severe cases, learning is completely impossible, and therefore the child needs constant outside help, care and consideration of the issue of disability.
Motor development is noticeably delayed. In severe forms of the anomaly, children cannot learn to roll over, crawl, sit up and walk in a timely manner, do not keep their eyes on toys, get tired quickly and often cry. Possible nutritional disorders with malnutrition, a general decrease in immunity, and frequent infectious diseases.
The combination of a defect of the nervous system with other anomalies of organ development predisposes to serious complications, including not only brain dysfunction, dementia, convulsive syndrome, but also heart failure, a tendency to pneumonia with heart defects, chronic renal failure and uremia with congenital polycystic disease, which aggravates phenomena of cerebral edema and can cause the death of the patient.
With severe occlusive hydrocephalus, death can occur in early infancy from cerebral edema, fatal arrhythmias, respiratory arrest due to compression of brainstem structures, severe pneumonia and other infectious complications.
In adults, a gradual increase in hydrocephalus with cranialgia, decreased memory and attention, irritability, a tendency to depression, morning sickness and vomiting at the height of headaches is possible. In severe cases, convulsive syndrome occurs. There may be problems with coordination and performing small movements, uncertainty when walking, and visual disturbances.
Causes and triggers in children
Evidence-based medicine experts have not established the exact causes of congenital cerebellar anomalies. Doctors believe that Dandy-Walker syndrome occurs due to a genetic disorder, a chromosomal disorder, or excessive production of cerebral fluid. Triggers (provoking factors) include the influence of toxic and harmful substances that poison a woman’s body.
Reference! The risk of a congenital defect in the fetus during a second pregnancy does not exceed 7% if there is no genetic prerequisite for the mother or father.
The risk of fetal defects increases in pregnant women:
- alcoholics;
- smokers;
- drug users;
- taking medications with embryotoxic or teratogenic effects.
A genetic disorder can be caused by radiation or cytomegalovirus, rubella, or other viral infections during pregnancy. A trigger is also considered to be the presence of diabetes mellitus, an autoimmune disease, or a metabolic disorder in a woman. Heredity plays a major role, that is, congenital defects have already been recorded in the family history.
Causes
The exact causes have not been established. There are several theories. These include the arrest of embryonic development during the formation of the rhomboid part of the brain, the absence of an outlet in the fourth ventricle, which is due to the late opening of the Magendie passage. Another probable cause is the formation of a typically ventricular (IV ventricle) villous plexus in the roof area of the rhomboid region of the brain.
The appearance of a cyst in the area of the cranial fossa, located behind, leads to disruption of the formation and growth of the cerebellar vermis and corpus callosum. Hereditary and teratogenic (physical, chemical, biological agents) factors take part in the development of the pathological process. At risk are pregnant women of the older age group, expectant mothers with a similar diagnosis and a history of other developmental defects. Provoking factors:
- Viral diseases (rubella, cytomegalovirus infection, herpes, measles) suffered by the mother in the first trimester of gestation.
- Diabetes mellitus diagnosed in the mother.
- Alcohol intoxication of chronic form.
- Hereditary predisposition.
Dandy-Walker malformation is a pathological condition that is often a consequence of genetically determined diseases (Meckel, Meckel-Gruber, Warburg syndrome), which confirms the important role of hereditary factors in pathogenesis.
Symptoms and signs
Before the birth of the baby, the pregnant woman does not experience any disturbance or complication of gestation. In the fetus, ultrasound reveals only cerebellar defects: underdevelopment, enlargement of the fourth ventricle, and the formation of a cerebrospinal fluid cyst.
After birth, unnatural behavior of the baby is added to the ultrasound signs of Dandy-Walker syndrome. Because of his headache, he constantly cries. Compression of the brain by a cyst leads to convulsions, twitching of the limbs, and increased muscle tone. This is manifested by impaired motor skills, involuntary rotation of the eyes, and the joints of the arms and legs are bent.
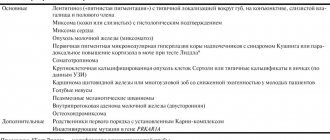
Signs of a congenital defect of the cerebellum and cerebrospinal fluid tract include:
- large size of the top of the head;
- soft skull;
- protrusion of the fontanel;
- deformation of the face, back of the head;
- stopping breathing (apnea);
- dropsy of the brain (not everyone);
- fusion of fingers or other congenital defect;
- long-term failure of fontanelle to heal.
