general characteristics
Auditory hallucinations are manifested by various sound phenomena - melodies, noises, voices, which are perceived by patients as true, really existing.
The attitude towards hallucinatory phenomena as a pathology is formed gradually as a result of beliefs on the part of loved ones and doctors. In mental disorders, when hallucinatory sounds are justified by delusional concepts, patients continue to believe in the reality of what they hear, despite the assurances of others. Auditory hallucinations can be simple or complex. Simple ones are represented by acoasms - noise, hissing, roaring, grinding, buzzing. Sometimes patients cannot guess what type of source generates the sound, in other cases they clearly determine its “reasons” - the shuffling of a boot sole, the creaking of floorboards, the hum of a car. Another type of simple auditory hallucination is phonemes. These are speech deceptions of hearing in the form of shouts, individual vowel sounds, syllables, and fragments of words.
Complex auditory hallucinations are represented by musical and verbal images. With musical phenomena, people hear playing musical instruments, singing, and melodies. Verbal hallucinations – individual words, phrases, monologue or dialogic speech. Verbal hallucinatory phenomena include commentary, threatening and imperative. Commenting voices express an opinion about the patient’s actions, threatening voices intimidate, imperative voices order or prohibit something to be done, for example, they demand to commit suicide or refuse to eat.
Proposed theories of the mechanisms of auditory hallucinations
Some studies have shown that when patients experience auditory hallucinations—that is, hearing voices—an area of their brain called Broca's area increases in activity. This zone is located in the small frontal lobe of the brain and is responsible for speech production: when you speak, it is Broca's area that works. One of the first to study this phenomenon were professors Philip McGuire and Suchi Shergill from King's College London. They noticed that their patients' Broca's area was more active during auditory hallucinations compared to when the voices were silent. This suggests that auditory hallucinations are produced by the speech and language centers of our brain. The results of these studies led to the creation of internal speech models of auditory hallucinations.
When we think about something, we generate inner speech - an inner voice that voices our thinking. For example, when we ask ourselves, “What will I eat for lunch?” or “What will the weather be like tomorrow?”, we generate inner speech and are thought to activate Broca's area. But how does this internal speech begin to be perceived by the brain as external, not coming from itself? According to internal speech models of auditory verbal hallucinations, such voices are internally generated thoughts or internal speech that is somehow misidentified as external, foreign. This leads to more complex models of the process of how we monitor our own inner speech.
©Kate MacDowell
English neuroscientist and neuropsychologist Chris Frith and other scientists have suggested that when we engage in the process of thinking and inner speech, Broca's area sends a signal to an area of our auditory cortex called Wernicke's area. This signal contains information that the speech we perceive is generated by us. This happens because the transmitted signal presumably dampens the neural activity of the sensory cortex, so it is not activated as intensely as by external stimuli, such as someone talking to you. This model is known as the self-monitoring model, and it suggests that people with auditory hallucinations have a deficit in this process, causing them to be unable to distinguish between internal and external speech. Although the evidence for this theory is currently quite weak, it is certainly one of the most influential models of auditory hallucinations to emerge in the last 20–30 years.
Causes of auditory hallucinations
Auditory hallucinations are more often classified as productive psychopathological symptoms, but can occur as a manifestation of neurological pathology affecting certain brain structures, as well as in the absence of diseases. The underlying causes of hallucinatory symptoms are abnormal activation of the auditory cortex, unrelated to external stimuli, and loss of the ability to recognize internal speech as one's own. Factors that provoke auditory hallucinations are physiological changes, mental illness, organic damage to brain tissue.
Physiological reasons
According to medical research, sometimes auditory hallucinations occur in completely healthy people. They are transient in nature, often provoked by unusual external influences. The critical attitude towards sound phenomena remains relatively intact: at the moment of hallucination, people cannot distinguish what is heard from reality, but later they begin to think about the unreality of what happened. The most likely causes of hallucinatory experiences in a healthy person:
- Lack of sleep.
