Types and classification
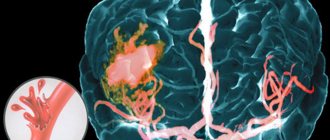
A major stroke occurs when large arteries are damaged, including the carotid arteries - they take part in the blood supply to the cerebral hemispheres. As a result of their blockage or rupture, the power supply to one or even two hemispheres may completely stop. This leads to a sharp deterioration in nervous activity, and in the absence of medical assistance within the first few hours, to death. It is important to determine the type of stroke and its causes - these factors influence the selection of further treatment and rehabilitation after a stroke.
Ischemic major stroke
Ischemic stroke occurs in 80% of patients. Its main reason is the deterioration of blood conductivity through the vessels, while their walls remain undamaged. Ischemia is oxygen starvation of tissues, which is especially dangerous for the brain. This type of stroke can occur suddenly or develop gradually, against the background of the main predisposing factors:
- blockage of a vessel by a thrombus, including atherosclerosis and plaque formation;
- vascular spasm, as a result of which blood cannot flow freely to the brain tissues;
- a sharp decrease in blood pressure - in such conditions, a small amount of oxygen-enriched blood reaches the nervous tissues.
With an ischemic stroke, there is still a chance of full recovery. If the walls of the vessel remain intact, in the first few hours all possible measures should be taken to restore blood circulation.
Extensive hemorrhagic stroke
A hemorrhagic stroke is a stroke that occurs when an artery ruptures. Its second name is non-traumatic cerebral hemorrhage. This is a dangerous phenomenon that can be fatal even if emergency care is provided in a timely manner. An extensive hematoma deprives brain tissue of the ability to receive and transmit nerve impulses, which can result not only in deterioration of memory, attention, skills and reflexes, but also coma and complete suppression of nervous activity.
There are several types of hemorrhagic stroke, which differ in the location of the hematoma and the degree of danger for the patient.
- Intracerebral hemorrhage is the most common type. Blood enters the brain matter and damages nerve cells that are responsible for various skills and functions in the human body. Risks to the patient's life are present, but they are minimal compared to other types of hemorrhagic stroke. The main causes are hypertension (high blood pressure), atherosclerosis and thrombosis. P
- Subarachnoid hemorrhage is a pathological condition in which blood enters the subarachnoid space, between the membranes of the brain. It often occurs spontaneously and can be fatal, even with prompt medical attention. Among the causes of subarachnoid hemorrhage, in addition to hypertensive crisis, are smoking, excess weight and alcohol abuse - all these factors lead to weakness of the vascular walls.
The danger of hemorrhagic stroke is that not every patient is able to fully restore lost skills. Even if all the doctor’s recommendations are followed, the nerve tissues undergo necrosis and cannot perform the function of transmitting nerve impulses.
Brainstem stroke
Both ischemic and hemorrhagic strokes can be located in the brainstem center. Here are vital centers that are involved in the regulation of breathing, swallowing, and heart rate. If blood enters this area, it can be instantly fatal due to the cessation of breathing and heartbeat.
Main types of stroke
There are two main types of apoplexy: hemorrhagic and ischemic.
Hemorrhagic stroke is a severe lack of normal blood circulation or, in other words, a stroke with rupture of blood vessels and a large amount of blood entering the brain.
The cause of this type of stroke can be poisoning, lack of vitamins, anemia, bone problems, or an aneurysm. And the forecasts will be disappointing. This type of stroke is the most dangerous and difficult to tolerate, which is why the number of people who died from this disease is high. If you're lucky, you can live after this for just a couple of days. Brain damage in such a situation is not compatible with life, however, they are different.
Read also: Do people die from strokes?
Ischemic stroke is the absence of normal blood circulation in a severe form or, in other words, stroke with injury to brain tissue , disruption of its functioning due to the fact that the flow of blood to the whole brain or its parts is stopped. In other words, a cerebral infarction. This type of stroke is the most common and has a high mortality rate. If a person has experienced an ischemic stroke 1 or even 2 times, then it is more than possible that he will not be able to endure the third. According to statistics, most patients fall into a state between life and death, without responding to external factors, for several days and, as a rule, do not come out of it.