As you grow older, mental retardation and impaired motor skills (coordination) appear. The child is capricious, irritable, cannot walk smoothly or stand steadily. Seizures occur periodically. In the morning, vomiting, nausea occur, and the headache intensifies. During the examination, visual impairment is revealed.
50% of children have no significant symptoms. A child from this group does not have a deformed head. But coordination of movements is impaired, the gait is swaying, and the legs are widely spaced while walking. There is a slight lag in the development of psychomotor skills and mental activity.
Reference! Rarely, symptoms and signs of a birth defect appear in children after 4 years of age or in adults.
Ultrasound of a pregnant woman
There are several main ultrasound signs of Dandy Walker syndrome, which can be determined already during a screening study at 21-23 weeks of pregnancy. During this period, an abnormality of intrauterine development can be suspected based on the detection of the following symptoms in the fetus:
- If the equipment has detected a formed or developing cyst of the posterior cranial fossa;
- disturbances in the structure of the cerebellum;
- expansion of the fourth ventricle of the brain.
In later stages of pregnancy, from about 31 weeks, in addition to these signs, the fetus will also show:
- Non-fusion of the palate and upper lip (“cleft palate”, “cleft lip”).
- Fusion of the fingers on the limbs.
- Disturbances in the structure of the urinary system, in particular the kidneys.
Dandy-Walker syndrome in adults
Statistics contain information when a cerebellar defect was diagnosed after a person reached adulthood. The disorder is more often referred to as a type of cerebral hydrocele. In these cases, the signs and symptoms of Dandy-Walker syndrome appear gradually after age 18.
As the condition worsens:
- the volume of the head increases;
- the occipital bone moves outward;
- I have a headache and medications don’t help;
- convulsions occur periodically;
- increased muscle tone - muscles are tense, sometimes to the point of spasm;
- Coordination deteriorates - unsteady gait, unclear movements;
- motor skills slow down;
- movement of the eyeballs is partially uncontrolled.
Intellectual impairments include memory impairment and loss of acquired skills. A person stops recognizing relatives and friends, becomes irritable, forgets how to read, dress, write, and so on.
Treatment of the syndrome
Treatment for this disease makes virtually no sense. Despite this, in some cases treatment is carried out. Sometimes this even leads to success.
It is worth saying that even with a successful outcome of treatment, the child will not be healthy. He will still have some signs (usually visual) that indicate he has Dandy Walker syndrome.
Drug treatment
Drug treatment is prescribed only in cases of mild disease. In such a situation, the patient is prescribed diuretics (for example: Mercuzal, Promeran, Novurit ), which reduce the level of fluid in the skull, relieve headaches and dizziness.
Surgery
If the enlargement of the skull begins to progress, surgical intervention is necessary. In this operation, the goal is to reduce intracranial pressure by shunting the fourth ventricle of the brain.
Surgery is also possible to improve the drainage of fluid from the brain and reduce the size of the child’s head.
In other cases, surgery is not used for this disease.
Home Remedies
Unfortunately, treating such a serious illness as Dandy Walker syndrome is impossible at home. Parents can only help their child with soothing decoctions if the patient has a high degree of irritability. In addition, it is permissible to use other non-traditional remedies to relieve a child of headaches and dizziness.
Doctors advise children to engage in various exercises without overstressing the patient’s muscles. This will prevent complete atrophy of the body muscles. You can resort to physical exercise only in case of a mild form of the disease. Otherwise it will not bring any results.
Some doctors advise hardening children who have Dandy Walker syndrome. But this is a rather controversial point of view. In this matter, consultation with the child’s attending physician is necessary. As practice shows, in most cases of hardening, the symptoms worsen, and the child’s condition approaches critical. In view of this, the opinions of doctors are divided from a categorical “no” to an unconditional “yes”.
Forms
During the prenatal period, doctors classify complete and incomplete forms of the defect. In the first case, the cerebellum is undeveloped: the vermis is absent, the cyst is connected to the fourth ventricle. In the second type, the defect is partially formed. The structure between the lobes is visible in places on ultrasound; the fluid cavity does not communicate with the entire surface of the worm.
After childbirth, doctors distinguish open and closed forms of the defect. The difference between these types is based on the patency of the liquor pathways. In the first case, there is a communication of the ventricle through the foramina of Luschka and Magendie with the subarachnoid space. In the closed form, the ducts are closed.
