Before moving on to the issue of rehabilitation after neurosurgery and traumatic brain injuries, you need to have a clear understanding of both.
Traumatic brain injury (TBI) is a set of contact injuries (soft tissues of the face and head, skull bones and facial skeleton) and intracranial injuries (damage to the substance of the brain and its membranes), having a single mechanism and age of formation. TBI is the third most common cause of death in the country (after cancer and cardiovascular diseases).
Neurosurgical surgery involves surgical treatment of diseases of the central and peripheral nervous system that arise both as a result of TBI or independently. The consequence of severe TBI and any neurosurgical intervention is a disruption of brain function of varying duration and severity, requiring further rehabilitation under the supervision of a neurologist. The rehabilitation program after TBI is highly individual and depends on the severity of the injury, the period of occurrence and the nature of the complications.
Differentiation of traumatic brain injuries
According to communication with the external environment, traumatic brain injuries, like fractures, can be open (penetrating, non-penetrating) and closed.
According to morphology, TBIs are divided into subtypes:
- Shake. The most gentle at first glance, but also the most insidious damage. The period of pronounced symptoms is up to several days.
- Squeezing. Pressure on the brain is exerted by a hematoma or the presence of air in the skull, or less often by a foreign body.
- Mild, moderate and severe brain contusion.
- Diffuse axonal damage - diffuse ruptures or tears of axons (coma with symptoms of brain stem damage).
- Subarachnoid hemorrhage is cerebral bleeding with a sharp headache and loss of consciousness in combination with hyperthermia and a meningeal symptom complex.
The combination of these injuries can be different, for example, bruise and compression or hemorrhage with bruise. Often there may be hemorrhage with the presence of a bruise and compression of the brain by the hematoma. Brain injury most often occurs at the site of impact, but often damage occurs on the opposite side of the skull - in the impact zone.
Traumatic brain injury
Preliminary consultation and registration: +7 (495) 433-11-30
Treatment of traumatic brain injury includes several stages: direct first aid, diagnosis and subsequent qualified treatment in a hospital, as well as possible rehabilitation actions and procedures at home. Often, the recovery period after a traumatic brain injury takes considerable time, but the right treatment and social rehabilitation regimen can minimize damage to health and preserve the patient’s fullness of life.
Rehabilitation at home has a number of advantages compared to being in a hospital:
- the recovery process is faster: the patient’s familiar environment and being among loved ones relieves him of stress and discomfort; recovery at home allows the patient to avoid an inconvenient and traumatic transfer to a medical facility
- home rehabilitation programs are significantly lower in cost than hospital stays, since treatment and rehabilitation procedures and consultations with specialists are directly paid for. The cost of a hospital includes a fee for the stay, hospital expenses for renting and maintaining premises, payment for expensive equipment (which in the vast majority of cases can replace mobile equipment)
- in home rehabilitation, the full range of therapeutic measures is used (physical therapy, massage, physiotherapy, mechanotherapy), as well as training in necessary household skills and handling of those everyday objects that the patient is used to using; family members can observe the entire rehabilitation process and also participate in it , receiving the necessary information about the patient’s health status and how to properly provide assistance and care
The rehabilitation program after a traumatic brain injury ranges from two weeks to one month:
"Intensive" (5 times a week / 1 month)
Program cost: 59,000 rubles
"Recovery" (5 times a week / 2 weeks)
Program cost: 33,500 rubles
“Optimal” (3 times a week / 1 month)
Program cost: 39,000 rubles
A multidisciplinary team works with the patient: an exercise therapy doctor, a neurologist, an exercise therapy instructor. If necessary, the patient can be examined and advised by a surgeon, traumatologist, nephrologist, endocrinologist, therapist, or psychotherapist.
Programs aimed at speech restoration:
"Twelve" (3 times a week / 1 month)
Program cost: 39,000 rubles
"Sixteen" (2 times a week / 2 months)
Program cost: 49,000 rubles
Programs aimed at restoring cognitive functions (memory, attention):
"Eight"
Program cost: 24,000 rubles
A speech therapist (or clinical psychologist) and a medical specialist (neurologist, exercise therapy doctor) work with the patient.
All specialists have valid professional certificates and experience in the field of rehabilitation.