Types of ischemic stroke include:
- Transistor attack of ischemic nature. As a result of the attacks, neurological disorders occur that disappear within 24 hours.
- "Minor strokes" They are similar to a full-blown ischemic stroke, but their symptoms subside within two days to three weeks.
- Progressive ischemic stroke, characterized by the development of stroke symptoms over several days. Functional restoration is not complete.
- Total ischemic stroke (completed). An established cerebral infarction with not fully regressing processes performed by the brain.
Causes and risk factors
A major stroke can happen suddenly, but in some cases symptoms worsen over several hours. An attack can occur in any person, regardless of gender and age. However, there are a number of predisposing factors that reduce the strength and elasticity of the vascular walls, thereby increasing the likelihood of developing a stroke. These include:
- old age (over 50 years) - over time it is worth paying more attention to proper rest, proper nutrition and physical activity;
- chronic hypertension - patients are advised to monitor their well-being and regularly measure blood pressure;
- any heart disease - if it worsens, there is a risk of increased or decreased pressure, deterioration in the quality of vascular walls, various types of arrhythmia (regular examinations are required);
- ischemic attacks - often occur as precursors of a stroke or heart attack;
- type and schedule of work, including high levels of nervous tension, night shifts and hazardous working conditions;
- bad habits - smoking reduces the strength and elasticity of blood vessels, causing surges in blood pressure;
- overweight;
- vascular diseases, including stenosis (narrowing) of the arteries that supply the brain;
- hereditary predisposition - a history of stroke in relatives.
To reduce the likelihood of a major stroke, doctors at the Clinical Brain Institute recommend undergoing regular examinations for any pathologies of the heart and blood vessels, as well as in old age. It is also important to adhere to a healthy lifestyle, choose proper nutrition and perform light physical activity. Fatty foods of animal origin are the main source of cholesterol. It accumulates on the vascular walls and can form plaques that narrow the lumen of the arteries.
Another reason for major strokes and complications after them is the lack of early diagnosis and timely treatment. The most effective period during which it is important to see a doctor is the first two hours. The Clinical Brain Institute has the necessary equipment, and specialists have extensive experience in treating strokes of any type, which guarantees maximum chances for a successful recovery.
Ischemic cerebral stroke: prognosis and consequences
Cerebral stroke, or “brain stroke,” is the number two “killer” in the structure of overall mortality worldwide: 25% of men and 39% of women die due to it.
More often, in four cases out of five, it is ischemic in nature, that is, the blood supply to the brain is disrupted due to blockage of the arteries by a thrombus or embolus.
Read also: Case history of stroke
The brain is such a delicate and demanding structure of the body that with a weight of 2% of body weight, it consumes 1/5 of the volume of incoming oxygen and 17% of all glucose. Even a short-term disruption of the blood supply to a small area of the brain does not go away without leaving a trace. If ischemia continues for more than 5 minutes, irreversible changes in the cerebral cortex occur. When the focus is localized in the midbrain, the cells die within 10 minutes of ischemia, and in the medulla oblongata - within 25 minutes.
What are the consequences and prognosis of ischemic cerebral stroke - read in this article.
Clinical picture
A major stroke occurs with damage to a large area of the brain. The clinical picture is pronounced, and the damage poses a danger to the patient’s life. It is important to seek emergency help if the victim exhibits the following symptoms:
- a sharp decrease in hearing and vision, impaired coordination of movements, inability to concentrate;
- acute headache, dizziness;
- nausea and vomiting;
- redness of the skin and mucous membranes or their pallor;
- decreased skin sensitivity, often on one side of the face or torso, muscle paralysis;
- the appearance of memory lapses;
- fainting.
With a major stroke, there is still a risk of developing coma. This is a condition in which the victim does not respond to any external stimuli, but his breathing and heartbeat continue. The coma can last for a long time, and the chances of further recovery depend on this.
What determines the prognosis after three strokes?
