Oh gods, gods, why are you punishing me? Yes, no doubt! It’s her, her again, the invincible, terrible disease of hemicrania, which makes half your head hurt. There is no remedy for it, there is no salvation. I’ll try not to move my head.. This is exactly how Pontius Pilate describes his headache in the immortal work of M.A. Bulgakov. The main character is so afraid of pain that he “cowardly thinks about death.” Unfortunately, not every person suffering from this illness finds his Yeshua Ha-Nozri, who, as we remember, not only recognized the illness, but was also able to heal it. But this is a literary work, and we will try to analyze this disease from the point of view of modern medicine.
And first a little history
The French word “migraine” (migraine) came to us from Latin; this disease was also called hemicrania (hemicrania - “half of the head”). The first written references to migraine symptoms are found in the cuneiform tables of the ancient Sumerians, which are more than 7,000 years old. Perhaps our ancestors suffered from migraines back in the Neolithic. Attempts to treat this particular disease can explain some of the skulls with traces of trepanation. Most likely, the ancient Homo sapiens tried to “release the evil spirit” that, in their opinion, was lodged in the skull. Migraine was well known to the healers of Ancient Egypt - papyri with recipes for its treatment have survived to this day. The first detailed description of a disease with severe headache, very similar to migraine, was made by the ancient Greek physician Aretaeus of Cappadocia in his book “On Acute and Chronic Diseases.” This healer called the disease heterocrania (heterokrania - another, alien head). He also compiled the first detailed classification of migraines and described several cases of death due to migraines, which, most likely, were actually cerebral hemorrhages. Celsus, a physician who worked in the 1st century BC, believed that the disease lasts throughout life, but does not threaten it. He put forward the (incorrect) theory that migraine attacks are usually accompanied by fever. There are also mentions of migraine in Hippocrates and Avicenna (in the “Canon of Medical Science”). However, the name given by the ancient Roman physician Claudius Galen has survived to this day - hemicrania. Galen thereby emphasized one of the distinctive features of this disease - the localization of pain in only one half of the head. The Greek physician Eginat identified factors that provoke migraine attacks, such as noise, shouting, bright light, strong smelling substances, and drinking wine. In the 4th century AD, Caelius Aurelian drew attention to the fact that migraine pain can be localized in the depths of the eye socket and radiate to the back of the head. In the 6th century AD, Alexander of Tralles pointed out the difference between migraine (hemicrania) and other headaches (cephalgia). At the same time, he believed that the source of headaches were disorders of the gastrointestinal tract and proposed replacing bloodletting, which was practiced to treat the disease, with enemas. With the advent of the Middle Ages, difficult times came for migraine sufferers. They were accused of having connections with the devil, and they tried to “drive out the possessing demons” with torture and torment. Only in the 16th century did scientists and doctors return to this problem. Various theories have been put forward about the origin of hemicrania and methods of its treatment. The disease was associated either with visual impairment or with lesions of the digestive system. Until the end of the 19th century, the main methods of treatment were bloodletting (6 ounces at a time, equivalent to 150 grams) and emetics. The period of the late 19th and early 20th centuries was characterized by a surge of activity in the study of migraine. For example, Flatau (Polish neurologist), in his monograph, which most fully describes the then ideas about migraine, provides references to more than 470 works on this problem. Among the great and famous people, Julius Caesar, Calvin, Linnaeus, Pascal, Beethoven, Darwin, Marx, Nobel, Heine, Edgar Allan Poe, Maupassant, Wagner, Chopin, Tchaikovsky, Nietzsche, Freud suffered from migraines.
