general characteristics
Various convulsive syndromes rank third in terms of overall incidence in the population after cardiovascular pathology and diabetes mellitus.
They account for 20% of all neurological disorders. Pathological symptoms more often occur in children (up to 15 years) and old age. Cramps are felt as involuntary spastic contractions of skeletal muscles - individual muscle groups or the entire body - of varying intensity, short-term or long-term. They arise spontaneously or are provoked by acute pathology or the action of external factors. Severe convulsive twitching of the muscles of the limbs and torso disrupts musculoskeletal function, leading to falls and injuries. Spastic tension is painful, often accompanied by arching or turning of the body, deviation of the head and eyes to one side. Tonic-clonic seizures are manifested by disturbances of consciousness and breathing, urinary incontinence, some are preceded by focal neurological symptoms. Single episodes have a favorable prognosis, but frequent seizures disrupt habitual activity and reduce the patient’s quality of life.
Classification
According to the mechanism of formation, convulsions are classified as rapid hyperkinesis, in the structure of which the phasic component predominates. They are divided into epileptic and non-epileptic, primary (idiopathic) and symptomatic (secondary). Depending on the nature of the predominant involvement of skeletal muscles, there are several types of convulsive contractions:
- Tonic
. Sharp and prolonged (up to several tens of seconds) muscle tension caused by the arrival of a nerve impulse of long duration. Leads to “freezing” of the limbs or body in a forced position. - Clonic
. Muscle spasms are short-term and irregular in nature, with rapid alternation of periods of contraction and relaxation. They have a locomotor effect, accompanied by motor acts. - Mixed
. Convulsive attacks characterized by a change from a tonic component to a clonic one or vice versa are called mixed. In most cases they are generalized (widespread) in nature.
Tonic spasms underlie athetosis; a type of clonic spasms is myoclonus - sudden and sharp (lasting up to a second) contractions of the flexor muscles. Based on the group of muscles affected, cramps can be flexor (flexor), extensor (extensor), or mixed. An important criterion that has found a place in the clinical classification is the prevalence of seizures, which allows us to distinguish two types of paroxysms:
- Partial (focal)
. They arise due to local activity involving a group of motor neurons. Accompanied by clonic or tonic contractions. They can be simple (without loss of consciousness), complex, secondary generalized. - Generalized
. Excitation immediately covers the entire cortex without the presence of an isolated focus, so the muscles of the entire body are involved in a seizure. Paroxysms are clonic, tonic, tonic-clonic. Myoclonic and atonic seizures are also distinguished.
Some conditions combine signs of focal and generalized paroxysms or are of an unspecified nature. In pediatric practice, afebrile and febrile convulsions, neonatal and infantile paroxysms are distinguished. The international classification for some seizures takes into account the prognosis (benign, severe).
How to spot an impending seizure
It is impossible to prevent an epileptic seizure, but you can warn others about it in advance or ask for help if you suffer from epilepsy and feel an attack coming.
First comes the tonic phase, its manifestations are convulsions, loss of control over the situation, increased salivation, etc. As a rule, due to hypertonicity of the muscles, the legs remain straight, and the arms involuntarily bend at the elbows. Breathing becomes difficult and may stop for several seconds at regular intervals. Asphyxia causes the skin to turn blue, especially the lips.
The tonic phase lasts about 30-45 seconds, after which the clonic phase begins. The clonic period is characterized by alternating muscle tension and relaxation - convulsions and convulsive states. During this period, the person twitches randomly, bends in unnatural positions, but does not come to his senses. The patient may spontaneously bite his lips or tongue, which causes blood to appear in the saliva. During the period of complete muscle relaxation, the internal sphincters also weaken, which can cause bowel or bladder emptying.