Doctors have identified factors influencing a patient’s survival after a third stroke:
- Constantly present, practically unchangeable indicators: the severity of the patient’s symptoms of the disease, the type of disease, the location of the stroke, the age of the patient.
- Variables: biochemical parameters of blood plasma, blood pressure, presence of temperature in the patient.
By monitoring the second group of indicators, doctors are in some cases able to cure a patient who has suffered 3 strokes. But this happens quite rarely.
With the third stroke, the consequences most often lead to the death of the patient within 2-5 days. If the person survives, complications are possible:
- Brain swelling.
- Memory loss.
- Development of seizures.
- Paralysis.
- Severe headache, cerebral hemorrhage.
- Impaired coordination of movements.
- Aphasia (loss of speech and writing skills).
In addition to these phenomena, peripheral neuropathy, the development of psychosis and coma may be observed. Each of these complications has its own symptoms, which doctors must take into account. For example, cerebral edema is characterized by headache, neck numbness, dizziness, blurred vision and other symptoms.
Cramps can occur in any muscle group with extensive bleeding in the brain.
Most often, after the third apoplexy, the patient develops paralysis of the limbs, which passes without atrophy of the muscle structures.
Aphasia is a consequence of damage to the left half of the brain. During recovery, a person will need the help of a speech therapist, because... he loses his speech skills and cannot listen normally. To restore all speech and writing skills, the patient must begin treatment within the first 2 weeks after the stroke.
Test for rapid diagnosis of major stroke
At home, you can identify the first signs of cerebrovascular accident and prevent the development of a major stroke. They can appear several hours before the attack, and it is important to distinguish them from the normal state. The patient may not understand the danger of what is happening and may be in good health, so primary diagnosis is the task of those around him. Doctors at the Clinical Institute of the Brain offer to familiarize yourself with simple tests that should be performed immediately if you suspect a stroke - they will help you seek medical help early and increase your chances of a full recovery.
- The first way to detect a stroke is to ask the person to smile. When cerebral circulation is impaired, one of the corners of the mouth remains drooping.
- The second way is to raise both arms in front of you and hold them for a few seconds. If normally this exercise does not cause difficulties, then during a stroke one arm either does not rise or immediately falls down.
- The third way is to ask to repeat a simple sentence. The person's speech may become unintelligible. You can also ask simple questions about the location of the victim, his name and date - he will not be able to give a clear answer to them.
- The fourth way is to direct the light source into the eyes. During a stroke, one of the pupils does not respond to light, while the other will constrict and then dilate in less intense light.
It is important to understand that not all the first signs of a stroke may appear in one person. If at least one of the points coincides, it is important to seek emergency medical help. At an early stage, there is a possibility of completely preserving brain functions and not losing nerve connections.
How is ischemic different from hemorrhagic?
To understand the difference between these two types, it is necessary to understand more carefully what they are.
An ischemic stroke , simply put, is when blood, due to a blood clot or other obstruction, does not flow to the brain tissue, as a result of which the tissue is weakened and does not “work.”
A hemorrhagic stroke is when part of the brain dies and the blood that should go there goes to the other side of the brain. Because too much blood accumulates, the vessels dilate and burst, causing bleeding in the brain.
Diagnostic and treatment methods
Treatment tactics depend on the type of major stroke, the patient’s age, concomitant diseases and other factors. With the hemorrhagic type, it is important to eliminate the source of bleeding, and some patients may require surgery to remove the hematoma or aneurysm. For ischemic stroke, therapy is carried out in several directions:
- correction of breathing and heartbeat;
- elimination and prevention of brain swelling;
- thinning the blood and preventing the formation of blood clots;
- symptomatic treatment aimed at relieving seizures, fever and other clinical signs.
The Clinical Institute of the Brain has all the necessary conditions for the treatment and rehabilitation of patients with strokes. At the first stage, all procedures must be carried out in a hospital, under round-the-clock supervision of doctors. In addition, in the first weeks the likelihood of a second attack is increased, and it is important not to miss its first symptoms. After complete stabilization, treatment continues at home, with mandatory examinations and constant monitoring of the patient’s condition.