Now let’s leave history and move on to modern ideas about this disease
Migraine is a neurological disease, the most common and characteristic symptom of which is episodic or regular severe and painful attacks of headache in one (rarely in both) half of the head. According to the ICD-10 classification, it is classified as a neurological disease (class G), a group of “episodic and paroxysmal disorders”. Migraine itself is under code 43. Currently, the following forms of the disease are distinguished (given with ICD code):
- G43.0 Migraine without aura (simple migraine)
- G43.1 Migraine with aura (classical migraine)
- G43.2 Migrainous status
- G43.3 Complicated migraine
- G43.8 Other migraine. Ophthalmoplegic migraine. Retinal migraine
- G43.9 Migraine, unspecified
According to epidemiological studies, in developed countries of Europe and America, migraine affects from 3 to 16% of the population, and according to some data, up to 30%; among women, 18% suffer from migraine, among men - 6% and among children - 4%. The severity of the disease varies from rare (several times a year), relatively mild attacks, to daily; but most often migraine attacks recur at intervals of 2-8 times a month. The social significance of the disease is great, despite the fact that the disease itself does not lead to death. It is worth remembering that attacks, as a rule, occur suddenly, which leads to the patient’s loss of ability to work and the inability to perform their work duties. The unexpected nature of the attacks is also due to the fact that most migraine patients experience attacks without an aura. Patients whose attacks usually occur with an aura also occasionally experience paroxysms without it. In other words, predicting when the next attack will occur is very, very difficult.
Migraine treatment
Migraine therapy is aimed at both pain relief during attacks and reducing their frequency. The list of painkillers includes paracetamol, aspirin, anti-inflammatory drugs, and ergotamines.
Along with these medications, triptans are used - drugs with complex effects. At the same time, they relieve pain, constrict blood vessels in the brain and act on receptors that release substances that provoke inflammation. As a result, the intensity of the pulsation of pain sensations decreases and they disappear completely.
Despite their effective action, systematic use of migraine medications containing caffeine and codeine is extremely undesirable due to the fact that they lead to addiction. The brain has the ability to remember the stimulating effect of these substances, which gives rise to new attacks. As a result, in order to get rid of the headache, the patient is forced to take the medicine again.
Etiology of the disease
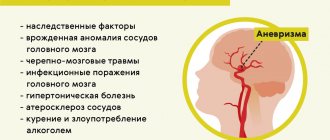
Hereditary factors play a significant role in the occurrence of migraine, and the risk of developing the disease in children with a hereditary burden on the paternal side is 30%, and on the maternal side - 72%. If both spouses suffer from migraine, then the likelihood of it occurring in their children is 80-90%. About 20 mutations have been found in various loci that are in one way or another associated with this disease. At the same time, genetic preconditions are more significant for migraine with aura than for attacks without it. There are also factors that provoke an attack (but it can begin without them). These include, for example: - stress, nervous and physical stress, - food factors (cheese, chocolate, nuts, fish), alcoholic drinks (most often beer and red wine, champagne), - taking hormonal contraceptives, - sleep (lack of , oddly enough, an excess), including changes in time zones, - weather factors (changes in weather, changes in climatic conditions).
Pathogenesis
Scientific American 299, 56 - 63 (2008) The pathophysiology of migraine has always remained mysterious, so by the end of the 20th century, three directions in its pathogenesis had emerged. All of them have received experimental and clinical confirmation. The first direction is based on the assumption: attacks are associated with narrowing or expansion of intra- and extracranial arteries. This is one of the initial theories. She suggests that migraines are caused by sudden constriction of intracranial vessels, causing cerebral ischemia and resulting aura. Following this, expansion of the extracranial blood vessels occurs, which causes headaches (Wolf, 1930). the shunt theory was proposed (G. Hake, 1960s). The headache was explained by the fact that during an attack, blood tends to pass from the artery directly