Surely you have encountered the phenomenon of floating spots in front of your eyes and glare. These are tiny shapes, lines, shadows or specks that feel like they are drifting across the surface of the eye. You may have wondered what this is and whether it is a dangerous symptom. Most often, the appearance of floating spots is normal and does not indicate problems with vision or eye condition. However, when this symptom becomes too frequent and is accompanied by glare, it may indicate a more serious problem.
Flares are flashes of light in the form of threads or stars. This can be either one flash in one visual zone, or multiple flashes in a wider area. Sometimes flashes may not be noticed because they most often appear on the side or in the periphery.
If you suddenly feel this unpleasant symptom, or the flashes and flickers become very frequent, you need to urgently make an appointment with an ophthalmologist to rule out any serious eye diseases.
What causes the floating fly effect?
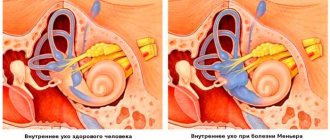
The vitreous humor of the eye is a clear gel that fills most of the eyeball and resembles raw egg white. Inside the vitreous are small clumps of protein that shift and move with your eyes. When these tiny clumps of protein cast shadows on the retina, the light-sensitive surface at the back of the eye, you see floating shadows.
As we age, the vitreous shrinks, producing more proteins. This is why, over time, it becomes more and more common to feel like you are seeing floating shadows. Opacities are more common in nearsighted people and diabetics and are more likely to occur after cataract surgery or eye injury.
If you get tired of the effect of floating shadows, try moving your eyes up and down or side to side to gently move them to the periphery of your vision.
Flicker Features
Flickering can appear in various forms. An accurate description of the picture that the patient sees makes it possible to narrow the range of possible diseases, because Many of them are characterized by special forms of flickering. Before visiting a doctor, it is very important to analyze all the features of the phenomenon and remember everything that you can see during the next attack.
The most common forms:
- Zigzag objects. Very often they occur with a sudden change in position, coughing or sneezing. Most often they go away on their own, but if they appear regularly, you need to consult a doctor. May include blurred vision, haze, rainbow spots or glows around light sources, and pain inside various areas of the head. Age-related physiological changes, vascular damage, the presence of a foreign body in the eye, incorrect selection of glasses, migraine, iron deficiency, pregnancy are the main reasons for the appearance of flicker in the form of a snake or zigzag.
- Rainbow circles. A colored halo that appears before the eyes often appears when they are tired or overstrained. Sometimes accompanied by redness of the eyeball, lacrimation or pain. May indicate developing cataracts or glaucoma. Instead of circles, a long arc may sometimes appear.
- Laser glare. Like rainbow circles, glare on the eyes is formed when they are very tired or overexerted. They may also mean that a person has serious problems with the retina. This is possible provided that the phenomenon is periodic and short-term in nature. Corneal edema, cataracts, prolonged exposure to bright light sources, and the use of low-quality eye lenses are the most common causes of glare.
- Bunnies. Bright flashes of light or glowing spots are often accompanied by painful sensations inside the head. They may indicate either simple eye fatigue or problems with the spine, blood pressure, blood vessels or brain.
- Ripple. The appearance of ripples in the eyes is associated with ophthalmological diseases or osteochondrosis. During an attack, it is difficult for a person to see small objects, because... he is hampered by gaps and blurriness of the picture.
Most people can pinpoint exactly what they are seeing. For some it is very difficult to do this, because... the phenomenon can be specific, which makes it difficult to catch those very visual defects and tell the doctor about them.
Flicker in the eyes can appear in the form of various jagged lightning bolts, dots, stripes, zigzags, spots, circles, spirals and other geometric shapes. They come in rainbow, colored, white, black or translucent.
What causes glare?
Glare occurs as a result of movement or tension of the retinal nerve cells. As the vitreous shrinks over time, it can pull on the retina, causing you to “see stars” or flashes of light. The process of separation of the vitreous from the retina is called “posterior vitreous detachment.” This is not a health hazard.
In about 16% of cases, the detachment process creates tiny tears in the retina, which can lead to retinal detachment. This is already a dangerous condition; if it is not treated, blindness is possible.
Other possible reasons why you are seeing strange flashes are an eye injury or a migraine.