Early and late diagnosis of the disease
The early detection of circulatory disorders in the brain structures has a great influence on the final result of rehabilitation. If this is successful, the doctor first assesses the patient’s condition using the following indicators:
- The number of points is determined using a special stroke scale.
- The time from the onset of the disease is recorded.
The patient is examined using MRI, determining the volume of tissue affected by the disease. After this, the patient is diagnosed and the prognosis for rehabilitation is considered. In fact, this is an attempt to predict what may happen to a patient in the first month after a stroke.
The sum of points on the disease scale allows doctors to predict what will happen to the patient after another stroke. The patient's chances of recovery increase sharply if he is under 40 years old and has a spouse. A low (compared to other patients) body temperature during the acute stage of the disease can give a chance for successful rehabilitation.
Read also: Stroke and pregnancy
Rehabilitation conditions improve if, in the first 7 days after a stroke, a person experiences positive dynamics, indicating some improvement in the patient’s condition. Such patients quickly restore speech skills and motor functions.
When diagnosing a stroke in a person late (it is carried out 30 days after the onset of the disease), doctors assess the condition and the chances of recovery based on factors such as:
- Manifestations of impaired motor function, speech disorder (at the same time, vision damage is possible), a drop in the patient’s mood, a change in his behavior.
- A person who has suffered a stroke experiences difficulties with self-care and movement, and cannot go to the store or drive a car on his own.
- After the third apoplexy, most patients cannot work in the same place.
After taking into account all these factors, doctors make a prognosis for the recovery of a particular patient after a stroke. If treatment is possible, the patient is prescribed the appropriate drug. Full recovery occurs in only 12-15% of the total number of patients with stroke.
An unfavorable outcome occurs when the patient has impaired perception and consciousness, persistent paralysis of the limbs, and signs of urinary incontinence.
Recovery after a major stroke
An important stage is the restoration of skills lost after a stroke. These can include the simplest functions, including speech, writing, and self-service in everyday life. A comprehensive program may include several stages:
- motor rehabilitation, development of damaged limbs, development of fine motor skills;
- speech, including regular classes with a speech therapist;
- physiotherapy is a set of techniques to improve blood circulation and improve brain nutrition.
The Clinical Brain Institute offers individual treatment and recovery programs after a major stroke. Here you have the opportunity to undergo a full examination and rehabilitation in a hospital setting, and then undergo examinations and attend useful procedures (physical therapy, hardware treatment, electrical and magnetic stimulation). A neuropsychologist, speech therapist, massage and physical education specialists work at the Clinical Institute of the Brain. However, exercises at home also play an important role in rehabilitation and should be performed by the patient independently.
Clinical Brain Institute Rating: 4/5 — 11 votes
Share article on social networks
Ideas about the pathogenesis of stroke from the perspective of cardioneurology
Cardioembolic stroke
is one of the most common pathogenetic subtypes of ischemic cerebrovascular accidents.