Main features
The disease is classified according to the degree of insufficiency in the development of cerebellar structures. Based on this, complete and incomplete forms of the disease are distinguished.
Manifestations of the disease in newborns and in adult children differ. A specialist can see the first signs on an ultrasound in the prenatal period, these include:
- The size of the fourth ventricle does not correspond to the norm for the duration of pregnancy - it is significantly enlarged.
- Underdevelopment of the cerebellum.
- The presence in the cranial fossa of a cavity filled with fluid - a cyst.
These signs give the doctor reason to make an assumption about the presence of the described disease. The diagnosis is confirmed by a combination of internal and external manifestations:
- Disproportion of the child's skull. The head seems disproportionately large.
- Craniotabes, in which the flat cranial bones in the area of the fontanelles become thinner, softening of the bone tissue occurs.
- The occipital bone loses its correct outline.
- Enlarged fontanels.
- Weakness of cry.
- Hydrocephalus is an accumulation of fluid caused by a violation of its outflow from the ventricles of the brain.
- Irregularly formed jaws, nasal turbinates.
- Nystagmus is involuntary oscillatory movements of the eyeballs.
- Uncontrolled convulsive contractions of the muscles of the arms and legs.
- Syndactyly is the fusion of the digital phalanges of the upper or lower extremities.
- Constantly bent position of the limbs, caused by tension in the muscle tissue (spastic tetraparesis).
- Motility disorders.
- Restless behavior.
In children over the age of one year, the pathology is manifested by attacks of headache, nausea and vomiting, irritability, impaired coordination of movements, vision problems, and mental and intellectual development delays.
Often the disease is accompanied by heart defects, kidney disease, and deviations in the development of facial bones.
Diagnostics
A woman is examined by ultrasound once every trimester. Ultrasound scanning is harmless to the fetus and can detect abnormalities in the early stages. A brain scan can reveal developmental abnormalities as early as 2.5 months of pregnancy. But to confirm Dandy-Walker syndrome, an ultrasound is repeated at 20–23 weeks of gestation. At this stage, a cerebrospinal fluid cyst, abnormal structure of the cerebellum, and deformation of the fourth ventricle are already visible.
If signs are detected again, the woman is prescribed an MRI. Based on the form of the birth defect, doctors assess the severity of Dandy-Walker syndrome. Due to the incurability of the disease, termination of pregnancy is recommended. But the final decision is made by the child’s parents.
After birth, the doctor examines the baby, feels and measures the head. Doctors evaluate the symptoms and external manifestations of the disease, then the child is sent for an ultrasound of the internal organs and neurosonography. From the mother, the doctor finds out the family history, lifestyle, course of pregnancy, cases of self-medication and the type of drugs used. It is advisable for the mother to consult a geneticist.
Important! The inexperience of an uzist or doctor increases the risk of error. To confirm the diagnosis, a pregnant woman must consult and/or undergo further examination with 2–4 doctors from independent medical institutions.
Dandy Walker Anomaly
Dandy-Walker anomaly (syndrome) is a malformation of the brain, which is characterized by a triad of symptoms - hypotrophy of the cerebellar vermis and/or cerebellar hemispheres, cysts of the posterior cranial fossa, hydrocephalus of varying degrees.
For your information, brain defects occur in 1 in 100 births, of which 80% are hydrocephalus of various origins, incl. and atrophic, of which from 9.5% to 12% are Dandy-Walker syndrome (DSW), but it is believed that this figure is underestimated, because There are forms of SDS without hydrocephalus.
The etiology of the syndrome is unknown. SDS can be a manifestation of genetic diseases such as Meckel syndrome (autosomal recessive path - microcephaly, polydactyly, polycystic kidney disease, ocular abnormalities - microphthalmos, optic hypoplasia, congenital heart disease, cryptorchidism, occipital spina bifida), Meckel-Gruber (same + encephalocele), Warburg, Turner, trisomy 9, triploidy, 6p- and other chromosomal aberrations.
It is assumed that factors such as viral infection (CMV, rubella), alcohol, and diabetes in the pregnant woman also play a role. If the syndrome is not associated with a genetic pathology, then the risk of recurrence during repeated pregnancy is 1-5%, and when inherited in an autosomal recessive manner – 25%. Combination with other defects of the central nervous system - 50%, especially often with agenesis of the corpus callosum 7-17%; polymicrogyria, agyria, microgyria, defects of the inferior olive are also common.