into the vein through the arteriovenous shunt, bypassing the intracranial capillaries. This causes cerebral ischemia, which is the main cause of headaches. The platelet theory suggests that migraine is caused by a primary platelet disorder. When platelets stick together, a significant amount of the neurotransmitter 5-hydroxytryptamine (5-HT) is released. This theory is proven by the fact that platelets of migraine patients have a more pronounced ability to stick together than those of healthy people, and are more sensitive to factors that provoke the release of 5-HT. The second direction explains pain by a discharge arising in the trigger zone of the midbrain (possibly in the serotonergic dorsal raphe nuclei of the brainstem). Recent positron emission studies have shown that the dorsal region near the midbrain aqueduct is activated during migraine. This activity is not reduced even by sumatriptan, even if it reduces migraine pain. These areas of the brain contain serotonin-, norepinephrine-, endorphin- and GABAergic systems. It is assumed that the triggering factor for migraine is the disturbance of this particular complex of neurophysiological interactions in this area. A sharp release of serotonin leads to vasoconstriction of blood vessels (prodromal period), however, 5-HT is quickly processed and removed from the blood, which leads to vasodilation and the development of a headache attack. Therefore, a number of researchers (Vein A.M. et al.; Gtsbel H.) believe that migraine is a primary neurogenic cerebral dysfunction with the presence of genetically determined brain stem failure, severe cortical hyperactivity with periodically occurring dysfunction of the hypothalamus. Finally, the third direction is associated with the excitation of neurons of the trigeminal nucleus in the brain stem (the so-called trigeminovascular system). The axons of these neurons terminate in the arterial walls and release vasoactive neuropeptides. (M. Moskowitz et al., 1989). According to this theory, the source of headaches are the cranial vessels and vessels of the dura mater, which have trigeminal innervation and are under the control of the mid-stem structures of the brain. During a spontaneous migraine attack, the brain stem structures located near the aqueduct of Sylvius, in the area of the locus coeruleus and the reticular formation, are activated, which are a kind of generator of a migraine attack. This leads to antidromic activation of the trigeminal-vascular system with the release of neuropeptides into the vascular wall (substance P, a neuropeptide associated with the gene that controls calcitonin), causing their dilatation, increased permeability and, as a consequence, the development of neurogenic inflammation in it. Aseptic neurogenic inflammation activates the nociceptive terminals of the afferent fibers of the trigeminal nerve located in the vascular wall, leading to the formation of a feeling of pain at the level of the central nervous system. As already mentioned, special attention is currently paid to serotonin as a key link in the pathogenesis of migraine. It is assumed that it is the triggering factor for the development of migraine, and the attack itself can occur through any of these mechanisms or a combination of them. The serotonin theory is also confirmed by the fact that during a migraine attack:
- The content of 5-HT in platelets drops sharply (by 30-40%)
- There is an increased content of serotonin metabolic products in the urine
- Migraine attacks can be provoked by taking reserpine, which promotes the release of 5-HT
- Known anti-migraine drugs (ergotamine) interact with 5-HT receptors
- Intravenous serotonin may relieve migraine attacks.
Causes of migraine
During vascular spasm and subsequent dilation, the walls are greatly stretched, this is due to an increase in serotonin levels. At these moments, migraine attacks occur. After the blood supply returns to normal, the pain goes away. Migraines in women are often hereditary. But we can identify a number of migraine pathogens that lead to its activation:
- Stressful condition, especially if it has been present for a long time;
- Lack of sports and daily activity;
- Poor ecology can also lead to migraine;
- Bad habits - alcohol, cigarettes;
- Sudden climate change and weather;
- Lack of a normal daily routine, lack of sleep;
- hormonal changes;
- Lack of essential vitamins in the body, abuse of fast food;
- Medicines, as side effects or if they contain substances contraindicated for you;
- Exposure to external stimuli - bright light, noise, odors, etc.