According to modern research, cardiogenic embolism causes 20-30% of all ischemic strokes, and this number may increase as cardiological diagnostic methods are introduced into clinical practice. To date, more than 20 cardiac disorders associated with embolic complications have been described [4]. These are non-rheumatic atrial fibrillation, myocardial infarction, thrombosis of the left ventricle of the heart, mitral stenosis, endocarditis and other, rarer heart diseases. Not all of these pathological conditions can be detected by physical examination. Latent paroxysms of atrial fibrillation, mitral valve prolapse with myxomatous degeneration of the leaflets, aneurysm of the interatrial septum, atheroma of the aortic arch, myxoma of the left atrium, patent foramen ovale, thread-like fibers of the mitral valve and other heart pathologies do not manifest characteristic, specific symptoms. It can be difficult to detect these violations even with targeted research. Diagnosis and correct clinical assessment of heart diseases that can lead to cerebral complications are also important because cardiocerebral embolism is a pathological process and not a completed event. Transcranial Doppler monitoring of the middle cerebral arteries allows us to detect microembolic signals in more than half of patients who have suffered a stroke due to the mechanism of cardiogenic embolism. In approximately 40% of patients, such signals are detected long-term (months and years) after the stroke [2,4]. A feature of cardioembolic stroke should also be considered the heterogeneity of the embolic substrate. Fibrin-erythrocyte thrombi, platelet aggregates, tumor particles, myxomatous elements, calcifications and atheromatous particles, fragments of valve vegetations can act as emboli. The morphological diversity of the substrate influences the treatment tactics of patients, which involves the use of both conservative and surgical methods. But conservative tactics, depending on the results of the examination, become very differentiated. It may include not only the prescription of anticoagulants and antiplatelet agents, but antibacterial therapy (endocarditis), the use of statins, antiarrhythmic drugs (paroxysmal atrial fibrillation). Surgical treatment brings encouraging results when detecting a cardiac tumor and patent foramen ovale [3,4,5]. In some cases, there is no alternative to heart valve replacement in severe endocarditis. Endovascular occlusion of the left atrial appendage is promising in order to prevent cardiogenic embolism in atrial fibrillation. It is obvious that with the expansion of knowledge about the nature of cardioembolic stroke, the possibilities of preventing and treating brain damage will increase. Hemodynamic stroke
accounts, according to various authors, from 8 to 53% of all ischemic strokes.
Such significant differences in the frequency of this pathogenetic subtype of ischemic stroke reflect the magnitude of unused diagnostic capabilities in determining the mechanisms of cerebral ischemia. A hemodynamic stroke is based on a discrepancy between the blood supply needs of the brain and the capabilities of the cardiovascular system. The formation of clinical symptoms of stroke occurs against the background of a long-term deficiency in the blood supply to the brain, caused by changes in its vascular system. A decrease in autoregulation of cerebral circulation, adaptation to the action of meteorological factors, physical and emotional stress, leads to a direct dependence of cerebral hemodynamics on the efficiency of the heart. Under these conditions, any pathological conditions that lead to a decrease in cardiac output (coronary insufficiency, arrhythmia, increased load on the myocardium) are inevitably accompanied by cerebral ischemia. Hemodynamic stroke is always the result of circulatory decompensation, in which the brain suffers as one of the main consumers of cardiac output [2,3]. Data obtained at the Scientific Center of Neurology of the Academy of Medical Sciences indicate the priority role of cardiac disorders in hemodynamic stroke [4]. As a result of cardiac examination, a variety of heart pathologies are detected in 70% of patients with hemodynamic stroke. Stratification of cardiogenic causes of hemodynamic stroke demonstrates that the most common causes of cerebral ischemia are silent myocardial ischemia and persistent atrial fibrillation. Next in frequency: sick sinus syndrome, paroxysmal atrial fibrillation and acute myocardial infarction. Less commonly, hemodynamic stroke is caused by: frequent ventricular extrasystole, transient atrioventricular block, ventricular fibrillation and pacemaker failure. All of these disorders can cause a reduction in cardiac output. In most cases, transient, asymptomatic cardiac disorders, revealed during cardioneurological examination, are associated with the hemodynamic mechanism. It should be noted that not only cardiac pathology underlies hemodynamic stroke. In some cases, decompensation of cerebral hemodynamics is associated with disturbances in the autonomic regulation of vascular tone and heart function. An example is hypotensive crises in patients suffering from parkinsonism. The hemodynamic mechanism of brain damage is also present in cases of stroke associated with arterial hypertension. The pathological basis of such damage is pathological processes in the arteries of the muscular type, occurring with their sclerosis, thickening and deformation. Hypertensive angioencephalopathy is the result of restructuring of the arterial system of the brain due to long-term hypertension. In hypertension, the entire cardiovascular system, and above all, the heart, is subject to remodeling. Left ventricular hypertrophy, dilation of the cavities of the heart, relative insufficiency of the valve apparatus, cardiosclerosis - lead to the formation of systolic and diastolic dysfunction. The result of remodeling is a decrease in hemodynamic reserve - the ability to maintain sufficient cardiac output under changing loads. Under these conditions, the immediate cause of stroke is most often a hypertensive crisis. An increase in the load on the myocardium leads to a decrease in minute blood volume, which in conditions of hypertensive angiopathy results in a hemodynamic ischemic stroke. Hemorheological stroke
is a special form of acute cerebral ischemia, which is based on altered blood properties.