A few minutes before the onset of epileptic syndrome, the patient may suffer from restlessness, increased anxiety, and may experience hallucinations of various types. There are several types of pre-epileptic conditions, so-called auras:
- speech aura – disturbance of sensory or motor functions;
- mental aura - a sudden, unconditional feeling of sadness, melancholy, increased anxiety, panic attacks, or vice versa, a sharp surge of energy and joy;
- vegetative aura – dysfunction of the executive organs: blood vessels, secretion glands and muscles;
- sensitive aura - distortions in the sensations of external stimuli, a feeling of extreme cold or heat, a disturbance in the sensation of one’s body;
- sensory aura - changes in auditory, olfactory and visual sensations.
It is important not to panic if you notice similar symptoms in yourself or someone nearby. You should calmly warn others about this and secure your location by removing all dangerous piercing or cutting objects, and also move to a safe place where you can lie down.
The round-the-clock reception of doctors at the Yusupov Hospital will protect patients in the clinic from complications after an epileptic seizure. We pay close attention to each of our visitors, guaranteeing high-quality treatment results.
Make an appointment
Why do seizures occur?
Causes of tonic seizures
Prolonged muscle tension occurs against the background of excessive excitability of cerebral structures, in conditions of disruption of the cortical regulation of segmental functions. Very often, neurons are negatively affected by toxic, metabolic factors, and endocrine and metabolic disorders. The causes of tonic seizures are the following conditions:
- Infections
: tetanus, rabies, febrile syndrome. - Electrolyte disturbances
: hypocalcemia, hyperkalemia, hypomagnesemia. - Endocrine disorders
: hyper- and hypoglycemia, hyperinsulinism. - Hereditary metabolic diseases
: amino acid (leucinosis, phenylketonuria), carbohydrate (glycogenosis, galactosemia), lipid (Gaucher disease, Norman-Wood disease). - Cardiovascular pathology
: complete atrioventricular block, acute hypotension. - Renal and liver failure
: uremia, bilirubin encephalopathy. - Psychogenic disorders
: hyperventilation syndrome, hysteria. - Epileptic syndromes of childhood
: Lennox-Gastaut encephalopathy, Otahara encephalopathy, infantile spasms. - Intoxication
: alcohol, carbon monoxide poisoning, strychnine. - Overdose of drugs
: morphine, antipsychotics. - The effect of physical factors
: severe overheating or hypothermia, electrical injuries, the influence of radiation.
Sometimes painful spasms are of a professional nature, occurring during prolonged muscle tension in stenographers, musicians, and milkmaids. Leg cramps are common among athletes and people whose work involves standing for long periods of time. They are often observed during pregnancy, with vascular pathology of the lower extremities - varicose veins, obliterating atherosclerosis, endarteritis.
Causes of clonic seizures
Pathological impulses that provoke short-term spasms of skeletal muscles are formed in higher cortical centers, the extrapyramidal system or peripheral motor neurons. Some clonic seizures develop due to focal damage to the brain stem or spinal cord due to tumors and strokes. Other causes of such seizures include:
- Focal epileptic seizures
. - Children's infections
: measles, chickenpox, influenza, parainfluenza. - Severe myoclonic epilepsy of infancy (Dravet syndrome)
. - Diffuse damage to gray matter
: Creutzfeldt-Jakob disease, subacute sclerosing panencephalitis. - Neurodegenerative conditions
: Tay-Sachs, Alpers diseases. - Non-progressive encephalopathies
: with Down syndrome, tuberous sclerosis. - Neonatal paroxysms
: “fifth day seizures”, benign familial epilepsy. - Poisoning
: drugs (piperazine, ergotamine), chemicals (formaldehyde, arsenic).
Causes of tonic-clonic seizures
Often in the clinical picture there is a change from tonic convulsive contractions to clonic ones. Generalized mixed seizures are a typical sign of epilepsy and its severe complication - epistatus. The occurrence of paroxysmal electrical activity of brain neurons is caused by a wide range of damaging factors:
- Cerebral pathology
: vascular disorders (CVA, arteriovenous malformations, aneurysms), traumatic brain injuries, tumors. - Infectious diseases
: polio, cholera, neuroinfections (meningitis, encephalitis, abscesses). - Arterial hypertension
: renal eclampsia, convulsive form of hypertensive crisis. - Toxicoses of pregnancy
: eclampsia. - Hereditary pathology
: leukodystrophy. - Intoxication
: nicotinic, narcotic (amphetamine, cocaine), poisoning (organophosphorus compounds, oxalic acid, lead). - Overdose of medications
: caffeine, atropine, amitriptyline, etc.