The particular danger of traumatic brain injury is that a variety of disorders in the body caused by it can appear a considerable time after the traumatic event itself. Therefore, it is important to promptly pay attention to the appearance of symptoms indicating various neurological disorders that may be associated with a previous TBI. Such symptoms may be: headaches, nausea, dizziness, impaired consciousness, retrograde amnesia, constant fatigue, depressive mood.
Depending on the severity of the injury, three degrees of traumatic brain injury are also distinguished: mild, moderate and severe. The severity is determined using the Glasgow Coma Scale, which assesses the degree of impairment of consciousness; visual, speech and motor reactions.
The most common traumatic brain injury is among the socially and labor-active part of the population under the age of fifty. The main causes of TBI are associated with: road traffic accidents, criminal injuries, industrial accidents, sports and domestic injuries. In case of untimely treatment or insufficient rehabilitation actions, TBI often leads to disability of victims and loss of ability to work.
For older people, traumatic brain injuries associated with falling from their own height are common. The number of such injuries especially increases in the autumn-winter period, when precipitation and ice significantly increase the risk of a traumatic fall.
In elderly people, the severity of the injury often significantly exceeds the force of mechanical impact during injury. In addition, it is necessary to take into account possible complications of existing chronic diseases after TBI.
- If you would like to learn more about our programs and services, please call our consultant:
+7 (daily from 8 to 20 hours)
- Licenses
Symptoms for various degrees of TBI severity
The severity of TBI is determined by the Glasgow Coma Scale (assessing the patient’s eye opening, movement and speech): mild – 13–15 points, moderate – 9–12 points, severe – 3–9 points. In other words, three factors are taken into account: state of consciousness, vital functions, neurological symptoms. In this case, the patient’s condition is assessed as satisfactory, moderate, severe, extremely severe, terminal (between life and death). The more serious the injury and the deeper its penetration, the more difficult the patient’s recovery.
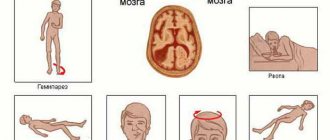
Symptoms of TBI with:
- Mild severity: headache (cephalalgia), dizziness, nausea and vomiting, sleep disturbance, irritability, fatigue.
- Moderate: speech impairment, partial loss of vision, paroxysms of the limbs, mental disorders, memory loss, heart rhythm disturbances, high-intensity cephalgia, increased frequency of respiratory movements while maintaining rhythm, loss of consciousness for up to several hours.
- Severe: convulsions, paralysis, hypo- or hypertonicity of muscles, lack of consciousness for up to several weeks, coma, critical impairment of vital functions, deep brainstem and cerebral disorders.
Severity of TBI
There are several degrees of severity of traumatic brain injury:
- Mild TBI - concussion and contusion of the brain - this type of injury is the most common and mild in clinical manifestations (short-term loss of consciousness, dizziness, nausea, and sometimes vomiting). Treatment involves strict bed rest for 7-10 days. Most often, the patient does not need rehabilitation measures;
- Moderate TBI - moderate brain contusion. Clinically manifested by switching off consciousness, impaired attention, disorientation in time, surrounding environment, epileptic seizures, which can manifest itself within 7-12 days after clearing consciousness;
- Severe TBI - severe contusion and compression. Clinically, there may be focal hemispheric and brainstem symptoms, hyperkinesis, increased muscle tone, followed by hypotension, motor excitation,. Focal symptoms regress slowly, often with pronounced consequences in the form of motor and mental disorders.
Initial consultation with a rehabilitation specialist
+8
Record
Periods, consequences and complications of TBI
The so-called traumatic disease includes three periods:
- Acute (duration 2 weeks – 2.5 months) – development of defense reactions to a damaging factor.
- Intermediate (duration 6 months – 1 year) – the process of lysis and repair in damaged areas.
- Long-term or final (duration 2-3 years, with complications - until the end of life) - completion of tissue degeneration and restoration of functions.
Complications of TBI in the acute phase:
- Impaired function of the respiratory system (respiratory depression and gas exchange disorders).
- Problems with central and regional (cerebral) circulation.