During pathological examination, CNS defects are found in 68% of cases with SDS. In addition to CNS defects, congenital heart disease, encephalocele, polycystic kidneys, polysyndactyly, hemangiomas, cleft lip/palate, Klippel-Feil, etc. are often encountered.
The syndrome was first described by Dandy and Blackfan at the beginning of the 20th century; they considered this condition secondary to congenital atresia of the foramina of Magendie and Luschka, which ensures the outflow of cerebrospinal fluid from the 4th ventricle into the subarachnoid space; Walker was the doctor who first performed surgical treatment on a patient with this pathology, so the disease became known as SDS.
Currently, the generally accepted hypothesis is that the syndrome is a complex anomaly in the development of the midline structures of the rhombencephalon. Gardner et al (1974) suggested that the disease is caused by an imbalance between the production of cerebrospinal fluid in the lateral and 3rd and 4th ventricles of the brain.
Its excessive production in the 4th ventricle leads to early expansion and bulging of the rhomboid vault, maximum expansion at the level of the 4th ventricle leads to compression and secondary hypoplasia of the cerebellar vermis, the appearance of a communication between the 4th ventricle and the posterior cranial fossa and the development of a cyst of the posterior cranial fossa.
Diagnostics.
In all cases of detection of cysts of the posterior cranial fossa and any pathology of the posterior cranial fossa, a differential diagnosis with an arachnoid cyst and dilatation of the cistern magna - for SDS, a defect in the cerebellar vermis, through which the 4th ventricle communicates with the cyst of the PCF, is pathognomonic. These changes can be detected by ultrasound and CT/NMRI of the brain both in the postnatal and antenatal periods.
Ultrasound pays special attention to the lower part of the cerebellum, although a definitive diagnosis still requires an MRI of the brain. But with nuclear magnetic resonance imaging there may be difficulties in interpreting the results, so a search is underway for the most informative diagnostic methods; some authors propose radioisotope research methods, others use pneumoencephalography. Karyotyping is mandatory to exclude chromosomal pathology. The main manifestation is progressive hydrocephalus in the closed form of SDS syndrome.
Treatment.
In the absence of hydrocephalus and signs of intracranial hypertension, observation (cases of SDS detection in adults during a routine examination are described). In the presence of symptoms of intracranial hypertension - shunt surgery, the location of implantation of the proximal catheter is debatable (into the cyst - with very large cysts of the posterior cranial fossa; into the lateral ventricle - most often; into the cyst and lateral ventricle - with concomitant occlusion of the “aqueduct of Sylvius”). Since 1983, attempts have been made at intrauterine shunting (surgery on the fetus - placement of a ventriculoamniotic shunt).
Data on the prognosis are contradictory - the first analyzes of the results of treatment in the 60-70s showed an unfavorable prognosis in all cases, and the mortality rate was 50%; subsequently (80-90 years) - survival rate increased to 78-80%, and the intelligence index was more than 80 in 30-60% of survivors, but the functional neurological prognosis was less favorable - many had ataxia, spastic paresis, impaired coordination of movements and associated Problems.
Therefore, now when identifying Dandy-Walker syndrome. antenatally, the issue of termination is decided individually and collectively. If detected postnatally, a full clinical and instrumental examination is required
(especially brain MRI, karyotyping, exclusion of heart defects, kidneys, skeletal system), dynamic observation of a pediatrician, neurologist and, if necessary, a neurosurgeon, for timely surgical correction.
In 2006, in the neonatal pathology department of the Academy of Children's Clinical Hospital, there was a child in whom SDS was suspected antenatally and confirmed after birth. Here is a description of this case.
Child D., date of birth 06/29/2006, was treated in the emergency department from 07/07/2006 to 08/03/2006. Pregnancy 1 (mother -23 years old, father -37 years old), against the background of chronic urogenital infection (mycoplasmosis , chlamydia, condylomatosis, chronic herpetic infection of the genital tract), rehabilitation at 20 weeks, polyhydramnios, anemia, threat of miscarriage, gestosis of the 2 halves, unstable position of the fetus, the woman herself has mental retardation.
