Constant headaches are a common reason for patients to turn to neurologists at the Yusupov Hospital. People experience headaches in the evening, in the morning after sleep, which do not go away after taking painkillers, and at night. Frequent headaches in men can occur in the presence of pathology of cerebral vessels or brain tumors.
Persistent headache is an indication for a comprehensive examination of the patient. Neurologists conduct instrumental analyzes using the latest equipment from leading global manufacturers. Analyzes are performed by experienced laboratory technicians. Patients are advised by candidates and doctors of medical sciences. Leading specialists in the field of headache treatment collectively develop tactics for managing patients whose headache does not go away for several days.
Non-pathological causes of daily headaches
Brain activity is disrupted due to minor disturbances in blood supply, metabolism, and innervation. Night headaches occur for the following reasons:
- lack of oxygen;
- high temperature in the bedroom;
- drinking alcohol in the evening;
- overwork.
Healthy sleep depends on bedding and posture. On a high pillow, the cervical spine bends strongly. Even in the absence of discomfort during sleep, muscle tension occurs and cerebral blood flow is disrupted. Sleeping without a pillow can also cause pain in the head and neck. Low-quality fabric dyes and softeners used to wash bed linen often contain harmful ingredients that cause breathing problems and headaches in the morning.
Experiences and intense mental activity in the evening lead to brain overstrain. At night he cannot switch off. The patient cannot sleep and often wakes up. After waking up, you feel discomfort, pain in the head, and fatigue. He gets morning headaches.
How does melatonin affect sleep?
The human body works according to natural biorhythms, which are called circadian. They are associated with the time of day, just like the production of certain hormones. It’s not for nothing that our ancestors got up at sunrise without any alarm clocks, but they also went to bed at sunset. Nowadays, people who call themselves “night owls” go to bed after midnight, and then wonder why in the morning after sleep they have a headache and absolutely no feeling of vigor.
To understand this issue, it is important to understand how melatonin is produced. The pineal gland is responsible for the sleep hormone, and the production of the substance is possible only in complete darkness. During the night, the pineal gland generates approximately 70% of the daily norm of melatonin, peak production occurs between 23.00 and 3.00.
When light stops reaching the retina, the brain sends a signal to produce melatonin. The hormone is gradually absorbed into the blood and distributed to all cells of the body. The body temperature decreases, the person begins to fall asleep.
By 2-3 am, melatonin production decreases. At the same time, the adrenal glands begin to produce cortisol, a hormone that excites the nervous system. By 6-7 o'clock in the morning its concentration in the blood becomes maximum, i.e. Nature intended that it is at this time that a person wakes up. And if this does not happen, cortisol turns into a stress hormone. That is why early rise and morning exercises are considered one of the best ways to combat nervous tension.
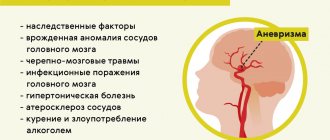
Pathological causes of headaches
A common cause of nighttime headaches is oxygen deficiency. It may be caused by abnormalities of the nasal passages and respiratory tract diseases. Night headaches occur after sleep apnea.
Blood supply to the brain is impaired during hypotension. The outflow of venous blood worsens due to a decrease in the tone of the intracranial veins. In the morning the patient feels it in his head.
With arterial hypertension, blood pressure may increase during sleep. The reason is the patient’s age, disruption of sleep and rest patterns. Vascular tone is impaired in diseases of the thyroid gland and heart. Nocturnal hypertension is dangerous for the development of heart failure and stroke. Headache occurs at night or in the morning.
Stress, anxiety, and mental trauma affect the central nervous system and change vascular tone. This provokes an increase in blood pressure and irritation of pain receptors in the walls of blood vessels. Night headaches that occur under the influence of psychogenic factors are varied in nature. They are accompanied by irritability, rapid heartbeat and are not relieved by analgesics.