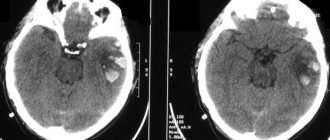
- Hemorrhagic complications (cerebral infarction, intracranial hemorrhage).
- Dislocation (displacement) of brain parts.
- Complications of a purulent-inflammatory nature: intracranial (abscesses, osteomyelitis, meningitis, encephalitis), extracranial (pneumonia, for example).
Possible consequences of TBI:
- Paralysis of the limbs (partial, complete) on one or both sides.
- Loss of vision, hearing, ability to speak, swallow, and breathe.
- Loss (weakening) of control over the function of the pelvic organs (the patient is not able to control the processes of urination and defecation).
- Tremor (shaking) in the limbs.
- Partial memory loss, deterioration of attention, changes in character and other consequences associated with higher nervous activity (usually after a coma).
In the long-term post-traumatic period, the development of epilepsy (acquired epilepsy), occlusive hydrocephalus, neuroses, and parkinsonism is possible. Also, cases of arachnoiditis and arachnoencephalitis (a disease of the central nervous system - serous (non-purulent) inflammation of the arachnoid membrane of the brain or spinal cord) are not uncommon.
Varieties
TBI is differentiated into closed and open forms. With the open version, the skin of the head and the wide tendon plate with which the muscles are fixed are damaged. The damage reaches the skull bones or deeper tissues. If the dura mater of the brain is damaged, then the open form is called a penetrating wound. With a closed version of TBI, the skin may be damaged, but the connecting plate is not affected.
Brain damage is classified into categories depending on the degree of the defect that occurs: mild, moderate (moderate) and severe. The Glasgow Coma Scale, the most commonly used system for classifying the severity of traumatic brain injury, assesses a patient's level of consciousness on a scale from 3 to 15. Diagnosis is based on the results of verbal, motor and visual responses to stimuli. It is believed that an index of 13 and above is a criterion for a mild disorder, from 9 to 12 for moderate (moderately severe), from 8 and below severe.
How to prepare for rehabilitation after a traumatic brain injury
Before rehabilitation can begin, the victim must receive nursing care and medication. At the first stage, assistance to the patient includes the following activities:
- emergency treatment by ambulance staff;
- intensive therapy;
- surgery if indicated;
- use of pharmacological agents.
Once the patient's condition is stabilized and not life-threatening, most people who have had a moderate or severe traumatic brain injury require rehabilitation. Patients may need to relearn basic skills such as walking or talking. The goal of rehabilitation interventions is to improve patients' ability to perform daily activities.
Rehabilitation therapy usually begins in the hospital. Recovery from a traumatic brain injury can continue in specialized rehabilitation centers or in public outpatient departments. The type and duration of rehabilitation is different for everyone, and depends on the severity of the TBI and what part of the brain was damaged.
What happens with a traumatic brain injury
A mild form of TBI is characterized by one or more of the following symptoms:
- attack of short-term loss of consciousness;
- loss of memory for events immediately before or after the injury;
- any change in mental status at the time of injury;
- focal neurological deficit.
Very often in such cases, the victim looks good outwardly, without realizing that functional problems are developing. Some people suffer from the long-term effects of TBI, known as post-concussion syndrome (traumatic encephalopathy). Persons suffering from this syndrome experience severe headaches, dizziness, decreased performance, weakness, insomnia and intellectual impairment.
Most traumatic brain injuries result in widespread damage to brain structures. The brainstem, frontal and temporal lobes are particularly vulnerable to local injury from contusions due to their location near bony prominences.
In addition to regulating the basic functions of excitation and inhibition, the brain stem is involved in the processes of attention and short-term memory. Trauma in this area can also lead to autonomic dysfunction: disruptions in metabolism, thermoregulation, respiratory and cardiac activity.
The limbic system helps regulate a person's emotional status. Connected to the limbic system are the temporal lobes, which are involved in many cognitive skills such as memory and language. Damage to the temporal lobes is associated with a number of behavioral disorders.
The frontal lobe almost always suffers from injury due to its large size and location at the front of the skull. The frontal lobe is involved in many cognitive functions and is considered the center of control of emotions and behavior of the individual. Damage to this area can lead to decreased criticality and increased impulsivity.