05/10/2021 | Category Symptoms of cervical osteochondrosis
Many who had an ultrasound of the neck saw in the conclusion the phrase “impaired venous outflow.” Let us immediately note that if this is discovered, this is already good, it means that the doctor looked carefully, not in a hurry, and did not miss anything. Sometimes there is no such record, although in fact there is a problem. The lack of recording may be due to various reasons, including due to outdated equipment; we will not dwell on this, but further we will describe the factors and symptoms by which it can be understood that the venous outflow is impaired, even if this is not indicated by the ultrasound results.
What is a venous outflow disorder?
First of all, let's understand the anatomy. Imagine a spine. Veins run next to it, through which blood should flow freely from the head down. If the vertebrae are displaced, then the veins can be pinched, deformed, and because of this their capacity is reduced. Blood accumulates in the posterior cranial fossa.
With normal intracranial pressure, there is no outflow of blood through the compressed vessels. In order for the outflow to be restored, the blood must flow with greater pressure, that is, the pressure must increase. We all know that increasing blood pressure is not beneficial for the body, to put it mildly, and here it is a necessary measure to restore blood circulation, otherwise more serious problems will arise.
In the long term, stagnation of blood and impaired circulation in the brain are fraught with many bad consequences, but there is no need to be afraid. The human body is excellent at recovering on its own, plus it informs in advance about possible problems with unpleasant and even painful sensations. Therefore, you need to listen to your body and simply help it be healthy, which is not difficult to do.
After an increase in pressure, a sharp outflow occurs through the posterior or jugular veins. Changes in the condition of the jugular veins are easier to see on an ultrasound than changes in the vessels near the spine, on the back of the neck.
Helpful advice
When you go for an ultrasound, be sure to ask to look at the jugular veins. If they write to you that they are dilated, this is an accurate sign of venous stagnation and circulatory disorders in the brain.
Reference. It is more difficult to see a similar sign of a disorder in the spine. Therefore, it may be that the problem is already there, but it is not yet visible when examining the back of the neck.
The jugular veins dilate and lose elasticity when large volumes of blood are dumped through them. As a result, blood circulation worsens even more, and the body signals this with pain.
Violation of venous circulation in the brain
The brain is a complex structure, its normal functioning depends on the state of blood circulation. In addition to the need to deliver oxygen and glucose to the nervous tissue, the outflow of venous blood and the removal of toxins with it, the result of cell activity, is important. If this process is disrupted, chronic venous insufficiency of the brain is formed.
A peculiarity of the vessels of the brain is the course of the veins: it does not coincide with the direction of the arteries, and a network is formed that is independent of them. If the outflow of blood through one of the vessels is impaired, venous blood is directed to the other, and compensatory expansion occurs. A prolonged decrease in tone leads to vascular atrophy, they collapse, and the risk of thrombosis increases. Dilated vessels contribute to the development of venous circulation insufficiency, the functioning of the valves is disrupted, they do not close tightly, and the direction of blood flow is disrupted.
Stages of the pathological process
The following stages are distinguished during cerebral venous insufficiency:
- latent: no clinical symptoms, no complaints;
- cerebral venous dystonia: some symptoms are observed: headaches, weakness;
- venous encephalopathy: severe symptoms caused by organic lesions are observed, venous outflow is impaired in all areas of the brain, there is a high risk of hemorrhages from dilated vessels.
Classification
There are chronic and acute variants of venous circulation in the brain. Chronic include venous congestion and venous encephalopathy, acute include venous hemorrhage, thrombosis of the veins and venous sinuses, thrombophlebitis.
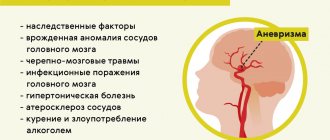
Causes and risk factors
Insufficiency of cerebral venous circulation can be caused by diseases or individual characteristics of the patient. The most common causes of pathology:
- neoplasms in brain tissue can cause disruption of venous outflow;
- head injuries that impair blood circulation to the brain;
- injuries during childbirth;
- hematomas formed as a result of stroke, atherosclerosis, bruises and other causes contribute to the formation of tissue edema, which complicates the outflow of blood from the affected area;
- blood clots and embolisms narrow the lumen of the vessel or completely close it, preventing the movement of blood;
- diseases of the spinal column, in which deformed sections of the canals compress the vessels and disrupt blood flow, also cause venous insufficiency;
- vascular features: hereditary predisposition and impaired development of veins can provoke the development of a violation of the outflow of venous blood.