Refusal to get enough sleep provokes depression of nervous functions: cognitive processes and orientation in time and space deteriorate. Visual and auditory hallucinations appear on the fourth day of insomnia, when anxiety, fussiness increases, and a feeling of unreality of the surroundings arises. Volitional functions are lost, the person becomes suggestible and controllable. - Sensory deprivation.
People are constantly surrounded by background noise. Absolute silence disorganizes the functioning of the brain; it begins to compensate for the missing stimuli with its own pathological activity, creating auditory hallucinations - sound images that have no external cause. Thus, astronauts in outer space are at risk of hallucinosis due to sensory deprivation. - Transition to sleep.
Just before falling asleep, some people experience hypnagogic visual and auditory hallucinations. Their content is often related to events that happened during the day or about which the person has been thinking a lot lately. Auditory phenomena are unstable and easily disintegrate when trying to recognize their source. Similar hallucinations are sometimes observed during periods of awakening and light daytime naps. - Adolescence.
Auditory hallucinations without any illness can occur in children during adolescence. The reasons are a violation of the process of internalization of the inner voice: when a child learns to conduct internal dialogues and read to himself (not out loud), inner speech is separated from its source, that is, the process of its generation ceases to be fully realized. There is a feeling of a voice from outside.
Mental illness
The most common causes of persistent auditory hallucinations are mental disorders. Patients can hear noises, the sound of steps, creaks, voices, melodies. In the structure of hallucinatory-delusional syndrome, the plot of hallucinations echoes delusional ideas: it strengthens them, guides them, confirms them. The most dangerous are imperative voices that order the patient to perform actions that harm himself or others. Possible causes of hallucinations of the auditory modality in psychopathology:
- Bipolar affective disorder.
The disease is characterized by alternating manic and depressive periods. Severe forms of depressive phases occur with increased distrust of others, the formation of ideas of relationship, and manic stages - with the experience of bliss, delusions of grandeur and physical impact, and auditory hallucinations. The patients' thoughts become incoherent, their behavior becomes agitated and inhibited. Auditory deceptions of perception enhance delusional ideas (“someone is whispering, which means they want to attack”). - Schizophrenia.
About 70% of patients hear voices that threaten without reason, give information about the desire of others to cause harm, comment on the patient’s actions, make comments, order suicide, or injure another person. Another option is antagonistic auditory hallucinations, when a person hears a dispute between “good” and “bad” voices. Associated symptoms are delirium, fragmented thinking, inadequacy of emotions and behavior. - Epileptic psychoses.
Acute psychoses occur with catatonia, delirium, hallucinosis, and religious-ecstatic states. Symptoms may appear against a background of clear or clouded consciousness. In chronic epileptic psychoses, imperative hallucinosis develops - voices force the patient to perform neutral or illegal actions. Auditory hallucinations are of a religious nature (for example, the voice of God demanding punishment for sins). - Alcoholic psychoses.
In people who abuse alcohol, the causes of hallucinations are acute intoxication and meta-alcohol psychosis. With alcohol intoxication, auditory hallucinations occur at the height of intoxication, especially after taking surrogates. Voices, as a rule, convey neutral information: they comment, discuss a person’s actions. During alcohol withdrawal after prolonged use, delirium (stupefaction) and alcoholic paranoid develop, which is accompanied by hallucinations of a threatening nature.
Neurological diseases
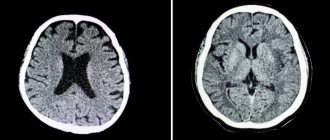
Hallucinatory phenomena of various modalities can occur as a result of organic damage to the central nervous system: with neurodegenerative pathologies, vascular diseases, ischemic, traumatic and tumor processes in the brain. The origin of auditory deceptions of perception is associated with increased excitability of the temporal lobes of the cortex. The following pathologies are considered as causes of hallucinations:
- Neurodegenerative diseases.