Diseases of the cervical spine and temporomandibular joint can provoke night headaches. With back pain, a person is forced to take an uncomfortable position, which causes spasms of the neck muscles. They cause headaches.
Failure to comply with the dosage of glucose-lowering medications or refusal to eat dinner in diabetes mellitus results in a sharp decrease in blood glucose levels and severe headaches. Histamine disease is characterized by prolonged attacks of acute headache in the orbital area in the evening and at night.
In the presence of brain tumors, patients complain of night and morning headaches. As the disease progresses, it intensifies. The head hurts when changing position, the patient's hands go numb.
Throbbing morning headaches are felt during migraines. They often intensify when the light is turned on and are accompanied by nausea and vomiting. Constant headaches that bother the patient night and day are characteristic of brain infections.
Expert opinion
Experts believe the findings could be useful in research into Alzheimer's disease, as many patients with the disease suffer from interrupted sleep, meaning their nervous system does not rest at night.
Naturally, in order for the brain to be active during the day, it needs to rest and recover at night. When going on night shifts, this balance changes and goes against the biological clock. That is, during that period of the day when the nervous system should rest, a person is busy with work, it does not rest and does not recover. Research has shown that those who work nights or longer hours have a higher risk of potentially serious illnesses, including some forms of cancer and obesity.
Researchers from Swansea University and the University of Toulouse have also found that night shifts can have a negative impact on both mental abilities and the health of the body as a whole.
Three thousand people participated in this study. The subjects underwent studies of memory and speed of thinking. The results showed that people who worked shifts for at least ten years had the same brain age as those who were on average 6.5 years older than them but did not work nights or around the clock. It was also found that even after dismissal from shift work (night shift), it takes about 5 years to restore normal functioning.
© 2014 Author of the text translation: neurologist, Titarchuk A.B.
Any copying of text and posting it on other sites should only be done with a link to the source site.
Cluster headaches
Attacks of cluster (bundle) headaches occur in paroxysms and are difficult for patients to tolerate. The pain has the following characteristics:
- localized in the eye area;
- radiates to the forehead, temple, cheek;
- accompanied by lacrimation, sweating of the forehead, a rush of blood to the face;
- more acutely felt when the patient is lying down;
- starts and goes away suddenly.
Night headaches begin without cause between 9:00 p.m. and 9:00 a.m. The peak of pain occurs at night, from zero to three o'clock. Attacks occur cyclically, followed by painless periods. Attacks are observed mainly in men. Pain occurs after drinking alcohol.
Men whose relatives suffer from cluster pain are at risk. The risk of developing a painful attack increases with head injuries, migraines, sleep disorders, mental and physical stress. Neurologists include possible causes of cluster headaches:
- abnormalities of the hypothalamus;
- pathology of blood vessels;
- disruption of circadian rhythms.
Patients relieve an acute attack at home with lidocaine drops in the nose. For symptomatic therapy, neurologists prescribe special medications and oxygen inhalations. In difficult cases, electrical stimulation of the brain is performed and the nerves that cause pain are removed. During the cluster period, doctors recommend giving up alcohol and nicotine.
Sleep disorders
Sleep disorders are diverse. They occur very often. Thus, in France, a national program to combat insomnia was adopted in 2006, as it turned out that a third of the French suffer from serious sleep disorders. Sleep disorders occur in various mental and somatic diseases. It is important to note that dissomnia is often one of the earliest signs of a mental disorder. Normalization of sleep, in turn, usually characterizes the state of recovery. Let us describe currently known sleep disorders.
Hypersomnia is an increased need for sleep and an increase in daily sleep norms that are not subject to conscious control. The duration of sleep increases to 15–16 hours a day or more, and the disturbance can last for several weeks and months. Increased activity in the waking state, as well as a feeling of satisfaction from sleep, usually does not occur with hypersomnia. Hypersomnia may be followed by periods of shortened night sleep. There is practically no information in the literature about the structure of sleep in hypersomnia, especially considering that it is observed in various diseases and painful conditions.