Circulatory disorders can be physiological and occur when coughing, sneezing, or physical strain. Such short-term deviations do not cause significant harm to health.
One-time attacks of cerebral circulatory disorders do not cause serious consequences for the body. However, prolonged blood stagnation can contribute to the development of serious consequences. The following risk factors increase the likelihood of cerebral venous insufficiency:
- frequent stress;
- smoking;
- alcohol abuse;
- prolonged dry cough;
- professional singing;
- hypertension;
- heart failure;
- reading in the wrong position
- professional swimming;
- frequent wearing of clothes that compress the neck;
- chronic rhinitis:
- work in high-altitude, underwater, underground professions;
- office work that involves staying in a position with the head tilted or turned;
- frequent physical activity of high intensity
Clinical manifestations
Disturbances of venous circulation, as a rule, are genetically determined. Currently, the role of the initial tone of the veins in the formation of venous discirculation is undeniable. Constitutional and hereditary factors are key for the development of venous dyshemia. Patients with a family “venous” history usually have several typical manifestations of constitutional venous insufficiency - varicose veins or phlebothrombosis of the lower extremities, hemorrhoids, varicocele, impaired venous outflow from the cranial cavity, esophageal varicose veins. Pregnancy is often the trigger.
Typical complaints:
- morning or afternoon headache of varying intensity;
- dizziness, depending on changes in body position;
- noise in the head or ears;
- visual disturbances (decreased visual acuity, photopsia);
- “tight collar” symptom - increased symptoms when wearing tight collars or ties;
- “high pillow” symptom - increased symptoms when sleeping with a low headboard;
- sleep disorders;
- feeling of discomfort, “fatigue” in the eyes in the morning (symptom of “sand in the eyes”);
- pastiness of the face and eyelids in the morning (with a pale, purple-cyanotic tint);
- mild nasal congestion (outside the symptoms of acute respiratory infections);
- darkening of the eyes, fainting;
- numbness of the limbs.
Signs of impaired cerebral venous blood flow are related to weather conditions. Headaches are poorly controlled by analgesics; often some relief is brought only by a change in body position - in a horizontal position, venous blood flow is redirected along collaterals - bypassing the affected vessel.
The patient’s psyche changes in such a way that minor experiences can lead to neuroses. Tearfulness increases, the patient often breaks into a scream. Mania and depression are observed. Severe damage leads to psychosis, accompanied by hallucinations and delusions; this can make the patient dangerous to himself and others.
Diagnostics:
- radiography determines the strengthening of the pattern of the veins of the skull, which indicates the presence of a pathological process;
- angiography is a contrast method for diagnosing blood stagnation, determining the patency of blood vessels;
- computed tomography and magnetic resonance imaging make it possible to accurately determine the presence of a pathological process in the brain, as well as in surrounding tissues;
- ultrasound examination of the veins of the brain and neck;
- rheoencephalography is a functional diagnostic method that assesses the condition of blood vessels;
- An increased level of pressure in the ulnar vein allows one to suspect abnormalities in the vessels of the brain.
Therapy is complex and includes several areas
- drug treatment;
- non-drug treatment: physiotherapy, massage, physical therapy;
- surgery.
Drug therapy
The following drugs are used to normalize cerebral circulation:
- venotonics strengthen the vascular wall, reduce permeability, have an analgesic effect, and eliminate inflammation;
- diuretics to eliminate swelling;
- neuroprotectors improve nutrition and metabolism of the brain;
- anticoagulants to thin the blood and prevent thrombosis;
- vitamin therapy (vitamins B and PP).
Non-drug treatment
There are a number of non-drug therapies that are effective as an additional treatment method and improve vascular tone. However, before treating impaired cerebral venous outflow with their help, it is necessary to assess individual risks and contraindications: in some cases, such procedures can lead to the opposite effect and worsen the patient’s condition.
Applicable:
- head and neck massage;
- oxygen therapy;
- foot baths;
- physical therapy: breathing exercises, neck exercises, yoga classes.
Intern of the ophthalmology department Gurlo A.I.
Head of the department ophthalmological department Rudova
Symptoms of impaired venous outflow
Headache
The most common symptom is pain due to increased intracranial pressure. The blood does not leave the head on time, and new portions of it continue to flow - the pressure rises, the body signals this with a headache.