Pathophysiology of aura in migraine
The aura is probably caused by cortical spreading - a “brain storm”. It is a wave of intense nerve cell activity that moves across an unusually large area of the cortex (the folded outer layer of the brain) - and especially in the areas responsible for vision. COURTESY OF DAVID W. DODICK (Dodick); UNIVERSITY OF CALIFORNIA, IRVINE, MEDICAL CENTER (Gargus); TAMI TOLPA (brain illustrations); COURTESY OF NOUCHINE HADJIKHANI (brain scans); MIGRAINE ACTION ASSOCIATION AND BOEHRINGER INGELHEIM (aura art) Scientific American 299, 56 - 63 (2008) Following the hyperexcitability phase, there comes a period of relatively long inhibition of nerve cells, during which neurons are in a state of “suspended activity”, when they cannot be excited. If we look at this in more detail, then: neural activity is controlled by precisely synchronized flows of sodium, potassium and calcium ions across the membrane of the nerve cell through ion channels and pumps, providing the resting cell with large amounts of potassium and small amounts of sodium and calcium. The neuron “discharges” and releases neurotransmitters when the flow of sodium and calcium ions rushes through the opening channels and depolarizes the membrane, as a result of which its inner surface becomes positively charged relative to the outer one. After this, the cells hyperpolarize for a short time: allowing potassium ions to rush outward, they now acquire a strong negative charge from the inside relative to the outer surface. The hyperpolarization closes the sodium and potassium channels, and soon after its discharge the neuron returns to a resting state. However, after intense stimulation, neurons may remain overly hyperpolarized or inhibited for a long time. The phase of hyperexcitability and subsequent inhibition, which characterize cortical spreading depression, may explain those changes in blood flow that were detected before the onset of migraine pain. When neurons are active and firing, they require a lot of energy and therefore a lot of blood (during this stage, blood flow increases up to 300%). This is precisely the picture that experts observed on tomograms of patients experiencing aura. However, later, during inhibition, silent neurons need less blood (the level decreases to normal).
Clinical picture
Clinically, a migraine attack without aura consists of three phases: prodrome, migraine attack, postdrome. Symptoms of the prodrome usually develop several hours before a migraine attack and include increased sensitivity or, on the contrary, decreased perception, irritability, tearfulness, excessive yawning, addiction to special foods (most often sweet), drowsiness, swelling. A migraine headache is one-sided, often pulsating, worsens with physical activity, and is accompanied by nausea and repeated vomiting. “Painful” behavior is typical: the patient tries to go to bed, retire to a darkened room, cover his head with a scarf or towel, and avoids bright light and noise. Upon objective examination, patients are asthenized, emotionally tense, and in some, a swollen temporal artery is detected on the affected side. Often patients try to compress the temporal artery, as a temporary cessation of blood flow reduces the throbbing pain. There are no focal changes in the neurological status, but quite often on the side of the headache there is pronounced pain in the muscles of the neck and skull, and tension during palpation. With migraine with aura, a prodrome can also occur, but most often the first phase is an aura, the clinical picture of which depends on the localization of the pathological process. In 90% of patients, it manifests itself in the form of visual disturbances, usually in the form of lightning and zigzags, flashes, sparks, combined with flickering spiral-like contours or scotomas. Sensory disorders - paresthesia - are in second place in terms of frequency of occurrence; first, the hand is usually involved in this process, then numbness spreads to the face and tongue (the so-called spreading cortical depression occurs, combined with regional oligemia). The aura symptoms regress completely after 20–30 minutes (up to 60 minutes), and before the attack there is usually a “free” interval without headache, which lasts no more than an hour, then a migraine attack develops. After the end of the attack, a postdromal period begins, lasting for 24 hours. Patients feel fatigue, muscle pain, swelling, frequent urination, and euphoria. Scientific American 299, 56 - 63 (2008) Ophthalmoplegic migraine is characterized To make a diagnosis of “Migraine with aura,” the patient must meet at least two criteria from points 1 and 2, and criteria 3 and 4 are also mandatory.
- The aura must have at least one of the following characteristics:
- Visual disturbances that occur after the aura (flashes, dots, lines, circles before the eyes)
- Tactile sensations that disappear after the aura (tingling, numbness)
- Speech disturbances completely disappear after the aura
- There are at least 2 symptoms in the aura:
- Visual and tactile symptoms are always the same before attacks
- Aura symptoms develop gradually
- The duration of each symptom is 5-60 minutes
- Headache attacks meet the criteria for migraine.
- The symptoms are not related to other diseases.
Retinal migraine is a very rare disease, which is a paroxysmal bilateral visual impairment in the form of scotoma or loss of visual fields, which lasts 10–15 minutes. Visual disturbances alternate with attacks of migraine without aura or migraine with ophthalmic aura.
Migraine
3100 January 10
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Headache is one of the most common complaints of patients when visiting a family doctor or neurologist. The cause of headache syndrome can be a number of factors.