In degenerative diseases, progressive death of brain cells occurs. Dementia develops, which manifests itself as a steady decline in memory, attention, and thinking. Auditory hallucinations are often combined with visual and olfactory ones. Voices are characteristic: words, calls, whole phrases, telling the patient what to do. - Local brain lesions.
Heart attacks, strokes, aneurysms of cerebral arteries, tumors, traumatic brain injuries are the causes of auditory hallucinations when the pathological focus is localized in the temporal lobe. Patients hear unformed noises, speech, melodies, and singing. With temporal lobe epilepsy, the sound of one or more musical instruments often occurs. - Acquired deafness.
Weakening of hearing or the development of absolute deafness leads to the appearance of auditory hallucinatory phenomena. The mechanism of their formation is similar to that in a situation of sensitive deprivation: the lack of impulses from the outside is compensated by the brain. Patients often hear ringing, singing, and music. This symptom persists after fitting a hearing aid or after installing a cochlear implant.
Causes of hallucinations
What can cause hallucinations in a person?
Researcher A.S. Shmaryan (1949), studying hallucinations as the main positive symptom of schizophrenia, suggested that damage to the temporal lobes of the brain contributes to this perceptual disorder. For example, a tumor in this area often causes hallucinations.
Observing patients with a disease associated with hallucinations, a number of researchers noted a structural and functional disorder in the superior temporal gyrus and damage to the anterior section of the superior gyrus of the left temporal lobe of the brain.
The surgical method of treating epilepsy, in which electrical stimulation of the superior temporal gyrus occurs, can also lead to various acoustic effects: noise, ringing, rumble.
Damage to the right temporal region causes olfactory, gustatory and musical hallucinations. If the left region is affected, verbal hallucinations may occur with severe anxiety.
Auditory hallucinations occur when not only the temporal lobe of the brain is affected, but also its other structures that take part in the functioning of the hearing analyzer. There is a hypothesis that states that in patients with schizophrenia, when the processes responsible for recognizing internal speech are disrupted, an erroneous perception of their own internal speech occurs as speech from the outside, addressed directly to them.
In addition to the above, the appearance of various types of hallucinations can provoke a state of intoxication of the body with certain drugs or substances.
Diagnostics
Auditory hallucinations are often a symptom of mental illness or organic brain pathology. If there is a suspicion of psychopathology, a clinical conversation and pathopsychological testing are carried out to assess changes in the cognitive and emotional-personal spheres. To confirm or refute the presence of an organic cause, laboratory tests of blood, urine and cerebrospinal fluid, EEG, CT and MRI of the brain are performed. To detect hallucinations themselves, a psychiatrist uses the following methods:
- Anamnesis collection.
Obtaining information about symptoms can be difficult because patients often lack critical understanding of the nature of hallucinations. Interviewing family members allows the doctor to determine the approximate duration of the disorder, accompanying changes in behavior, emotional reactions, and intellectual abilities. General information about the patient is also taken into account: age, presence of vascular and neurological diseases, alcohol or drug addiction. - Observation.
The presence of auditory hallucinations can be detected by observing the patient’s behavior: he listens to something, holds his head half-turned, pauses for no apparent reason before answering the doctor’s question. When there are intrusive voices, the patient enters into a dialogue with them: asks them to be silent, not to indicate. - Aschaffenburg sample . A perceptual disorder hidden by the patient can be identified using a provocative test. The patient is invited to talk on a switched off phone and share his impressions of the conversation. The presence of auditory hallucinations is confirmed when conducting a dialogue, discussing its topic with a doctor. A positive result is most typical for alcoholic delirium.
Diagnosis and treatment of hallucinations
Of course, the presence of any of the above types of hallucinations in a person cannot go unnoticed by others and does not require a specialized diagnostic method. A person talking to a non-existent character and trying to get rid of a snake crawling on his body, but existing solely in his imagination, cannot help but attract attention. And this is very important, because... the presence of hallucinations is an indicator for immediate contact with specialists and placement of the patient in a hospital setting. This is necessary so that you cannot harm yourself or someone close to you.