A case from the practice of Dr. Shishonin
The man was diagnosed with migraine and prescribed medication. The patient took the pills with discipline, but there was no noticeable improvement. Migraine attacks did not become less frequent and were often as severe as before starting to take the drugs. The attack was very difficult to relieve with analgesics; you had to take the maximum allowable doses, and even they did not always work. The pain went away on its own after some time.
Dr. Shishonin recommended going for an ultrasound under the compulsory medical insurance policy and asking to look at the jugular veins. An ultrasound showed that they were dilated. The cause of the migraine became clear - increased intracranial pressure.
After conservative non-drug treatment, improvement occurred within two months.
Extreme migraine
A very painful symptom occurs due to loss of elasticity of the jugular veins. Up to a certain point they can withstand the increased load, and then they can no longer cope. Swelling appears in the brain stem. They are not yet dangerous to human life and health, but they cause severe pain in the ternary nerve.
This is an extreme degree of migraine, it is almost impossible to tolerate and difficult to relieve with analgesics. A person becomes incapacitated, no matter how strong his will is. In addition, nausea occurs, the patient is physically unable to drink liquids or eat food. A migraine can last a day and goes away on its own when the pressure rises to such an extent that blood discharge does occur. If such conditions are repeated frequently, it becomes potentially dangerous.
Ptosis of the eyelid
A case from the practice of Dr. Shishonin
The person suddenly developed ptosis and the mobility of the eyelid was impaired. The hospital carried out a full examination - a microstroke was not confirmed, and no tumor was found.
An ultrasound scan examined the veins in the neck and revealed gross venous congestion. Conservative treatment without pills gave results after six months. If a person had paid attention to the headaches that he often had earlier, the problem could have been solved faster.
Labored breathing
This symptom itself is ambiguous; there can be many reasons. But if it is accompanied by regular pain in the back of the head or temples, then the cause is most likely venous stagnation.
Lack of air due to a violation of venous outflow can occur either unexpectedly and without cause (not during physical activity, not in a stuffy room), or, as they say, out of the blue - during a walk, in a well-ventilated room. If such situations recur, and under different conditions, you need to check and treat the neck first.
What else you need to know about symptoms
There are many signs of circulatory problems. Any discomfort in the head, neck, chest, or upper back may indicate this problem. You need to undergo an examination, and in any case it will be useful to do simple exercises. Unlike pills, carefully performed gymnastics and gentle self-massage have no side effects, that is, in any case the condition will not worsen.
The main principle of the doctor is Primum non nocere (“First of all, do no harm”). Therefore, Dr. Shishonin recommends making maximum use of the natural recovery abilities inherent in our body.
Left artery lesion
Hypoplasia can occur in both the right and left vertebral arteries. In this case, the left-sided pathology is not immediately expressed, since this blood vessel is physiologically wider than the right one and its dysfunction can be compensated for a long time by the body independently. Often, symptoms appear only during exacerbation of chronic diseases, for example, atherosclerosis, hypertension, etc.
Over time, symptoms will intensify along with age-related changes in the tissues and organs of the human body. The main symptom of hypoplasia of this vessel is cephalgia, spreading to the cervical spine.
As the vertebral arteries narrow, compensatory anastomoses are formed in the body - vascular anastomoses. Blood subsequently flows through them in a roundabout way, bypassing the hypoplastic areas of the circulatory system.
- Hypoplasia of the left vertebral artery: what is it, causes and treatment features
The clinical picture of hypoplasia of the left transverse sinus is determined by the degree of underdevelopment of the left vertebral artery. A mild form of pathology practically does not manifest itself, while with a severe degree of changes, the anomaly is visualized on MRI images. Its presence is also indicated by night headaches, nausea, and vomiting.
Severe hypoplasia of the cerebral sinuses can cause thrombosis, papilledema, and loss of visual fields.
How can you help yourself without pills?
There are two simple ways. The first can be used by each person independently without preparation. The second one is a little more difficult, but regular viewers and readers of Dr. Shishonin will master it very quickly.
It is better to use both methods: working on the points on the sides of the front of the neck, and working under the back of the head. This way, you will not only get rid of headaches and other symptoms of impaired venous outflow, but you will also feel more energetic, your mood and memory will improve. The main thing is to regularly devote time to yourself and help your body recover. The capabilities of the human body are almost limitless, but you need to develop them by doing gymnastics and self-massage.