Headaches vary in duration, nature, and intensity. According to their origin, they are divided into primary and secondary. Primary headaches are an independent pathology in which headache is the first and main complaint. These include migraine, tension headache, and cluster headache. The cause of secondary headaches is diseases that arise as a result of damage to cranial structures (traumatic brain injury, tumors, brain infections, vascular pathology) or that appear for the first time in connection with another disease. This article will discuss one of the forms of primary headache, namely migraine.
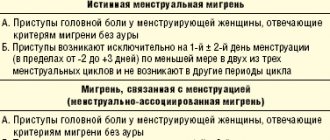
The most common forms of migraine
Migraine is a type of headache that is characterized by periodically recurring attacks of throbbing headaches, often with one-sided localization and sufficient intensity that it makes a person’s daily activities difficult.
Migraines may worsen when climbing stairs or during physical activity. This pain is accompanied by at least one of the following symptoms: nausea, vomiting, increased sensitivity to light and sound. The duration of the attack usually ranges from 4 hours to 3 days. These signs are characteristic of migraine without aura (80% of cases). Migraine with aura (up to 20% of cases) includes, in addition to what is described above, a complex of reversible neurological symptoms preceding the attack. These include:
- completely reversible visual disturbances (flickering spots, stripes, blurred vision);
- completely reversible sensory symptoms (tingling sensation, numbness);
- completely reversible speech impairment;
- completely reversible distortions in the perception of the size and shape of objects.
Causes of migraine attack
It has been proven that migraine headaches are based on neurogenic inflammation and secondary dilatation (persistent dilatation) of blood vessels.
In most patients suffering from migraine, there is an indication of the familial nature of the disease.
The occurrence of migraine depends on the level of female sex hormones, so women suffer from it more often.
In patients suffering from migraine, the excitability of brain cells is increased, which increases when exposed to external and internal migraine provocateurs. Most often, attacks are caused by emotional stress, weather changes, menstruation, hunger, lack of sleep or excess sleep, certain foods (chocolate, citrus fruits, bananas, fatty cheeses) and alcohol intake. In response to stimulation of brain structures, specific proteins are released that cause dilation of brain vessels and activation of pain receptors in their walls. Pain impulses enter the sensory (perceptive, sensitive) cortex of the brain, which forms the sensation of throbbing pain.
What diseases can cause headaches?
Migraine refers to a primary headache when there are no diseases that could provoke an attack. However, secondary headaches, that is, those caused by other diseases, can resemble migraines.
Therefore, the doctor usually conducts a thorough examination of the patient in order to clarify the cause of migraine-like conditions, since the patient’s treatment tactics depend on this.
The following are possible sources of secondary headaches:
- head and/or neck injury;
- vascular lesions of the cervical spine;
- non-vascular intracranial lesions (for example, brain tumors, intracranial hypertension of various origins);
- taking medications and/or stopping them;
- infections;
- violation of the structures of the skull and face;
- mental illness.
Which doctors should I contact if I develop a migraine?
First of all, you should contact your general practitioner. As a rule, migraine does not reveal any changes in somatic and neurological status. If they are detected, the doctor will give a referral for laboratory and instrumental examinations and consultation with specialized specialists: , , , dentist, otolaryngologist to exclude/confirm secondary headaches.
Diagnosis of migraine and additional examinations if secondary headache is suspected
A detailed questioning of the patient is the basis for correct diagnosis. If a migraine is suspected, the doctor may prescribe laboratory and instrumental examinations to the patient, which he selects individually depending on the suspected causes of the headache.
Clinical blood test with a detailed leukocyte formula. One of the main laboratory tests for quantitative and qualitative assessment of blood cells. Includes a cytological examination of a blood smear with counting the content of different forms of leukocytes and determination of the erythrocyte sedimentation rate and smear microscopy in the presence of pathological changes.