Treatment
When the causes of glare in the eyes are accurately determined, the doctor will prescribe the necessary treatment. It may include drugs of a different spectrum, depending on the type of disease. The following types of drugs may be prescribed:
- Eye drops.
- Antibacterial and antiviral tablets.
- Medicines aimed at normalizing blood pressure.
- Means for lowering glucose levels.
- Vitamin complexes.
In most cases, patients are prescribed Emoxipine or Wobenzym. Both drugs are intended for the eyes. The first improves their health and strengthens blood vessels, and the second relieves inflammation and pain. They show high effectiveness in combating most diseases associated with the organs of vision.
If there are no contraindications, you can do a light massage of the eyeballs. This will improve blood flow and relieve tension. With its help, you can remove flickering zigzags that appear before your eyes in just 5 minutes.
Additionally, homeopathic remedies can be prescribed: Teridion, Crocus, Ignacia. The effectiveness of their use has not been proven, but some doctors are inclined to believe that such drugs are quite effective.
When to see a doctor about floaters
If you experience any of the following symptoms, contact your eye doctor immediately for emergency eye care.
Symptoms that should not be ignored:
- The sudden appearance of floaters accompanied by flashes (which can be of any shape or size).
- An increase in floating particles, accompanied by a darkening of one side of the visual field.
- Shadows in peripheral vision
- Do you see glare all the time?
In many cases, the appearance of floaters before the eyes is not a cause for concern; however, the above symptoms may indicate a retinal detachment, and if left untreated, it can cause permanent vision loss or even blindness.
If you experience the above symptoms, you should see a doctor within 24 hours. You will have to endure the discomfort of having your pupils dilated during an eye exam so that the ophthalmologist can get a good look at the peripheral retina and diagnose or rule out a retinal tear or other serious condition. It is worth finding out whether there is a threat to vision. If it's just an uncomplicated posterior vitreous detachment, which is quite common, or an ocular migraine, then you can breathe a sigh of relief.
Diagnostics
If flickering has become regular or is accompanied by serious symptoms, then you cannot do without visiting a doctor. First you need to visit an ophthalmologist. After an examination and a short conversation, the doctor will determine whether there is a need to consult with other specialists, and will also prescribe several important examinations.
You will need:
- Blood and urine tests;
- Ophthalmoscopy;
- Ultrasound;
- CT.
You need to undergo examinations as soon as possible, because... Some diseases require the fastest possible therapeutic intervention. If you delay, there is a risk of encountering complications that will be very difficult to treat.
Traditional methods
You can get rid of flicker at home. Folk remedies that have worked well in the past will help you cope with the problem. The wide variety of methods can be confusing and the effectiveness of such treatment will suffer. Therefore, it is recommended to give preference to the following methods:
- Honey with aloe juice. Mix them in equal quantities to achieve a homogeneous consistency. Place 2 drops into eyes morning, afternoon and evening. The course of treatment is 2 weeks.
- Cucumber juice. Grate the cucumber and squeeze out all its juice through cheesecloth. Mix with water in equal quantities, blot a cloth in the mixture and place on your eyes.
- Chamomile decoction. Pour 250 ml of boiling water over 3 tablespoons of flowers, leave covered until completely cool, strain. Rinse your eyes with the mixture once daily.
After using such products, flickering spots in front of the eyes should stop forming. However, you should consult your doctor in advance, because... in some cases, traditional methods may be contraindicated.
Causes of visual hallucinations
Visual hallucinations are more typical for organic brain lesions, namely the occipital and temporal lobes of the cortex, the rostral parts of the brainstem, and the thalamus. They are also a frequent companion of a darkened, confused consciousness, hypnotic or half-asleep state. The content of the images is varied, but neurological causes more often provoke hallucinations of the true type, and psychotic and hypnotic states provoke pseudohallucinations. Causes include extreme exposure, organic brain damage, mental illness, and acute intoxication.
Intense stress factors
The causes of occasional isolated hallucinatory influxes are states of acute physical or mental stress. Extreme situations that threaten a person’s life lead to changes in brain functioning. Factors affecting the mental state can provoke visions with increased suggestibility and impressionability - psychological readiness to see something related to experiences, but not existing in a real situation. How stress causes are considered:
- Impact of critical temperatures.