It should be emphasized that the important fact is that hypersomnia is not a state of somnolence observed in epilepsy after seizures, vegetative-vascular paroxysms, hypoglycemia, encephalitis, meningoencephalitis, acute intoxication, as some authors do (Vein, 1974, etc.). In psychiatric practice, hypersomnia is especially common in states of apathy, anergy, asthenia and mild depression. The number of dreams does not increase; on the contrary, it decreases significantly. Some patients develop something of a sleep addiction: they would like to sleep more if they do not experience unpleasant sensations while sleeping. For example, this disorder occurs in depression. An increased need for sleep may be accompanied by a shortening of daily sleep norms. Such patients constantly feel a drowsy state with a desire to fall asleep, but they cannot fall asleep for a long time, which is why they resort to taking sleeping pills.
Short-term states of hypersomnia, characterized by short episodes of excessive sleepiness and subsequent disturbances of various kinds, often occur. Thus, the patient reports: “If I feel unusually strong sleepiness, I already know that something is wrong with me. I fall asleep quickly, but only for a short time. Then I suddenly wake up and at this time I feel as if I am falling somewhere, flying away somewhere. At the same time, I feel as if something is in the way in my hands, my heart turns over and begins to pound rapidly. The next morning after this, I get up broken, with a headache, my head hurts somewhere inside, in the depths.”
Narcolepsy - attacks of irresistible drowsiness with immersion in short-term sleep, lasting up to 20-30 minutes. It was first described within the framework of Gelineau's syndrome (1880). In its complete form, this syndrome, in addition to sleep attacks, includes attacks of cataplexy, states of sleep paralysis, disturbances of nighttime sleep and daytime sleepiness. The disorder most often appears before the age of 30. Then it progresses or flows stationary.
Along with essential narcolepsy associated with the influence of genetic factors, various variants of symptomatic narcolepsy are described that occur in diseases such as meningoencephalitis, brain tumors, the gummous form of cerebral syphilis, and vascular damage to the diencephalic region of the brain. Narcoleptic sleep is MDH sleep. Narcolepsy not associated with MDH sleep has also been described. This disorder is characterized by periodic sleepiness during the daytime, but no sleep attacks are observed. Apparently, epileptic seizures occur in the form of sleep attacks. Due to sleep attacks, narcolepsy can lead to such adverse consequences as car accidents, falls from heights, burns, frostbite, and drowning. We will describe the following symptoms of narcolepsy: sleep attacks, cataplexy attacks, sleep paralysis states, night sleep disorders, concomitant disorders.
a) Sleep attacks occur suddenly and autochthonously, that is, without the influence of any external causes. They begin with the appearance of a growing and irresistible need to sleep, so that patients fall asleep within a few seconds or a matter of minutes. They can fall asleep in any circumstances. Sleep attacks occur only during the daytime. There can be up to 3–5 or more of them per day. They can occur daily and occur at the same time. At the beginning of the attack, a pattern of MDH sleep is revealed, and at the height of the attack, REM sleep is revealed. It is very difficult or impossible to awaken patients, since the threshold for perceiving external stimuli increases sharply. Patients fall asleep with a feeling of rapidly falling into sleep, and sometimes wake up with the feeling that they have woken up, and not woken up, as happens with normal awakening. The pupils, if this is not an epileptic attack, are constricted. There are no cramps, muscle tone is reduced, and there is no loss of urine, feces, or semen. There are no dreams.
b) Attacks of cataplexy are usually provoked by emotions, both positive and negative (fun, fear, etc.). There is a sharp and significant drop in the tone of all voluntary muscles or only in individual muscle groups, sometimes different from attack to attack. At the same time, patients may fall as if knocked down, like a “sheaf,” or lose objects from their hands, cannot speak, their jaw suddenly drops, their head falls, etc. Consciousness is not impaired, and there is no drowsiness. During prolonged attacks, lasting up to half an hour, drowsiness may occur; however, patients do not fall asleep. This reveals the pattern of MDH sleep.