According to fetal ultrasound dated 05.05.05 - fetal hydrocephalus, dilation of the cistern magna up to 14 mm. Delivery 1 at 39 weeks, cesarean section due to transverse position of the fetus. At birth: weight 3430 g, height 50 cm, head circumference 37 cm, chest circumference 35 cm, Apgar score 8/9 points. Early adaptation period: tissue pastiness, tendency to hypothermia, mild systolic murmur, torticollis, chin tremor, syndactyly.
Status on admission: moderate condition, restless, rough voice, unstable convergent strabismus, brachycephalic head, BR 2.5-3 cm, head and body alignment to the right, tremor of the hands, spontaneous Moro reflex, muscle tone increased pyramidal type, more on the right, SHR are revived.
The skin is pink and clean. Discharge from the eyes, more on the right. Syndactyly of 2-3 toes of both feet. In the lungs - without pathology, RR 38/min., HR 144/min., soft systolic murmur on the left edge of the sternum.
Examination carried out:
General blood and urine analysis - without pathology. Blood biochemistry – without pathology. Blood test for antibodies to IUI dated July 18, 2006 - antibodies to toxoplasma in the child and mother are negative, to chlamydia trachomatis -A-not detected, G- + 1/80. General immunoglobulins dated July 18, 2006 A-0, M-0.39, G-7.7. NSG: date
07/11/06 – expansion of the bodies of the lateral ventricles up to 7 mm, thickening of the ependyma, expansion of the cistern magna, from
07.20.06 - negative dynamics - increase in ventriculomegaly up to 9 mm (bodies on both sides), thickening of the ependyma, adhesions. L-puncture from 13.07 - increased pressure, in the analysis - B-0.296, Pandi +, cytosis 3 grade, cerebrospinal fluid PCR method for DNA of CMV, toxoplasma, herpes simplex viruses types 1 and 2 were not detected. ECG: date 10.07 – sinus rhythm, vertical position of the electrical axis. Ultrasound dated July 13, 2006 – liver, kidneys, adrenal glands, spleen – without pathology.
EchoCG: 07/14/06 - slight enlargement of the right parts of the heart, secondary ASD 4 mm, valvular apparatus is not changed. LLC – 2.5 mm – conclusion: congenital heart disease, small secondary ASD, slight overload of the right parts, control after 3 months. Examined by a geneticist - MVPR, SDS cannot be ruled out, blood was taken for karyotype 07/24 - 46, XY. MRI of the brain from
07.28.06 – the median structures are not displaced, hypoplasia of the vermis and cerebellar hemispheres with expansion of the greater occipital cistern and the quadrigeminal cistern up to 25-40 mm in diameter, expanded subarachnoid spaces in the frontal and temporal regions, ventricles of a normal shape, bodies of the lateral ventricles up to 13 mm, posterior horns - up to 16 mm, third ventricle 3 mm, fourth 7 * 10 mm.
Conclusion: SDS option. Moderately severe mixed hydrocephalus. Neurosurgeon - there are no indications for surgical treatment. Examination by an ophthalmologist dated July 25, 2006 – opalescence of the cornea, the vessels in the fundus are narrowed, observations regarding congenital glaucoma, dated August 1, 2006 – opalescence of the cornea has decreased.
Treatment was carried out: 10% glycerin, pantogam, local treatment of conjunctivitis. The condition at discharge was satisfactory. Weight 4255 (+825), head circumference 38 (+1 cm). Discharged home with recommendations - observation by a neurologist, OH control once every 7 days - 1 month, then according to the condition, NSG after 1 month, examination ophthalmologist after 7 days - (congenital glaucoma?), observation by a cardiologist. ZRT+ 11.07, 13.07, 17.07.
At 2.5 months. A control NSG was carried out on September 2, 2006 - signs of internal hydrocephalus remained, without increasing over time. Ultrasound of internal organs dated September 20, 2006 - in the parenchyma of the liver and spleen - multiple small hypoechoic inclusions 0.2-0.3 cm without acoustic tracks. Echocardiography dated September 25, 2006 – self-healing of secondary ASD.
At the age of 4.5 months. By ambulance, the child is admitted to the ICU of the CSCH in a very serious condition with signs of intracranial hemorrhage with displacement of the midline structures of the brain, and a cerebral coma quickly develops.