Diagnostics
The initial examination of the patient involves the analysis of anamnestic information (time of onset of the disease, the presence of predisposing factors) and identification of objective signs. But taking into account the polymorphism of the causes of seizures, it is not possible to establish the correct diagnosis using clinical data alone. Therefore, the patient is recommended to undergo a comprehensive examination:
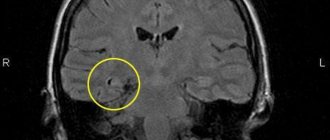
- Tomography
. To identify ischemic-hemorrhagic, inflammatory foci, it is preferable to do an MRI of the brain. CT scan of the head clearly visualizes tumors, injuries and abnormalities of the skull bones, and expansion of the ventricular system. Vascular defects - malformations, thrombotic occlusion, aneurysms - are diagnosed using non-invasive CT or MR angiography of the cerebral arteries. - Electroencephalography
. The study of brain biopotentials makes it possible to identify pathological activity in the form of local or generalized discharges (peaks, sharp waves, spike-wave complexes). Violations are assessed when performing provocative tests - photostimulation, hyperventilation. For better documentation of paroxysms, it is recommended to conduct video-EEG recording with myography. - Lab tests
. The causes of some seizures are established on the basis of a blood test with the determination of biochemical parameters (electrolytes, glucose, renal, liver tests), and a toxicological study. Suspicion of an infectious etiology of epileptiform paroxysms requires serological tests (ELISA, RIF), molecular genetic analysis (PCR). Clinical and bacteriological analysis of cerebrospinal fluid is often performed.
To exclude possible cardiac pathology, an ECG is done; in case of toxicosis of pregnancy, a general urinalysis is prescribed; structural pathology of the kidneys and liver is detected by ultrasound results. Diagnosis of convulsive syndrome is carried out by a neurologist, but based on the expected etiological factors, related specialists may be involved. It is necessary to differentiate primary and symptomatic epileptic seizures, to distinguish them from other paroxysmal conditions - syncope, migraine, tremor, etc.
First aid for seizures
Treatment
At the Neurology Clinic of the Yusupov Hospital, clients can count on several treatment methods. In particular, we are talking about drug therapy and neurosurgical technologies. By skillfully combining these techniques, doctors achieve a significant improvement in the condition of their patients and provide them with the most comfortable life possible with this pathology.
It should be understood that epilepsy is not a death sentence; people with this disease can live a normal life, limiting themselves to virtually nothing. To do this, you need to regularly undergo the necessary examinations, see your doctor and take prescribed medications. Doctors at the Yusupov Hospital take care of their patients, regularly ordering examinations and prescribing medications only based on the individual indicators of each patient.
Treatment of seizures
Help before diagnosis
Regardless of the cause, seizures are an acute condition that requires qualified medical care. Local painful spasms can be eliminated by self-massage, pinching, or stretching the muscle. When a generalized attack develops, it is important to provide first aid to the victim: place a cushion or pillow under the head, turning it on its side, clear the mouth of foam and mucus, and provide access to fresh air. The ambulance team stops the paroxysm with anticonvulsants; in case of high fever in children, antipyretics are administered.
