The disease develops when the pathogen enters the body through damage to the skin and mucous membranes (wounds, burns, frostbite). Minor injuries sustained when working with soil on personal plots are especially dangerous.
The incubation period of the disease ranges from 3 to 30 days.
Often, at the onset of a person’s illness, the wound has healed and the sick person does not remember the location and nature of the damage. First, vague symptoms appear: deafness, headaches, loss of appetite, anxiety, a slight increase in temperature, and later a convulsive contraction of the masticatory and facial muscles joins. Then the cramps can spread to the entire muscle. When the occipital muscles and back muscles are affected, the body bends backward. The arms and legs are less affected, but extensor spasms are possible. Particularly dangerous are prolonged spasms of the respiratory muscles, which lead to death.
Emergency prevention of tetanus is carried out for any injuries and wounds with a violation of the integrity of the skin and mucous membranes, frostbite, and burns of the second, third and fourth degrees, animal bites, penetrating injuries or surgical interventions on the gastrointestinal tract, in unvaccinated persons or persons with an unknown vaccination history , out-of-hospital abortions, childbirth outside of medical institutions, gangrene or tissue necrosis of any type, abscesses, carbuncles. Emergency prophylaxis of tetanus is carried out until the 20th day from the moment of injury. The decision to carry out emergency prophylaxis is made based on the conclusion of a doctor at a clinic or hospital.
Immunization is the only reliable way
prevention of tetanus. Vaccinations against tetanus are mandatory and are carried out in accordance with the national calendar of preventive vaccinations from the age of three months, along with vaccinations against diphtheria. Vaccination consists of 3 vaccinations followed by revaccination at the age of 18 months, 7 years, 14 years, and then revaccination is carried out every 10 years until the last revaccination (for life).
Vaccinations against tetanus are carried out in medical institutions (clinics) at the place of residence or work free of charge.
At the same time, against the background of mass immunization in the Russian Federation, the epidemiological features of tetanus have changed: diseases are registered among the adult population, mainly among people over 50 years of age, who account for about 70%; the most affected group are pensioners. Infection occurs in 90% of cases with minor injuries, for which the victims, as a rule, do not seek medical help. But an early visit to the surgical office or emergency department (on weekends and holidays) to a medical institution and emergency tetanus prophylaxis can save your life and the lives of your loved ones.
Tetanus
Tetanus
3549 January 25
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Tetanus: causes, symptoms, diagnosis and treatment methods.
Definition
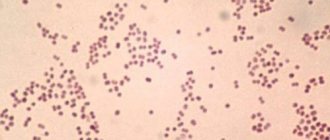
Tetanus is a dangerous infectious disease caused by the tetanus bacillus Clostridium tetani
. This bacterium is extremely stable in the environment: its spores remain viable for years, and at a temperature of 90°C - for about two hours. Vegetative forms of clostridia die within a few minutes in boiling water and within 3-6 hours after treatment with antiseptics and disinfectants. Once in the wound, bacteria begin to produce a toxin that affects the nervous system, leading to severe muscle spasms and cramps.
As the disease progresses, muscle spasm causes severe breathing problems and can ultimately be fatal.
Tetanus can be contracted anywhere in the world, but most cases of infection occur in hot countries with poor sanitary and hygienic conditions. In countries with temperate climates, the peak incidence occurs in the summer-autumn period.
Causes of tetanus
The lack of preventive vaccination of the population plays a huge role in the spread of infection.
Tetanus bacilli live in the soil. The route of infection is contact. Bacteria enter the body through wounds, abrasions, burns, frostbite, etc.
After entering the wound, bacteria begin to produce a toxin that penetrates the processes of nerve cells, causing spastic muscle contractions and cramps.
Due to its ability to exist for a long time in the form of spores in soil, water bodies, and on objects, the tetanus causative agent can enter any premises with dust and dirt and infect any surfaces, including medical ones.
Classification of the disease
Depending on the route of infection:
- wounded,
- postoperative,
- postpartum,
- post-burn,
- after frostbite,
- post-injection,
- tetanus of newborns.
By prevalence:
- local (only the muscles closest to the wound are affected),
- generalized (all muscles of the body are affected).
According to the clinical course:
acute, chronic, with a mild course (symptoms are mild).
By severity:
mild form (about 3 weeks pass from the moment of infection to the first symptoms), moderate form (symptoms appear 2 weeks after infection), severe (symptoms appear 9–15 days after infection), extremely severe (the incubation period lasts only 3 -5 days).
Tetanus symptoms
The first symptoms appear on average 7–10 days after infection; in rare cases, the disease can develop earlier.
There are three classic symptoms of tetanus:
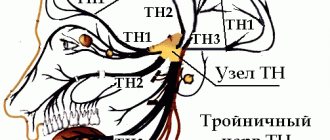
- Trismus, that is, convulsions and stiffness of the jaw muscles, opening the mouth is difficult, and in the later stages of the disease it becomes impossible. Contraction of the facial muscles creates a specific expression of the “sardonic grimace” - a simultaneous expression of suffering and a smile;
- stiff neck, which causes stiffness and pain in the neck muscles, limited neck mobility when the head is tilted forward;
- dysphagia (impaired swallowing function).
Other symptoms of tetanus:
- pain in the wound area and sometimes twitching of nearby muscles;
- stiffness of the abdominal muscles;
- painful body spasms that last for several minutes, usually caused by minor phenomena - a draft, loud noise, touch, light;
- headache;
- pain in the back and neck;
- increased sweating.