c) Conditions of sleep paralysis are observed during falling asleep, as well as upon awakening from sleep. More often, perhaps, they arise upon awakening. Apparently, they are confined to the first and second phases of slow-wave sleep. As a rule, there is no feeling of sleep; patients feel as if they are not yet asleep or have already woken up. Actually, dreams do not occur at this time. Patients are partially aware of external impressions, understand where they are, autopsychic orientation is not impaired. The most characteristic disorder is a feeling of complete motor numbness.
Patients report that they cannot perform even simple voluntary movements, for example, they are unable to open their eyes, mouth, raise their voice, raise their hand, move their fingers, etc. At the same time, they make extraordinary and unsuccessful efforts to perform some kind of activity. that movement. During repeated attacks, the painfulness of the condition is often realized. A feeling of helplessness appears, and the need for outside help arises. The patient says, for example, that he tries to call someone for help so that he can be “pushed away.” The duration of states of sleep paralysis does not exceed a few seconds, however, there is often a disturbance in the perception of the sense of time, so that, according to patients, up to 10–15 minutes pass until the moment of final awakening from sleep.
Hypnagogic or hypnopompic delusions of perception almost always occur, especially auditory, tactile and visual hallucinations. An acute feeling of fear and a feeling of an alien physical presence are often experienced. Perceptual deceptions are not identified by dream patients. In many patients, a critical attitude towards hallucinations does not appear immediately even after awakening. Having finally woken up, some patients experience palpitations, difficulty breathing, and trembling in the body. Some of them have a fear of repeating states of paralysis.
Let’s give one observation: “Starting at the age of 18 and for more than 15 years, almost every morning before waking up, it seems to me that a brownie is crushing me. I'm scared, it's hard to breathe, I'm suffocating. I know that the brownie needs to be asked whether this is for good or for bad. If it's good, it should get hot, and if it's bad, then a cold breeze should blow. But no matter how hard I try, I can’t say anything, I can’t open my eyes, I can’t even move a finger. I feel that all this is happening in reality, I am no longer sleeping and I am not dreaming of anything. I hear my mother walking around the room or talking to someone. Some time passes until I finally manage to open my mouth or move my arm or leg. The stiffness immediately goes away after this. It lasts a very long time, 5–10 minutes. Then I finally come to my senses. Previously, I didn’t believe in any brownies, but now I think they exist.” Sleep paralysis can also occur during daytime sleep.
d) Night sleep disturbances are manifested by too rapid or, on the contrary, delayed falling asleep. Sleep can be superficial and interrupted by night awakenings, both spontaneous and associated with some kind of external interference. As a rule, night sleep does not bring rest and satisfaction; it is also filled with unpleasant dreams and nightmares. When falling asleep and waking up, deceptions of perception and episodes of oneirism may occur.
e) Various associated disorders are also observed. During the daytime, patients report lethargy and drowsiness. Mental asthenia, irritability, torpidity of mental processes, and apathy are often detected. Disorders such as subdepression, sexual problems, menstrual disorders, obesity, and hyperthyroidism are also possible. Metabolic disorders, loss of appetite, loss of performance, and phenomena of autonomic dysfunction are also often detected.
In its expanded form, Gelineau syndrome is quite rare. Much more often and in various painful conditions, its individual components are observed, especially the state of sleep paralysis.
Pickwickian syndrome (J.Elliot, 1781) is manifested by disorders of consciousness (stunning) or involuntary attacks of daytime sleep in combination with myoclonic hyperkinesis. The disorder is caused by hypoventilation of the lungs due to pathologies such as obesity, certain lung diseases, rapid or shallow breathing. Patients usually fall asleep in a sitting position. Hyperkinesis that occurs during sleep can cause patients to fall. In addition, the “Pickwickian personality type” is considered characteristic: good nature, optimism, sociability, sufficient physical and mental activity, practicality and success, as well as excess in food. The hereditary nature of the disorder is assumed (autosomal recessive inheritance). The name of the disorder is borrowed from Charles Dickens's novel The Pickwick Papers, one of whose characters, servant Joe, suffered from this disorder.