Diagnosis and differential diagnosis
DIAGNOSTIC CRITERIA FOR MIGRENUS HEADACHE
- One-way localization
- Pulsating nature of the pain
- Intensity, aggravated by monotonous work and walking
- Nausea, vomiting, photophobia, sensitivity to sounds
- The duration of a migraine attack is from 4 to 72 hours
- History of at least 5 attacks
- The duration of any aura symptom is no more than 60 minutes
- Complete reversibility of aura symptoms
- Interval between aura and headache 60 minutes
It is worth noting that general clinical research methods, such as general blood and urine tests, and a skull x-ray, do not reveal any changes. Cerebrospinal fluid analysis is normal. Echoencephalography also does not give any results. Rheoencephalography data during an attack indicate interhemispheric asymmetry of blood supply, spasm of cranial vessels and decreased tone in the external carotid artery. During the interictal period this is the norm. The encephalogram shows generalized nonspecific dysrhythmia; there is no convulsive activity. EchoEG, CT, and MRI methods are used to exclude space-occupying formations in the brain, the presence of infarcts, hemorrhages and aneurysms. On the other hand, with prolonged and protracted attacks, neuroimaging reveals small infarcts, atrophy of the brain substance, expansion of the ventricular system and subarachnoid space. The following criteria exclude the diagnosis of migraine:
- No change in the “painful side” during the patient’s life
- Progressively increasing headache
- Sudden onset of headache after physical exertion, coughing, sexual activity
- Increase in accompanying symptoms of headache - nausea, vomiting, photo-, phonophobia
- Detection of persistent neurological symptoms, congestive optic discs, meningeal symptoms, impaired consciousness
- The appearance of the first migraine attacks after 50 years
- The appearance of fever, arthralgia, myalgia, arterial hypertension against the background of headache
Let's consider the differential diagnosis of visual aura of migraine and an attack of occipital epilepsy
| Symptom | Migraine aura | Occipital epilepsy |
| Visual image | Flashes of light, flickering, iridescent figures, bean-shaped or zigzag-shaped spots. The color is often snow-white or golden | Multicolor, colorful spherical images |
| Development of symptoms | Gradual development of visual phenomena over 5-30 minutes. Positive symptoms (photopsia, scintillation) are replaced by negative ones (scotoma) | Rapid development within seconds. Negative symptoms are not typical |
| Duration of paroxysm | Less than 60 minutes | 2-3 minutes |
| Spread in the field of view | The image appears in the center of the visual field and gradually spreads to the periphery, leaving behind a scotoma | The image appears in the periphery, usually in the temporal part of the visual field, and is enlarged and/or replicated, moving in the horizontal plane |
| Development of subsequent headache | Migraine headache develops during or within 5-20 minutes after the end of the aura | Postictal headache occurs 3-15 minutes after the attack |
We've sorted out the diagnostics. Let's move on to treatment now.
Treatment
So, treatment includes preventing an attack and stopping it. Basic goals :
- Reduce the frequency and severity of attacks, disability
- Reduce the use of poorly tolerated, ineffective, or unwanted pharmacotherapies for the treatment of acute pain
- Improve quality of life
- Avoid escalation of acute headache when discontinuing medications
- Teach and empower patients to manage their disease to enhance
- personal control of migraines
- Reduce headache-related distress and psychological symptoms
To begin with, all patients are given general recommendations for effective treatment of migraine:
- Compliance with work and rest schedules, avoiding stress and excessive overload
- Maintaining a sleep schedule and avoiding excess sleep on weekends, since excessive sleep often causes “weekend migraines”
- Regularity of meals, avoidance of dietary errors, especially those that are suspected as provocateurs of headache attacks
- Avoiding alcohol, especially red wine and beer
- Limiting intake of coffee and strong tea
- Limiting the use of simple and combined analgesics (no more than twice a week), which is associated with a high risk of developing “reverse headaches”
- Avoiding excessive late-night exercise, especially prolonged sitting with the head bent
- Elimination of possible migraine triggers specific to a particular patient (bright flickering light or light flashes, sudden loud sounds, strong odors)
Analgesics and NSAIDs are used to relieve a migraine attack.