Conservative therapy
Hospitalization is necessary for everyone who has developed a seizure for the first time, with severe and prolonged paroxysms, or with the presence of aggravating pathology. After verification of the diagnosis, along with symptomatic correction, treatment of seizures involves eliminating the causes and influencing the main pathogenetic moments of their development. Based on the clinical situation, the following groups of medications can be used to relieve attacks and treat the underlying disease:
- Anticonvulsants
. Treatment of partial and generalized epileptic seizures is carried out with lamotrigine, carbamazepine - in monotherapy or in combination with other drugs. Convulsive syndrome in organic pathology of the central nervous system can be treated with valproate, clonazepam; in the neonatal period, the drugs of choice are phenobarbital and diphenine. Refractory epistatus requires the administration of anesthesia (sodium thiopental, propofol). - Electrolytes
. Relief of spasmophilia and hyperkalemia is carried out with calcium preparations. Chloroprivate tetany and hyponatremia are treated with sodium chloride infusions; hypomagnesemia is corrected with magnesium sulfate. To eliminate metabolic alkalosis, saline solution and potassium chloride are used. - Hypotensive
. To correct blood pressure during eclampsia, including renal eclampsia, and hypertensive crises, peripheral vasodilators (sodium nitroprusside), beta blockers (esmolol), and ganglion blockers (pentamine, arfonade) are used. Diuretics - osmotic (mannitol, urea), loop (furosemide) - help eliminate concomitant cerebral edema.
In case of poisoning, antidote, detoxification, and infusion therapy are carried out; withdrawal forms of epistatus are treated with a combination of anticonvulsants and antipsychotics. Detection of neuroinfections requires appropriate antimicrobial (antibacterial, antiviral) correction; hypoglycemia is treated with glucose, pyridoxine-dependent seizures with vitamin B6. In some cases, a high-fat ketogenic diet is recommended to relieve seizure symptoms.
Surgery
Drug-resistant variants of epilepsy are an indication for more radical treatment. Among neurosurgical interventions, resections (temporal and extratemporal, hemispherectomy), disconnection operations (subpial transsections, callosotomy), and transcranial stimulating methods are practiced. As a result, it is possible to achieve a complete cessation of attacks within a year or a significant reduction in their frequency with the achievement of adequate control.
Some symptomatic seizures are also treated surgically. In case of traumatic brain injuries and strokes, early intervention is necessary, aimed at evacuation of intracranial hematoma and decompression of cerebral structures. Abscesses and brain tumors also need to be removed. Intravascular recanalization operations - intraarterial thrombolysis, thrombectomy, angioplasty with stenting - are designed to restore blood flow in ischemic areas of brain tissue.
Complications of epilepsy
The following complications are possible with epilepsy:
- status epilepticus of generalized seizures;
- injuries (bruises, fractures);
- increased intracranial pressure: accompanied by bursting headaches, nausea and vomiting, and sometimes confusion;
- cerebral edema (accumulation of fluid inside nerve cells and in the intercellular space): characterized by an increase in neurological symptoms, possible depression of consciousness up to coma;
- ischemic and hemorrhagic stroke: with epilepsy, a violation of the central regulation of vascular tone occurs, blood pressure can sharply increase, which, with predisposing factors (atherosclerosis, aneurysms), leads to depletion of blood flow and ischemic stroke or rupture of the vessel wall and hemorrhage;
- thrombosis of intracranial veins: develops against the background of stagnation of venous blood when vascular regulation is disturbed during an epileptic seizure; in acute inflammation it manifests itself as an ischemic stroke;
- aspiration pneumonia;
- PE (pulmonary embolism) is accompanied by a feeling of lack of air, a sharp increase in breathing, blood pressure drops to low numbers, and death is possible;
- pulmonary edema due to status epilepticus;
- cardiogenic shock;
- renal failure due to cardiogenic shock.
Diagnosis of epilepsy
Diagnostic capabilities are currently very wide; they make it possible to accurately determine whether a patient suffers from epilepsy or whether an attack is a consequence of another disorder. For this, first of all, instrumental examinations , which are crucial in diagnosing and determining the type of seizure.
EEG (electroencephalography) is the main diagnostic method. Patients with epilepsy show changes in their brain wave patterns even when they are not experiencing seizures.
CT and MRI of the brain. The fundamental methods for diagnosing epilepsy are visual diagnostic methods - computed tomography and magnetic resonance imaging. They make it possible to identify the patient’s organic substrate (tumors, cysts, vascular malformations or aneurysms), evaluate its function and structure, and sometimes identify foci of abnormal electrical activity that occur in epilepsy.