Hallucinations indicate the development of a mental illness, and sometimes a whole complex of them. Sometimes the appearance of hallucinations indicates damage to certain parts of the brain. In such cases, treatment is aimed primarily at eliminating the disease that is accompanied by hallucinations. Treatment is usually complex and depends on a number of reasons: the nature of the diseases that led to the occurrence of hallucinations, physiological parameters of the body, biochemical blood parameters, etc. It is important to begin treatment of the disease in time to prevent its further development.
| Read more about the treatment of schizophrenia |
Any questions? Need specialist help? Call us
Treatment
The basis of symptomatic care for patients with hallucinations is the selection of antipsychotic drugs that alter dopamine metabolism. They reduce psychomotor agitation and thinking disorders, and stop hallucinatory-delusional phenomena. In case of severe emotional disorders, antidepressants and mood stabilizers are additionally prescribed. In some cases, cognitive psychotherapy, aimed at convincing the patient of the unreality and pathological nature of audible phenomena, is effective.
How to treat?
To answer this question, the first step is to visit an otolaryngologist. The doctor will conduct a detailed examination of the nasal cavity and paranasal sinuses. This will allow you to determine at what level the lesion is present - peripheral or central. If pathological processes are identified (inflammation, hyperplasia of the mucous membrane, etc.), then they are simultaneously treated.
In modern otolaryngology, gentle surgical techniques (mainly endoscopic) and conservative tactics are used. If peripheral pathology is excluded, then the next step is to consult a neurologist. After identifying neurological disorders and diseases, the doctor will prescribe differentiated treatment that will help cope with olfactory hallucinations.
At ENT Clinic No. 1, appointments are conducted by qualified otolaryngologists. Our specialists are constantly improving their professionalism to provide assistance in accordance with the latest advances in medicine. Make an appointment and feel the joy of a full life without foreign odors!
PsyAndNeuro.ru
Hallucinations are an important symptom for the diagnosis of various psychotic disorders. Although a number of specific characteristics, such as insulting, commentary, and imperative voices, as well as auditory hallucinations of an extracampal nature (i.e., beyond the “sensitive field” of the analyzer), are no longer highlighted in the DSM-5, many clinicians still tend to consider that hallucinations in schizophrenia can be identified based on these characteristics.
However, it is worth considering that there is growing recognition among scientists that hallucinatory experiences span a wide range of mental disorders and may even be part of the everyday experience of people who do not meet the criteria for any mental disorder.
In a new study, F. Waters and C. Fernyhough analyzed whether certain characteristics of hallucinations thought to be specific to schizophrenia are indeed so by conducting a systematic review of scientific papers examining direct comparisons of the clinical characteristics of auditory and visual hallucinations among 2 or more groups of patients, one of which necessarily included persons with schizophrenia. 43 articles were reviewed, studying hallucinations in 4 main groups: non-clinical conditions; drug and alcohol related conditions; various neurological diseases and other medical conditions, as well as mental disorders.
The authors provide evidence that hallucinations in mental disorders, in addition to schizophrenia, schizotypal disorder, as well as schizoaffective disorder, can also occur in bipolar disorder (in manic, depressive and mixed phases), unipolar depression, dissociative disorders, personality disorders, PTSD, anorexia and bulimia nervosa.
Hallucinations can also be a consequence of the pathology of various physiological systems. For example, acquired deafness is a common cause of auditory hallucinations, and various eye diseases or damage to the afferent visual pathways can cause visual hallucinations (in Russian psychopathology, this type of perceptual deception is called Charles Bonnet hallucinations). Various metabolic disorders associated with endocrine status, including thyroid dysfunction and Hashimoto's disease, vitamin D and B12 deficiency, can also cause hallucinations. Other conditions associated with hallucinations include chromosomal disorders such as Prader-Willi syndrome, various autoimmune diseases, acquired immunodeficiency disorders such as HIV/AIDS, and sleep disorders such as narcolepsy. Neurological diseases such as tumors, traumatic brain injuries, epilepsy, and various vascular diseases can also cause hallucinations. Perceptual deceptions are also quite common in neurodegenerative diseases such as Parkinson's disease and Lewy body dementia.