As the disease progresses, cramps spread to the muscles of the whole body (opisthotonus), the patient, to alleviate the condition, takes various forced positions - arches, bends to the side or freezes like a pillar (hence the name of the disease).
In severe cases, the cramps are so severe that they can lead to muscle tears and broken bones.
Severe disease is accompanied by an increase in body temperature, a decrease in blood pressure, and an increase in heart rate.
Diagnosis of tetanus
As a rule, an accurate diagnosis can be made based on the clinical picture in the presence of a wound indicating possible infection.
Laboratory diagnosis is not performed, since the presence of antibodies in the blood may indicate vaccination in childhood. With tetanus, there is no increase in antibody titers, since even lethal doses of exotoxin do not cause an immune response. The cerebrospinal fluid (CSF) also remains unchanged, despite damage to the nervous system.
In some cases, bacteriological methods are used (microscopy of fingerprint smears, histological examination of tissues excised during surgical treatment of wounds, inoculation of wound discharge on nutrient media under anaerobic conditions), which make it possible to detect the pathogen at the location of the wound. However, it is possible to isolate a culture of the pathogen from a wound in only 30% of patients.
Which doctors should I contact?
In case of injury with a violation of the integrity of the skin, frostbite or burn, you should consult a traumatologist or surgeon, who, after examination, collection of anamnesis and complaints, will refer the patient to specialized specialists: an infectious disease specialist, a neurologist.
Treatment of tetanus
Treatment of patients with tetanus is carried out only in a hospital. In severe cases of the disease, the patient is hospitalized in the intensive care unit.
Strict bed rest and complete rest, reduction of noise and light exposure are indicated.
Muscle relaxants and antipsychotics are used to relieve seizures. Due to swallowing disorders, medications are often administered intramuscularly or intravenously.
If the respiratory muscles are damaged, artificial ventilation may be required.
The administration of antitetanus serum is mandatory. Moreover, the sooner it is introduced, the greater the likelihood of neutralizing the toxin.
Surgical treatment consists of treating the wound, removing foreign bodies, prescribing antibacterial therapy if a bacterial infection is suspected and in order to prevent the development of a purulent process. The wound cannot be sutured to prevent the proliferation of tetanus bacillus, since a closed wound without access to oxygen is a beneficial environment for this bacterium.
Particular attention is paid to replenishing fluids, providing nutrition with sufficient calories, rich in vitamins and microelements. In case of severe swallowing impairment, nutrition is provided with liquid nutritional mixtures using a probe - a special thin tube that is inserted through the nose into the stomach cavity.
Complications
Complications are divided into early, which occur in the midst of the disease, and late, which can remain after recovery.
Early complications include:
- Respiratory infections (bronchitis, pneumonia) - occur as a result of impaired ventilation of the lungs associated with muscle spasms and prolonged bed rest.
- Myocardial infarction - observed in severe and extremely severe cases of tetanus, since the heart muscle, like other muscles of the body, can be exposed to tetanus toxin. The toxin is especially dangerous for older people and patients with cardiovascular diseases.
- Sepsis is a systemic inflammatory response in response to microorganisms entering the bloodstream. The danger of sepsis is that the inflammatory process affects all organs and systems of the body, disrupting their proper functioning, and in some cases can lead to death. Treatment of sepsis requires the simultaneous administration of several intravenous antibiotics, constant monitoring of laboratory blood parameters, pulse, blood pressure, body temperature, and urination.
- Bone fractures, dislocations, and muscle ruptures are characteristic of extremely severe tetanus.
Late complications:
- Spinal deformity.
- Contractures of muscles and joints are a condition in which a muscle or joint retains restriction and stiffness in movement even after recovery from the underlying disease.
- Heart rhythm disturbances.
- Temporary paralysis of the cranial nerves, the most common manifestation of which is impaired swallowing function, double vision, ptosis (drooping) of the eyelid.
Prevention of tetanus
There are planned and emergency prevention.
Planned prevention includes vaccination, which is carried out from the birth of the child.
In Russia, the course of vaccination against tetanus consists of 3 DTP vaccinations (at the age of 3, 4.5 and 6 months) and a single revaccination at the age of 18 months. Further revaccination is carried out at 6–7 years and at 14 years with the ADS-M toxoid vaccine. Subsequent revaccinations are carried out every 10 years.
All vaccinations must be included in vaccination certificates. A full course of vaccinations provides protection for 95–100% of the vaccinated population.
Emergency prevention should be carried out in unvaccinated or incorrectly vaccinated people who receive any mechanical damage to the skin. To do this, anti-tetanus serum is administered as early as possible (permissible up to 20 days from the moment of injury). Before its administration, a test with diluted serum is carried out: if the diameter of the redness is less than 1 cm, the test is negative, if 1 cm or more, it is positive. If the test is negative, the serum is injected subcutaneously into the outer surface of the shoulder or subscapular area. If the test is positive, serum administration is contraindicated. In this case, human immunoglobulin is administered.
Sources:
- Infectious diseases: national guidelines / Ed. N.D. Yushchuka, Yu.Ya. Vengerova. - M.: GEOTAR-Media, 2009. P. 521–529.
- Ryumin A.M., Sobolevskaya O.L., Korochkina O.V., Volsky N.E., Mikhailova E.A., Otmakhova I.A., Sobchak D.M., Khryaeva O.L. A case of mild tetanus: tactical features of management // Nizhny Novgorod State Medical Academy. 2021. pp. 98–100.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.