An anamnesis of the disease is very important , which allows, based on questioning the patient, to find out the details of the onset and development of the disease, its duration, nature of the course, and the presence of a hereditary predisposition to epilepsy. It is extremely important to describe the paroxysms themselves, their frequency, description, and the presence of factors contributing to the occurrence of attacks. Such questioning allows the doctor to determine the type of seizure and also suggest which area of the brain may be affected.
It should be understood that the appearance of a single convulsive attack, although it is an alarming symptom, does not always indicate the presence of epilepsy. The doctor has the right to consider this diagnosis if the patient has had two or more attacks.
Epilepsy and television, computer technology
Epilepsy is known to be a brain disease that causes repeated, unprovoked seizures. An exception to this rule are reflex forms of epilepsy that arise as a result of provoking factors. The most common type of reflex form is photosensitive epilepsy. This disease usually debuts in adolescence, with a predominance in girls. In approximately 50% of patients in this group, seizures occur only in response to rhythmic light stimulation. The most dangerous frequency for humans is 15-20 flashes per second.
Provoking factors can be any type of intermittent rhythmic light stimulation in everyday life: watching television (especially light shows and “shooter” cartoons); computer monitor screen (mainly video games); color music at discos; cycling along linearly planted trees; observing the flickering of telegraph poles or a light source through a window in a vehicle (especially at night and at high speed); observing the sun's glare on the water; flickering headlights of passing vehicles while driving in a car. These are just the most common factors; in fact, there are many more of them.
A special type of photosensitivity form is television (or computer, which is essentially the same thing) epilepsy, in which seizures are provoked mainly by watching television or playing computer games. Seizures can occur during computer games or when using game consoles. There are even terms such as “computer game epilepsy” and “star wars epilepsy”. Such attacks occur between the ages of 7 and 17 years and are usually provoked by prolonged viewing of television programs with flashing images (for example, cartoons) in a dimly lit room. Seizures more often occur when viewing images in black and white, and when the distance to the TV screen is less than 2 m. Seizures may occur only when approaching the TV screen when switching TV channels. Some patients experience a unique phenomenon of “forced attraction to the television screen.” At the same time, before the onset of attacks, they begin to peer intently at the television screen, which gradually occupies the entire field of vision. There is a feeling of being unable to take your eyes off the TV screen and a violent attraction to it. Patients slowly approach the TV, sometimes coming close, then loss of consciousness and generalized tonic-clonic convulsions occur.
Treatment of patients with photosensitivity epilepsy is extremely difficult. In addition to the use of basic antiepileptic drugs, compliance with a number of regime measures is mandatory. First of all, factors of rhythmic light stimulation in everyday life should be avoided. If this is not possible, then the easiest way to avoid an attack is to cover one eye with your hand. Using polarized sunglasses, preferably blue, can also help. Preventative measures regarding television viewing include:
- Increasing the distance between the patient and the television screen by more than 2 m.
- Use of additional TV screen lighting installed near the TV and sufficient general lighting of the room.
- Prohibition of watching programs if the TV is faulty or the program settings are unclear (flickering images).
- Covering one eye with your hand when you need to move closer to the TV screen or when changing channels.
- The most optimal are modern 100 Hz color TVs with remote control, as well as LCD computer monitors. For patients suffering from all other forms of epilepsy, except photosensitivity, watching television and working on a computer are not contraindicated, and the duration should be determined by general hygienic standards for children of this age.
Epilepsy and lifestyle
It should be remembered that patients with epilepsy are ordinary normal people who are no different from other people, especially in the period between attacks.