A decrease or increase in body temperature is accompanied by a change in blood supply to the brain - the body strives to maintain a constant internal environment, regulates heat transfer, narrowing or dilating blood vessels. Visual hallucinations appear during hypothermia, when the body temperature drops to 35° C, and during hyperthermia, with a body temperature of 39° C and above. The state of hallucination does not last long and is accompanied by disorientation, confusion, and disruption of the functioning of vital organs. - Deprivation of physiological needs.
The causes of hallucinatory visions can be critical conditions in which a person is deprived of the ability to satisfy basic physiological needs - food, water, sleep, rest. Blurred images begin to appear on days 8-9 of fasting, on days 2-3 without water (up to about 10% of body fluid is lost). The critical phase of sleep deprivation is 4 days, when irreversible life-threatening processes occur, apathy increases, abulia occurs, and hallucinatory symptoms develop. - Lack of sensory stimulation.
The human nervous system is able to function normally when receiving various information from the outside - when the senses are stimulated. Sensory deprivation is partial or complete isolation from external influences. Its causes are the loss of the analyzer, staying in a closed room without light, sounds, or vibrations. Sometimes this state is created artificially using derivation chambers and baths. In the absence of external visual stimuli, the brain begins to compensate for the lack of information by creating visual hallucinations. - Social isolation.
Visual hallucinatory images are formed as a result of long-term forced or specially organized loneliness (hermitage). This phenomenon has been studied in most detail using examples of prisoners in solitary confinement. They experience elementary auditory and visual hallucinations (flashes of light, screams, noises) provoked by sensory deprivation, as well as complex dynamic images - “friends”, “mentors”, “saviors”. They contact the prisoner with glances, silent orders, and words. - Psychological trauma.
Possible causes of visual hallucinatory symptoms are traumatic situations. The first pathogenetic mechanism is associated with situations of loss of loved ones, places or events to which a person was attached. Hallucinatory images “return” what was lost. Another mechanism is based on post-traumatic experience: the emotions of fear, anger, horror were not experienced in a critical situation, so a person involuntarily returns to it through thoughts, dreams, visual hallucinations. Example: a former military man suffering from PTSD “sees” explosions and shooting enemies.
Neurological diseases
Visions in neurological patients occur with local and diffuse brain damage. Visual images can be provoked by pathological irritation of the areas responsible for receiving and processing visual information. This type of disorder is characterized by elementary images – photopsia. In addition, visual hallucinations are sometimes included in the structure of the hallucinatory-delusional symptom complex, the clouded consciousness syndrome. The most common causes of visions:
- Dementia with Lewy bodies.
The disease is diagnosed in patients 65-70 years old and is characterized by changes in the structure of neurons in the cerebral cortex. Typically, it begins with a triad of symptoms, including extrapyramidal disorders, dementia, and visual hallucinations. Most often, hallucinatory images develop that have a clear color, shape, size, and volume. A typical sign of this type of dementia is the rapid disappearance of visions when the patient tries to interact with them. - Alzheimer's disease.
The basis of the pathology is the process of neuron death, loss of synaptic connections in the cortical zones and subcortical areas of the brain. Visual hallucinations are possible in the second stage of the disease, when there is a noticeable deterioration in everyday and professional activities, the process of constructing a speech utterance is disrupted, and it becomes impossible to perform voluntary actions. Hallucinatory symptoms manifest themselves in the context of delusional syndrome and are often accompanied by anxiety, fear, and panic. - Parkinson's disease.
The disease occurs with the progressive death of neurons that produce the neurotransmitter dopamine. In a mild (outpatient) form of the disease, psychosis develops in approximately 20% of patients, in a severe form - in 65%. The psychotic state is manifested by unmotivated fear, absent-mindedness, insomnia, hallucinatory-paranoid symptoms, and disorientation. The causes of psychosis in Parkinson's disease are considered to be the rapid progress of pathology and the use of medications aimed at alleviating motor dysfunction. - Traumatic brain injuries.
TBI includes bruises and concussions, barotrauma, and skull injuries. With focal damage to the occipital areas, visual hallucinations are represented by elementary forms: zigzags, flashes in one half of the visual field. Hallucinatory-delusional psychoses more often develop in men after moderate and severe injuries. They appear many years later, in the long term. Visual hallucinations form before psychosis against the background of twilight, delirious or oneiric changes in consciousness. In a psychotic state, auditory pseudohallucinations occur more often. - Cerebral vascular pathologies.