Kline-Levin syndrome (1925, 1936) is characterized by alternating periods of hypersomnia and normal sleep-wake cycles. This happens one or more times a year. During periods of hypersomnia, which last up to several weeks, the daily sleep rate increases and reaches 15–16 hours or more. During such sleep, patients can be awakened, but at the first opportunity they fall asleep again. There are no dreams.
Sleep does not provide a feeling of rest. Bulimia often occurs at the beginning of the period of hypersomnia and after it ends. While awake during the period of hypersomnia, other disorders may occur: apathy, irritability, depression, aggressiveness, hypersexuality. Sometimes delusions and hallucinations, confusion, psychomotor agitation and incoherent speech also occur. Some patients develop fever of central origin. The disorder usually begins in childhood and adolescence and is more common in boys. Remissions of varying durations are possible. In rare cases, it is complicated by narcolepsy. The nature of the disorder has not been established.
Hysterical hypersomnia is manifested by states that are externally similar to deep sleep and occur in connection with traumatic situations. During painful episodes, muscle hypertonicity, delayed urination and defecation, analgesia of the skin and mucous membranes with various configurations are detected. The EEG records a picture of wakefulness, which most likely indicates the fact of a dissociative disorder of consciousness. Subjectively, it is sometimes experienced not as an attack of drowsiness, but as a memory loss. Let us present an observation that meets the mentioned criteria. The patient reports that she recently received news that her boyfriend is cheating on her with her friend. She was shocked by this news and decided to talk to her friend. After an explanation with her, as the patient says, “I felt better and at the same time even more painful.” Returning home, she immediately went to bed without undressing. “I immediately forgot. When I came to my senses in the morning, my first thought was “it’s good that I didn’t die.” There was no feeling that I fell asleep, slept and woke up. I didn't dream of anything that night. It seemed to me that I had simply forgotten everything that had happened the day before. After that, I rarely remembered the betrayal, calmly, as if nothing special had happened. I slept off troubles in the same way before.”
Another variant of the dissociative reaction to stress is hysterical stupor. At the same time, patients freeze in an expressive pose depicting suffering. There seems to be no normal sleep at night. In the waking state, consciousness is narrowed, this can be judged by the fact that many questions, including those related to well-being, as well as changes in the situation, are not accompanied by responses; patients’ requests are ignored. Nevertheless, contact with the outside world is not completely interrupted. Understanding of the speech of others is preserved. Muscle tone is slightly increased.
When reminded of a traumatic situation, psychologically adequate and understandable facial and vegetative reactions arise: tears appear, patients may blush, turn pale, close or open their eyes, and clench their teeth. The state of stupor lasts from several hours to a number of days. Signs of hysterical psychosis (Ganzer syndrome, etc.) are not observed either at the beginning or at the end of the painful condition. The exit from the latter is critical, after which dissociative amnesia is revealed. Another, much milder form of hysterical stupor is the state of hysterical mutism, which occurs with clear consciousness and without subsequent amnesia.
Hypersomnia with sleep apnea is associated with impaired respiratory function during sleep. Usually more common in elderly and obese patients. Sleep apnea is defined as stopping breathing for 10 seconds or more. With pure apnea (i.e. apnea of central origin), respiratory movements are completely interrupted. With pure obstructive apnea, respiratory movements, on the contrary, increase, but the flow of air into the lungs stops for mechanical reasons. Sometimes both of these forms of the disorder are combined. Pathology is considered to be five or more episodes of apnea per hour or 30 or more episodes during the night. Patients may not have complaints about sleep disorders.