During the examination - NSG dated November 13, 2006 - in the right hemisphere the formation of heterogeneous echogenicity (cavitary, cystic changes with hyperechoic solid areas) with unclear contours and irregular shape; localization - the lower parts of the frontoparietal zones, the right temporal region, the diencephalic region - at least 1/3 of its volume with a displacement of the midline structures to the left up to 5 mm, the cerebral peduncles are deformed - a space-occupying formation of the right hemisphere, occupying at least 1/3 of its area with dislocation median structures, compression of the rostral part of the trunk (brains of the brain) and impaired cerebrospinal fluid dynamics (occlusive hydrocephalus).
KBC from 11.12.-er 2.1, HB 53, reticulocytes 25%, platelets 147t, leukocytes 16.2 thousand, b-1e-1p-12s-63l-15-m-8soe-48mm/hour. Coagulogram dated November 12, 2006 - fibrinogen 0.75, RFMK-6, APTT-176.6, PTI-29%, TV-16.5 sec. antithrombin 3-88%, APTT-2.82, factor 8-108%, factor 9-1.5%, von Willebrand factor-192%.
A consultation was held on November 13, 2006 - there was a mass formation in the brain (tumor? hematoma? due to impaired hemostasis, vascular malformation), but taking into account the location and size, it was inoperable, the child’s condition was recognized as incurable. Received treatment: mechanical ventilation, infusion therapy, hemostatic therapy (fresh frozen plasma No. 3, Novo-Seven No. 1, Dicynone, Vicasol), zinacef, red blood cell transfusion. The condition progressively worsened, stage 3 coma, atony. At 00:80 on November 19, 2006, the death of a child was recorded.
Pathological and anatomical diagnosis: MVPR - CNS - SDS (intrinsic hydrocephalus, hypoplasia of the cerebellar vermis, cystic dilatation of the 4th ventricle), angiomatous malformation (mixed vascular malformation), congenital heart defect - aneurysm of the sinus of Valsalva, lungs - bilobar lungs, limbs - syndactyly 2 -3 toes. Complications: massive intracranial hemorrhage in the right frontoparietal region.
Cerebral coma stage 3. Postanoxic encephalopathy is total necrosis of the brain. Swelling of the brain and spinal cord. Bilateral bronchopneumonia. Concomitant – residual effects of generalized intrauterine cytomegalovirus infection.
Thus, a child with a cerebral defect (CDD) identified antenatally and confirmed after birth in combination with a heart defect, syndactyly and signs of ongoing intrauterine infection required monthly follow-up multidisciplinary observation in a clinical setting for timely detection and correction of dysfunction of damaged organs and systems.
Treatment methods
Patients with congenital defects and their parents are provided with palliative care. This includes methods of supportive therapy, consultations with psychologists and social workers.
Drug and surgical treatment are used for severe symptoms of the defect. If there is no intracranial hypertension, hydrocephalus and other dysfunctions of internal organs, the child is under medical supervision. He should be regularly examined by a neurosurgeon, neurologist, and pediatrician.
Children with Dandy-Walker syndrome are given maintenance therapy with vitamin-mineral complexes and amino acids. Medicines are also prescribed to eliminate the severe symptoms of the defect. To restore the functioning of the heart, kidneys, and other organs, drugs are selected individually according to medical indications.
Drugs prescribed for Dandy-Walker syndrome:
- Sedatives and sedatives - eliminate the child’s irritability and capriciousness.
- Antispasmodics and analgesics - relieve pain.
- Vitamin B - increases the transmission of impulses to neurons.
- Plasma replacement solutions inhibit the development of complications of Dandy-Walker syndrome. They support the vital activity of cells, the functioning of the brain and internal organs.
- Corticosteroids - reduce the production of cerebrospinal fluid in the ventricles of the brain.
- Vasodilators - expand the lumen of blood vessels, facilitate the outflow of cerebrospinal fluid in open forms of the defect, and blood circulation.
- Diuretics - the diuretic effect helps remove excess fluid from the vessels. This reduces intracranial pressure.
- Beta blockers - relieve swelling of brain tissue.
Physiotherapy is also prescribed . It includes exercise therapy, balneotherapy - therapeutic mud, swimming, salt baths. The doctor also prescribes massage. These methods are aimed at reducing the patient’s muscle tone, as well as improving his psycho-emotional state.