Diseases of the cerebral vessels (atherosclerosis, arteritis, hypertension) lead to a deterioration in the blood supply to its individual areas and diffuse organic lesions. Neurological symptoms include headaches, dizziness, vomiting, perception disorders, and speech disorders. Patients see flashes, sparks, flickering. Visual phenomena develop during exacerbation of the disease and are accompanied by disorientation in space and general weakness. - Brain tumors
. Clinically, brain tumors are manifested by focal and general cerebral symptoms. The causes of visions are neoplasias localized at the junction of the frontal and temporal lobes. Visions arise within the framework of paroxysmal disorders - short-term hallucinatory influxes without delirium. The patient's critical abilities remain relatively intact; after a certain duration of illness, he begins to understand that visible images are a symptom of the spread of the tumor.
Mental disorders
Visual hallucinations develop in psychotic states of various origins. Exogenous psychoses are characterized by true hallucinatory images, while endogenous psychoses are characterized by pseudohallucinations. In both cases, there is emotional and behavioral inadequacy of the patient, a decrease or complete absence of a critical attitude towards his condition. Common psychotic causes of hallucinations:
- Symptomatic psychoses.
This group includes infectious psychoses, psychotic states provoked by endocrinopathies, vascular pathologies, acute intoxication with surfactants, and alcohol. Stupefaction occurs in the form of oneiroid - a dream-like disorientation with detailed pictures of fantastic pseudo-hallucinatory experiences intertwined with reality. The content is usually adventurous, fabulous, less often - ordinary. Visual hallucinations are colorful, moving, massive. Patients either actively participate in the visions or remain observers. - Schizophrenia-like disorder.
Common causes of the disease are head injuries, neuroinfections, and epilepsy. In organic delusional disorder, visual hallucinations predominate, rather than auditory hallucinations as in schizophrenia. Their content is often related to the theme of delirium and reflects scenes of a mystical or religious nature. Hallucinatory-delusional syndrome is manifested by inappropriate behavior, impulsiveness, and emotional excitability. - Schizophrenia.
This disease is characterized by auditory hallucinatory phenomena. Visual hallucinatory disorders occur less frequently, they are not clearly expressed, inconsistent, flash in fragments, and resemble visions. Often their purpose, content, and reasons are completed by the patient on the basis of delusional ideas and information from hallucinatory voices. If schizophrenia has developed as a result of taking psychoactive substances, “flashbacks” appear - pictures from the past.
Acute period of intoxication
A state of acute intoxication develops after the administration of a large dose of a psychoactive substance. It leads to impaired consciousness, deterioration of cognitive activity, and distortion of perception. People's behavior and emotions become inadequate and uncontrollable. There is no critical attitude towards one's own condition. Visual hallucinations are most likely due to poisoning with the following substances:
- Drugs.
Common causes of visions are the use of hallucinogens, volatile solvents, and cannabis preparations. When intoxicated with hallucinogens, the world begins to seem brighter, objects begin to appear in unusual colors. Visual hallucinations are elementary and scene-like, often true. Substance abuse using volatile solvents is manifested by impaired consciousness with acute hallucinosis, delirium or oneiroid. Hallucinatory pictures are bright, plot-driven. Taking cannabinoids provokes visions that are brighter than the real world, present with open and closed eyes. - Medicines
. Visual hallucinations as part of delirious stupefaction occur in case of poisoning with diphenhydramine, atropine, and antidepressants. When taking large doses of psychostimulants, intoxication paranoid develops, which includes delusional ideas, visual and other types of hallucinations. There is a risk of developing manic-like states with euphoria, motor disinhibition, and accelerated thinking. - Alcohol.
Delirium tremens occurs when drinking stops in patients with stages II-III of alcoholism. Alcoholic delirium is manifested by delirium associated with hallucinatory images of various modalities. Visions are usually threatening, appearing in the images of unpleasant and dangerous creatures - demons, devils, creeping reptiles. A state of psychosis, psychomotor agitation during intoxication, is a common cause of self-harm.