Scientific American 299, 56 – 63 (2008) doi:10.1038/scientificamerican0808-56 The most acceptable and frequently used agent is acetylsalicylic acid. Its action is aimed at blocking the conduction of pain impulses by suppressing the synthesis of pain modulators (prostaglandins, kinins, etc.); the antiplatelet properties of the drug, which help improve capillary blood flow, are also important. Aspirin is prescribed in the first minutes or hours of an attack, no later than 2 hours later, 500–1000 mg per day. For severe attacks, combined analgesics are prescribed solpadeine, etc. Contraindications to the use of these drugs are the presence of gastrointestinal diseases, a tendency to bleeding, and individual intolerance. In second place in terms of frequency of use are ergot preparations, which have a powerful vasoconstrictor effect on the smooth muscles of the artery walls. They prevent neurogenic inflammation and have dopaminergic and adrenergic effects. Drugs in this group are highly effective (75% of attacks are stopped within 20–45 minutes). Example - Ergotamine tartrate 0.01 under the tongue, no more than 3 tablets per day. Fewer side effects occur with combination drugs containing ergotamine and caffeine. At the beginning of an attack, take 1-2 tablets, but no more than 6 tablets per day. Selective serotonin First generation drugs are used: sumatriptan (imigran), 50–100 mg orally; II generation drugs: zolmitriptan (zomig) - 2.5 mg orally, naratriptan (naramig) - 2.5 mg, rizatriptan (maxalt) - 5 mg; III generation drugs - eletriptan (relpax) - 40 mg, etc. Relpax has maximum selectivity to 5-HT/VD receptors, which ensures high efficiency and a minimum number of side effects. Migraine status is Apply:
- prednisolone 40–60 mg or dexamethasone 4–8 mg IV bolus,
- ergotamine IV drip,
- neuroleptics (cerucal, raglan, melipramine),
- tranquilizers.
In this case, the use of periosteal and intraosseous blockades is especially indicated. During the interictal period the following are used:
- β-blockers (anaprilin, atenolol, etc.),
- calcium channel blockers (verapamil, nifedipine),
- antidepressants (amitriptyline, Coaxil, Prozac, etc.),
- serotonin antagonists (metisegrid, peritol, etc.).
In older patients, nootropic and vascular drugs have a good effect. The use of muscle relaxants (sirdalud, mydocalm, etc.) is also effective; it is recommended to include anticonvulsants in treatment - carbamazepine, gabapentin. Drug therapy is selected individually for the patient. Long-term observation is required to keep the number of attacks to a minimum. Author: Denis Dokuchaev Translation of pictures from Scientific American: Georgy Borisov and Boris Lee References
- Clinical guidelines for the diagnosis and treatment of patients with migraine from the American Academy of Neurology
- Migraine: clinical picture, diagnosis, treatment, E. L. Sokov, L. E. Kornilova
- Neurology national guide, 2015 Gusev, Konovalov
- Migraine. Stepanchenkov
- Principles of migraine treatment G.R. Tabeeva
- Modern approaches to the diagnosis and treatment of migraine B.S. Frolov, V.I. Kurpatov.
- Migraine and epilepsy. Yu.E. Azimova, G.R. Tabeeva
- Why Migraines Strike David W. Dodick & J. Jay Gargus Scientific American 299, 56 – 63 (2008) doi:10.1038/scientificamerican0808-56
Treatment of the disease
How to treat migraine? Treatment of this disease should be aimed at eliminating the symptoms of the attack and identifying the causes of the disease.
Most often, among the doctor's prescriptions you can see general painkillers, such as analgin, codeine, phenobarbetal, anti-inflammatory and painkillers - ibuprofen, paracetamol.As an auxiliary treatment, doctors recommend taking a course of psychotropic drugs, for example, domperidone, metoclopramide, etc.
It is not recommended for pregnant women to take any tablets for migraines. In this case, it is better to use alternative methods of stopping attacks:
- Acupuncture.
- Massage.
- Herbal infusions and decoctions.
- Vitamins and dietary supplements.
- Healthy sleep.
- Health-improving gymnastics and swimming.
Before putting into practice the chosen method of treatment, you should definitely consult your doctor.