Cerebral ischemia during hemorheological stroke is directly related to the blockade of microcirculation. Numerous factors lead to an increase in blood viscosity, among which the most important are: erythremia, hypercoagulation, hyperfibrinogenemia, hyperglycemia, dyslipidemia. Timely assessment and correction of these factors is absolutely necessary in both preventive and treatment programs aimed at compensating cerebral hemodynamics. Atherothrombotic stroke
is the most common and, as a rule, severe pathogenetic variant of stroke. Atherothrombosis usually affects large main arteries that have significant atherosclerotic changes. The absolute annual risk of stroke with stenosis of one carotid artery reaches 12–16% [5]. Large atheromas of unstable structure create favorable conditions for thrombus formation, which leads to artery obstruction. Timely diagnosis of atherosclerotic changes in the large arteries of the brain is one of the most important areas of cardioneurology. Assessing the degree of risk, feasibility and method of surgical intervention is possible only with a comprehensive examination of the state of the cardiovascular system.
Programs:
Assessment of rehabilitation potential
Movement restoration
Rehabilitation after stroke
Restoration of cognitive functions
Early (resuscitation) rehabilitation
Prevention of cerebral ischemia during antihypertensive therapy
Currently, there is no doubt that adequate antihypertensive therapy can prevent the development of cerebrovascular complications, including recurrent stroke [1,4,5]. However, in patients with cerebrovascular pathology there is a risk of neurological complications caused by a significant decrease in blood pressure when its level falls below the lower limit of autoregulation of cerebral circulation. There are a number of factors that determine the safe tactics of antihypertensive therapy in the post-stroke period. It has been established that in the acute period of stroke, the increase in blood pressure is compensatory in nature and is aimed at maintaining adequate perfusion pressure in the peri-infarction zone. Therefore, the optimal level of systolic blood pressure in the acute phase of ischemic stroke is 160-180 mmHg. Art. and diastolic blood pressure 95-105 mm Hg. Art., which is associated with a lower incidence of early and delayed cardiovascular and neurological complications and less pronounced residual neurological deficit. In patients who have suffered a hemorrhagic stroke, the risk of recurrent hemorrhages is directly dependent on the level of blood pressure: the minimum risk is found at 120/70 mm Hg. Art., lower values were not achieved in studies. On the contrary, after an ischemic stroke, blood pressure levels must be maintained slightly higher, and optimal blood pressure values depend on the condition of the great arteries. In the presence of occlusive atherosclerotic lesions of the carotid artery, the lowest incidence of complications and the best outcomes are recorded with a systolic blood pressure of 130-140 mm Hg. Art., at higher or lower blood pressure levels, the risk begins to increase. With bilateral stenosis of the carotid arteries of more than 70% of the lumen of the vessels, there is an inverse relationship between the level of systolic blood pressure and the risk of stroke. Due to the danger of iatrogenic cerebral ischemia, blood pressure is maintained at 160-170 mm Hg. Art. – this tactic brings the best results. In patients with long-term and high hypertension, cerebral circulatory failure can occur at relatively normal blood pressure levels, so it is very important to plan a safe range of its reduction during long-term antihypertensive therapy. Studies by the Scientific Center for Neurology of the Russian Academy of Medical Sciences have shown that with the relative preservation of the cerebrovascular adaptive reserve and the absence of pronounced damage to the main arteries of the head, it is permissible to reduce systolic blood pressure by 20%, and diastolic blood pressure by 15% from the initial drug-free level. During treatment, as a rule, blood pressure approaches the so-called “target” levels - 120 - 130 mmHg. However, for patients with clinical manifestations of cerebral ischemia, gross atherosclerotic changes in the main arteries, hypertensive angiopathy, this requires a longer time.