Self-massage in the collarbone area
Working out certain points improves blood flow through the jugular veins. This will help immediately reduce or completely eliminate headaches caused by blood stagnation. If you do this self-massage regularly, the veins will become more elastic, resilient and begin to work like pumps, draining blood from the head in time. Accordingly, headaches will stop without taking medications. This is important because any drugs have side effects, including those delayed over time. It is imperative to use the body’s natural ability to heal itself.
Self-massage technique step by step:
- Place two fingers in the middle of the collarbone - just above the jugular fossa.
- Lightly press on the point - the pressure should not be strong, but should feel pleasant.
- Start working the point with circular rotations clockwise or counterclockwise - whichever is more comfortable for you.
- Do 20-30 rotations.
- Move to the other side of the neck and repeat steps 1-4.
Important! Please note again that you cannot put pressure on the point. Throughout the self-massage there should be pleasant sensations, and after its completion - a feeling of vigor or pleasant relaxation (depending on the time of day). This is a marker that you are doing everything right.
How often to perform
Everything is individual here. For some, it will help the first time and the headache will subside for a long time, for others, several sessions in a row are needed, and then maintain the condition of the veins with preventive self-massage.
If you have a diagnosed migraine, you need to start working on the point as soon as the first signs of pain appear. As soon as there is the slightest hint of imminent pain, we immediately do it. This will certainly reduce the intensity of pain and will most likely stop its further development. That is, a terrible migraine attack, for which even pills don’t help, simply won’t happen, your head will hurt a little, but it will go away after working on the clavicular point.
To prevent migraines, if they happen several times a month or a year, it is useful to do self-massage every week. This will help maintain the elasticity of the veins and blood vessels, so the blood will circulate correctly, without stagnation. The risk of not only headaches, but also increased intracranial pressure will be reduced.
Working out the back of the neck
As we have already found out, the problem arises due to compression of blood vessels, which is a consequence of the incorrect position of the vertebrae. Gymnastics will help solve and even more so prevent such a situation. For urgent help, you can gently influence the vessels. Let's take a closer look at how to do all this.
Gymnastics for the neck
Gymnastics should be performed regularly. Spend just 3-5 minutes a day and you will almost 100% protect yourself from headaches. A bonus is the prevention of high blood pressure – both intracranial and arterial.
There are many sets of exercises for the neck; you can see in detail, with step-by-step instructions and explanations, in Dr. Shishonin’s publications on cervical osteochondrosis. You've probably already read these articles and watched the videos, so let's briefly remind you. Tilts and rotations of the head, movements of the neck should not be performed abruptly, but carefully, so that there are pleasant sensations similar to those you experience when stretching after sleep.
Triggering a reflex response
The back of the neck can be treated with a piece of ice. The temperature effect causes a reflex reaction of the vessels: they react by restoring their shape. Dr. Shishonin spoke in detail about these techniques in specialized articles on cervical osteochondrosis.
Here we just remind you that you need to work with ice carefully. Don’t be afraid, you physically won’t be able to harm yourself, but don’t overdo it, otherwise the effect will be worse than from a delicate influence.
What is hypoplasia? Causes, signs, treatment of hypoplasia
Hypoplasia is the underdevelopment of any organ or tissue - this is a common and main feature of pathology, be it hypoplasia of the kidneys, brain, or hypoplasia of a segment of the right or left vertebral artery.
In humans, underdevelopment of individual organs most often occurs. So, this pathology can affect the brain, but not the entire central nervous system, or one lung without involving the second and upper respiratory tract.
Pathology occurs due to a malfunction during intrauterine development. The most common causes of hypoplasia development:
- a failure that occurs during the initial formation of germ cells;
- incorrect intrauterine position of the fetus;
- scanty amount of amniotic fluid;
- bad habits of the expectant mother - smoking, drinking alcohol and drugs (most often they cause brain hypoplasia);
- infectious diseases of women during pregnancy;
- abdominal injuries of a pregnant woman;
- exposure to physical factors - elevated temperature, radiation;
- exposure to toxic compounds and harmful metabolic products.
Hypoplasia is not always detected on time. The success of diagnosis depends on the degree of underdevelopment and which organ is affected. Thus, to identify signs of tooth enamel hypoplasia in a child, an examination by an experienced dentist is often sufficient. While diagnosing renal underdevelopment will require additional instrumental examination methods.
Underdevelopment of the entire organism is called dwarfism.