Most children (about 90%) with epilepsy can attend regular schools and kindergartens. It is recommended to inform the staff about the child’s illness in order to enable them to act correctly if attacks occur. There is no need to restrict children from additional classes in a foreign language, music, etc. In most cases, attacks occur during a period of passive, relaxed state, drowsiness. At the same time, mental activity helps to reduce epileptic activity. The leading American epileptologist V. Lennox said that “activity is the antagonist of seizures.” Only a small number of children and adolescents (approximately 10%) have additional severe disorders of the nervous system: motor (cerebral palsy) or mental (mental retardation, psychosis). These children should attend kindergartens and schools with an individual approach and adapted programs. The most severe patients should be trained in special educational centers at home
In general, we can say that children suffering from epilepsy should try to lead a normal lifestyle. It should be taken into account that parental overprotection leads to the isolation of children in society and their poor social adaptation. Children should definitely play sports, as it has been found that active physical activity has a positive effect on the course of epilepsy. Playing sports has a beneficial effect on self-esteem and reduces the level of isolation of children from society. As with people without epilepsy, the healthiest option is regular exercise (exercise). A child with epilepsy should be included in all types of school activities, except for potentially dangerous types of physical education (for example, swimming or participation in certain competitions). When choosing a sport, it is necessary, in addition to personal preference, to also be guided by the fact that the risk of acquiring various injuries is minimal. Each sport contains certain dangers that should be analyzed jointly by the doctor and the patient's family. Tennis, badminton, and some team sports are optimal. Swimming is contraindicated due to the risk of an attack in water.
If you have uncontrolled seizures with impaired consciousness, you must follow simple safety rules, the purpose of which is to minimize the likelihood of injury during an attack: do not be at a height, at the edge of a platform, or near bodies of water. When riding a bicycle, the child must wear a helmet, and rides must take place on roads without cars (dirt roads outside the city). In photosensitive forms of epilepsy, rhythmic flickering of light should be avoided: watching television, computer games, ripples on the surface of reservoirs, flickering headlights of passing vehicles, etc. In all other forms of epilepsy, watching television and working on a computer is possible subject to generally accepted hygienic standards.
For patients suffering from epilepsy, activities related to driving a car, as well as service in the police, fire departments, and guarding important facilities are contraindicated. Working with moving machinery, chemicals, or near water bodies may pose a potential danger to patients. With a shift work schedule, the patient must have the opportunity to get adequate sleep and take medications in accordance with the doctor’s prescriptions. Lack of sleep is especially dangerous for children and teenagers who have seizures immediately after waking up.
In general, a patient's ability to perform activities is influenced by the type of epilepsy, the nature of the seizures, the severity of the disease, the presence of concomitant physical or intellectual impairments, and the degree to which seizures are controlled by antiepileptic drugs.
Recommendations
Recommendations that can help you cope with daily problems and make your life more comfortable.
Believe me, the tips given here can be useful even for people who do not have epileptic seizures. Use them according to the type of seizure or problem you are having.
In bathroom:
- Doors must open outwards, do not lock them (place an occupied sign on the door).
- It is safer to take a shower rather than a bath.
- Sing while in the shower to let your family know you are okay.
- Wash with warm water (avoid too hot water).
- Every time, check whether the drainage and ventilation systems in the bathroom work.
- Patients suffering from frequent epileptic seizures should take additional safety measures while taking a bath (special surfaces, chairs with belts, etc.).
- Do not use electrical appliances (hair dryer, electric lift) in the bathroom or near water.
In the kitchen:
- If possible, cook in the presence of other members of your family.
- Use plastic plates, mugs and glasses.
- Wear rubber gloves when using a knife or when washing dishes.
- Avoid frequent use of sharp knives (if possible, use already cut or prepared foods).
- Use the microwave whenever possible.
At work:
- Inform your colleagues about the possibility of an epileptic seizure and tell them how they can help you (show them how to put you on the pillow, who to call, etc.).
- Avoid stressful and overtime work.
- Wear protective clothing depending on the type of seizure you have and the work you do.
- Keep spare clothes in your office so you can change if necessary.
At home:
- Cover the floor and furniture with soft materials.
- Cover furniture with sharp edges or buy furniture with rounded edges.
- Place protection around open flames, heaters and radiators.
- Avoid smoking and lighting fires when you are alone.
- Do not carry lighted candles, hot dishes or food.
- Avoid heaters that may tip over.