The operation is indicated to restore the outflow of cerebrospinal fluid in another way. Two methods are used: ventriculoperitoneal shunting or endoscopic ventriculostomy. In the first case, a soft tube is inserted into the ventricle. Then the catheter is directed subcutaneously behind the ear and in the collarbone area into the abdominal cavity. Liquid will flow into it and dissolve.
During ventriculostomy, a hole is made in the cranial bone, a neuroendoscope is advanced into the ventricle, and excess cerebrospinal fluid is drained. The procedure is minimally invasive, short-lived, the patient is discharged on day 3, no late complications were recorded.
Reference! Surgical treatment eliminates only hydrocephalus and intracranial pressure. Mental abilities, coordination of movements or central nervous system functions are not restored by the operation.
Prevention
There is no specific prevention. A woman should lead a healthy lifestyle and avoid contact with harmful substances. During pregnancy planning, you need to be re-examined and cure any identified sexually transmitted infections. During pregnancy, you should not take medications with teratogenic or embryotoxic properties. These drugs also cause birth defects and defects.
For prevention purposes, you should not skip scheduled visits to the gynecologist and ultrasound. Early detection of infectious and inflammatory diseases and their treatment reduces the risk of birth defects.
What do you need to remember?
- Dandy-Walker syndrome belongs to congenital severe and incurable cerebellar defects.
- The disease can be caused by a virus or any factor affecting the formation of the embryo.
- External signs include head deformation; other symptoms include crying, poor coordination, and mental retardation.
- In adults, signs of the defect appear late.
- The defect has two forms and may be accompanied by dropsy of the brain.
- Symptomatic therapy drugs are used for life; surgery is performed to restore the outflow of cerebrospinal fluid.
- Complications include disruption of the functioning of internal organs and the central nervous system.
- People with severe birth defects do not live long.
- General recommendations are used as prevention: a healthy lifestyle, timely treatment.
Literature
- Neurology and neurosurgery / ed. A.N. Konovalova, A.V. Kozlova; E.I. Gusev, A.N. Konovalov, V.I. Skvortsova: textbook: - vol. 1. - 2009. - 624 p.
- Nikiforov A.S., Konovalov A.N., Gusev E.I. (ed.) Clinical neurology: In 3 volumes - Vol. 3, part 1, part 2. - M.: Medicine, 2004.
- Benda C. Dandy-Walker syndrome or so-called atresia of the foramen Magendie // J. Neuropathol. Exp. Neurol. 1954. Vol. 13. P. 14.
- Snyders RJM, Nicolaides KX Ultrasound markers of fetal chromosomal defects. M.: Vidar, 1997. 192 p.
- Conford E, Twining P. The Dandy-Walker syndrome: the value of antenatal diagnosis // Clinical Radiology. 1992. Vol. 45. P. 172-174.
- Yudina E.V., Medvedev M.V. Perinatal outcomes in congenital malformations. Dandy-Walker syndrome // Ultrasound diagnostics in obstetrics, gynecology and pediatrics. 2000. No. 4. P. 266-271.
- Osenbach RK, Menez,es AH Diagnosis and management of the Dandy-Walker Malformation: 30 years of experience // Pediat. Neurosurg. 1992. Vol. 18. P. 179-189.
- Nyberg D., Mahony B., Hegge F. et al. Enlarged cisterna magna and the Dandy-Walker malformation: factors associated with chromosome anomalies. Obstetrics and Gynecology. 1991. Vol. 77. P. 436-442.
- Congenital malformations: prenatal diagnosis and tactics / Ed. B.M. Petrikovsky, M.V. Medvedeva, E.V. Yudina // M.: RAVUZDPG, Realnoe Vremya, 1999. 254 p.
Treatment options
Unfortunately, it is impossible to completely get rid of this pathology, to eliminate the cause of its occurrence, so treatment will be symptomatic, depending on the existing dysfunction of the internal organs (kidneys, heart, visual organs).
To normalize the outflow of cerebrospinal fluid, surgical intervention is necessary.
Today, the shunt method , when a special shunt connected to the abdominal cavity is inserted in the area of the 4th ventricle of the brain.
Through this shunt, excess fluid will be removed from the brain.
This makes it possible to alleviate the child’s condition, however, such consequences as, for example, mental retardation, unfortunately, cannot be eliminated.
Parents of a sick child must understand that the child’s intellectual abilities will be at a low level of development, and no methods of correctional education will help to fully resolve this problem.