This apparently indicates that the structure of sleep in some cases is significantly disturbed, which is why sleep during breathing stops turns into a state of somnolence. Normal night sleep is practically non-existent. After breathing stops, its activation begins with loud intermittent snoring followed by convulsive breathing. In addition to the mentioned signs of the disorder, headaches in the morning, increased fatigue, a tendency to depression, fluctuations in blood pressure and cardiac arrhythmia are also observed. Sleep apnea can have extremely dangerous consequences, including death from pulmonary and cardiovascular failure, as well as death from other, as yet unknown causes. There is evidence that sleep apnea is associated with crib death syndrome or nursing death in infants and children. Some authors tend to identify sleep apnea with Pickwickian syndrome. While awake, patients with sleep apnea may also experience sleep attacks, suggesting a possible connection with narcolepsy.
Alveolar hyperventilation syndrome is characterized by disturbances in pulmonary ventilation and external respiration function. It is believed that the disorder is associated with insufficient blood flow to the lungs, as well as decreased breathing during sleep. In some cases, patients experience insomnia or, more precisely, a sharp reduction in sleep norms, but much more often they experience excessive drowsiness. Death may occur during sleep.
Insomnia is manifested by an absolute lack of sleep for a long time. Insomnia in this understanding occurs in psychiatric patients in acute psychotic states. A complete lack of sleep is usually short-lived and rarely lasts more than a week.
Sleep deficiency syndrome is much more common The disorder is manifested by the following symptoms:
- decreased need for sleep;
- difficulty falling asleep;
- night awakenings;
- early morning awakenings;
- decreased sleep quality, apparently associated with disturbances in its structure; such a dream usually does not bring rest.
The result of this is a significant reduction in sleep time at night. If previously some patients could at least partially compensate for the lack of night sleep by resting and sleeping during the day, then with the onset of insomnia, daytime sleep may disappear. The causes of sleep deficiency are varied.
With great consistency, this disorder occurs in the prodromal period of acutely emerging and rapidly occurring psychoses. With rare exceptions, it is observed in states of melancholic and anxious depression, especially if anxiety and fears intensify or appear closer to the night, and drowsiness disappears or even a rise in mood and activity occurs. As a rule, the norm of daily sleep is sharply reduced in manic states of various types, in the acute period of post-stress disorder, in a state of alcohol and drug withdrawal. Persistent sleep disturbances occur in chronic pain syndrome, psychotic states with delusional, hallucinatory and catatonic psychomotor agitation.
A significant reduction in daily sleep norms is also observed outside of psychotic conditions, for example, due to overwork, inability to relax, influxes of thoughts, excessive fears of insomnia and attempts to lull oneself to sleep in one way or another (by counting, for example), fear of dying in sleep, fear of repetition of nightmares, conditions sleep paralysis and other sleep-related disorders.
Very often, sleep is disturbed due to anxiety about what happened the day before or what is to come the next day, anticipation of recurring panic attacks at night, vegetosomatic crises, worsening pain and senestopathies. Children, adolescents and even adult patients often cannot fall asleep for a long time due to fear of the dark and frightening fantasies. Some patients report interference with the onset of sleep, such as myoclonus or fibrillary muscle twitches that occur at the very beginning of sleep. There are patients who, for various reasons, fall asleep only in the morning.
Quite common causes of difficulty falling asleep are frequent flights to other time zones, long-term work at night (on duty, emergency situations, military operations), living in northern latitudes in conditions of the polar night changing to polar day, changing time from winter to summer and vice versa.
Night awakenings can occur for various reasons: frequent night urination, snoring of other people, extraneous sounds, lighting, fear of oversleeping at the right time of awakening, nightmares, after which patients wake up in fear or wake themselves up. Some researchers have linked nighttime awakenings during MDH sleep to an activation response that protects patients from nightmares.