- Use irons and other electrical appliances with care, especially those with a safety circuit breaker.
- Try not to climb on chairs or ladders, especially if there is no one at home except you.
How to behave if your loved one has a seizure?
Most epileptic seizures are limited in time and stop spontaneously after 2-5 minutes without any special treatment.
When an attack occurs for the first time, in all cases it is necessary to urgently consult a neurologist or epileptologist.
Help for a patient with epilepsy depends on the type of attack and its duration. Patients suffering from generalized tonic-clonic seizures often need help. While most people with “minor” seizures (absences) do not need any special intervention. It is important to know the situations in which it is necessary to resort to qualified medical assistance. These may be the following cases:
- an epileptic attack occurred for the first time in life;
- there are doubts that this is an epileptic attack;
- the duration of the attack is more than 5 minutes;
- the patient has respiratory dysfunction;
- regaining consciousness after an attack is too slow;
- the next attack occurred immediately after the previous one (serial attacks);
- an epileptic attack occurred in the water;
- the attack occurred in a pregnant woman;
- The patient was injured during an epileptic attack.
Situations in which immediate medical attention is not necessary:
- if the epileptic attack lasts no more than 5 minutes;
- if the patient regains consciousness and a new attack does not begin;
- if the patient did not injure himself during an epileptic attack.
It is necessary to be able to provide first aid in the event of a generalized tonic-clonic seizure.
The following activities are recommended:
- Remove all objects located in the immediate vicinity of the patient that could harm him during an epileptic attack (iron, glass, etc.).
- Place a soft, flat object (pillow, bag, package) under your head.
- Unbutton your clothes or untie your tie, or loosen your waist belt.
- Until the convulsions stop, move the person to a lateral position (fix the legs straight and the arms lying along the body).
- Do not put any objects in the mouth (spatula, spoon, etc.), and do not attempt to open the patient’s jaws.
- Do not put any liquid into the mouth until the patient has fully regained consciousness.
- It is not recommended to restrain patients during an epileptic attack.
- If the attack happened to a stranger, look in his things for documents confirming a possible illness or an identification bracelet.
- Record the time of onset of the epileptic seizure to determine its duration.
- Always wait at the scene until the patient regains consciousness.
- If necessary, call emergency medical services.
If an epileptic attack occurs in water, the patient must be held in such a way that his head is constantly on the surface of the water. It is necessary to pull the person out of the water while continuing to support his head on the surface. After you have pulled the patient out of the water, it is necessary to examine him and, in case of airway obstruction, immediately begin resuscitation (mouth-to-mouth artificial respiration in combination with chest compressions). Even though the condition of a person who has an epileptic attack under such circumstances is satisfactory, it is necessary to send him to the nearest medical facility for a thorough examination.
In the event of an epileptic attack in transport, it is necessary to vacate the nearest seats and bring the patient into a lateral position. It is also very important to ensure that he can breathe freely. If the seat is adjustable, then it is moved to a supine position until the end of the attack, and the patient himself turns over to the side position to ensure free breathing. It is recommended to cover nearby hard surfaces with pillows, blankets, clothing or bags to avoid injury during a generalized attack.
Drug treatment of epilepsy
Principles of drug treatment for epilepsy:
- the main drugs for treating the disease are anticonvulsants;
- it is necessary to choose the right dosage and regimen - only a specialist doctor can do this;
- when choosing a drug, you need to take into account the type, frequency and time of occurrence of attacks;
- the absence of convulsive seizures does not mean that recovery has occurred - in no case should you stop taking the drug yourself or take breaks without the knowledge of the doctor;
- the doctor controls the healing process not only by external symptoms, but also by the electroencephalogram;
- the dose of drugs can be reduced only if attacks have not recurred for 2 years;
- complete withdrawal of the drug is usually possible only after 5 years, with a complete absence of attacks during this entire time and normalization of the electroencephalogram, the decision to cancel is made only by the attending physician;
- The ultimate goal of drug treatment for epilepsy is to achieve complete recovery with drug withdrawal.