Additionally, it is worth paying attention to the fact of hallucinatory experiences in people who do not meet the criteria for mental disorders. Psychotic experiences occur in approximately 4-7% of the general population, with 80% of such cases being transient. In this group, the prevalence of hallucinations depends on the stage of development: for example, in children they occur in 8%, and in older people in 1-5% (which may again indicate a connection with the development or involution of the nervous system). Hallucinations can also occur in situations involving extreme physiological or psychological stress, such as extreme fatigue, sensory deprivation, bereavement, etc.
The results of this study showed that no characteristic of hallucinations clearly predicts a diagnosis of schizophrenia, with the exception of age of onset in late adolescence. Among the 21 characteristics of hallucinations in schizophrenia given in the article, 95% were observed in other mental disorders, 85% in various neurological diseases, 66% in conditions associated with drugs and alcohol, 52% in non-clinical conditions (See Table 1 ).
Tab. 1 Phenomenological features of hallucinations (abbreviated version)
| Characteristic features of hallucinations | Schizophrenia | Non-clinical conditions | Conditions associated with drugs and alcohol | Neurological diseases and other medical conditions | Other mental disorders |
| Auditory hallucinations (“voices”) | 75% | ±58% | ±50% | ±32% | 46%—57% |
| Hallucinations in three or more sensory systems | 60% | None | ±16% | ±20% | ±76% |
| Appear alive and real | 80% | ?% | ±26% | ±48% | 54%—100% |
| Extracampal properties | 50% | ±57% | ±70% | ±37% | ±60-83% |
| Commentary character | 65% | 20-41% | 20-60% | 10-41% | 40-80% |
| Offensive character | 60% | 43-53% | ?% | ±33% | 58%—93% |
| Imperative character | 84% | Ots. | ±4% | ?% | 62%—82% |
| Lack of conscious control | 78% | Ots. | ?% | ±53% | ±78% |
| Family history of mental illness | 30% | Ots. | ±23% | ±30% | ±40% |
| Age of onset: late teens to early 20s. | 18-24 | Ots. | Ots. | Ots. | Ots. |
| Similarities with schizophrenia (%) | — | 52% | 66% | 85% | 95% |
In general, scientists have concluded that when considering hallucinations, it is inappropriate to give weight to certain characteristics of hallucinations when diagnosing schizophrenia, because The results of the study did not confirm that, based on certain characteristics of hallucinations, it is possible to unambiguously diagnose schizophrenia. Moreover, Schneider's first-line symptoms were not specific to schizophrenia, because they occurred in non-clinical conditions - 20-40%, narcolepsy - 10-17%, alcohol withdrawal - 26-60%, mood disorders - 20-55% and dissociative disorders - 80%.
This review provides important insights regarding the diagnostic value of hallucinations. For example, hostile voices speaking in the third person and causing distress may equally be present in a patient with schizophrenia, epilepsy, a brain tumor, or PTSD. However, this finding does not suggest that hallucinations are clinically uninformative.
In general, as the study authors conclude, hallucinations are a feature of human perception that crosses the boundaries of diagnostic categories and spans the gap between psychopathological and non-clinical experience. Therefore, it is important for the clinician to focus on the combination of hallucinations with other symptoms and clinically significant findings.
The material was prepared as part of the Pro-Schizophrenia project, a specialized section of the official website of the Russian Society of Psychiatrists dedicated to schizophrenia, modern approaches to its diagnosis and treatment.
Source: F. Waters, C. Fernyhough. Hallucinations: A Systematic Review of Points of Similarity and Difference Across Diagnostic Classes. Schizophrenia Bulletin, Volume 43, Issue 1, 1 January 2017, Pages 32–43, https://doi.org/10.1093/schbul/sbw132
Prepared by: Kasyanov E.D.