Nighttime awakenings are observed most consistently in depression. In this case, patients wake up suddenly, sharply, without any external reasons, sometimes at the same time of the night. Such awakenings can occur both in the first and second half of the night. Patients often report that they wake up feeling as if they have already had enough sleep and they no longer want to sleep. Others report waking up anxious, sad or afraid, with a feeling of heart palpitations, or sweating. Nighttime intervals of wakefulness can last up to half an hour or more, and some patients no longer manage to fall asleep. The number of spontaneous night awakenings sometimes reaches 4–5 or more.
Early awakening from sleep is common in elderly patients, as well as in a significant number of depressed patients. Patients wake up 1–3 hours or more earlier than usual, as if missing 1–2 sleep cycles with the longest time of paradoxical sleep.
In cases of absolute and forced insomnia, psychotic disorders may develop after a few days.
Back to contents
Diagnosis of headache
Neurologists at the Yusupov Hospital determine the cause and type of persistent headache based on data from a clinical examination of the patient, instrumental and laboratory research methods. Doctors at the Neurology Clinic prescribe the following diagnostic procedures:
- Doppler ultrasound of head and neck vessels;
- electromyography;
- electrocardiography;
- diagnostic spinal puncture (if a neuroinfection is suspected).
Computed tomography and magnetic resonance imaging are performed if a brain mass is suspected. To determine the condition of the cerebral vessels, contrast angiography or multislice tomography is performed.
Migraine
Migraine is a throbbing, sharp pain that ranges in intensity from moderate to unbearable. As a rule, attacks occur in the morning, but nighttime manifestations are also possible. Migraine affects one half of the brain, lasts up to 3 days and is accompanied by the following symptoms:
- nausea and vomiting;
- photophobia;
- aphasia;
- noise intolerance.
There are many reasons for migraines: hormonal imbalance, poor diet, insomnia, stress, and heredity. In people prone to migraines, attacks occur more frequently over time; The result of the disease may be permanent damage to the central nervous system.
Classification of headaches
Classification of headaches by attack location.
Nighttime headaches can be classified according to two main characteristics: the frequency and duration of attacks and the location.
By time of attack
Pain of different etiologies has a different character:
- common - occurs with problems with blood vessels in the brain;
- paroxysmal - with increased blood pressure, migraine, cancer;
- repeated - for neuritis of the cranial nerves.
However, a more striking diagnostic sign that helps to quickly determine the cause of pain is the localization of the syndrome.
By location of pain
Pain can affect any part of the brain. On this basis, it is divided into the following types:
- Unilateral - occurs with migraine.
- Cluster - in the front of the head. Lasts up to an hour. More common in men. Complemented by cold symptoms, often accompanies infectious diseases.
- Tension - compressive.
- Temporal. Occurs when the temporal arteries are damaged. The pain intensifies due to depression, overwork, sleep disturbances, and rapid weight loss. Accompanied by discomfort in the neck area.
Some types of pain (organic - due to injuries and other damage to the nervous tissue, hypochondriacal - without a real cause) can be localized throughout the head. The pain syndrome caused by tumors is localized where the tumor has developed.
Treatment of pain syndrome
In most cases, the simplest analgesics - Ibuprofen or Citramon (Citramon increases blood pressure) help with night headaches. If the syndrome has become systematic and lasts more than a week, it is necessary to begin a course of therapeutic exercises.
The best way to get rid of pain is to eliminate its cause. If this is not possible (for example, with a migraine), you can at least alleviate the condition by eliminating factors that increase pain - tobacco smoke, bright light, loud noise. Some types of pain are not responsive to medication but can be managed with oxygen and physical therapy.
Pain associated with vascular damage is treated by treating the disease that caused it - hypertension, arteritis, etc. Relaxation, exercise, and massages will help with headaches caused by overwork or stress.
With timely consultation with a doctor and correct diagnosis, you can not only get rid of headaches at night, but also prevent its relapses. It is also important to remember that a healthy lifestyle will help you avoid pain at all in 80% of cases.