Home > Cancer treatment in Israel > Treatment of meningioma in Israel
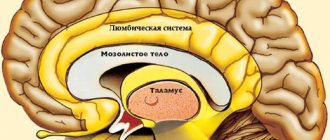
Meningioma is a tumor that develops from the membranes covering both the brain and spinal cord. In terms of frequency, it ranks first among benign intracranial neoplasms – it accounts for 25% of all diagnosed cases. As a rule, the tumor is characterized by a slow growth rate, and it can be localized in different parts of the nervous system due to the fact that the meninges cover both the brain and the spinal cord.
Typically,
patients have one primary focus of meningioma , but in rare cases, tumors form in several parts of the central nervous system
.
Most often, meningiomas occur in women aged 40 to 70 years, but men over 35 years of age also suffer from the pathology. As a rule, the disease is diagnosed accidentally, during a test for another reason, or when the formation significantly increases in size and the symptoms become severe. There are 3 types of meningiomas: benign, atypical and malignant. Benign meningiomas do not invade surrounding tissue, grow slowly and in many cases do not require treatment, but only regular monitoring. Atypical and malignant meningiomas - they account for about 5-10% of the total - are characterized by rapid infiltrative growth. It is malignant types of meningioma that are more common in men.
Malignant tumors are mainly localized in:
- cavernous and parasagittal sinuses;
- pyramid of the temporal bone;
- wings of the sphenoid bone;
- foramen magnum;
- cerebral hemisphere zone;
- tentorial notch;
- cerebellopontine angle.
Malignant meningiomas require immediate medical attention at the first signs of the disease.
To ensure an accurate diagnosis and receive the most effective medical care, you need to choose the right clinic. Israeli clinics are among the leading cancer centers in Europe: the best oncologists and neurosurgeons are gathered here, and all conditions for a comfortable stay are created for patients. Israel also attracts medical tourists due to the affordable cost of medical care combined with the opportunity to undergo a full examination, therapy and rehabilitation in one medical facility. You can evaluate the benefits of our clinic’s offers by sending an online request or contacting us at the phone number indicated on the website.
Consult an Israeli specialist
Causes of the disease
The reasons for the formation of tumors and their transformation into malignant lesions have not been clearly established. However, doctors are aware of the negative impact of certain factors that increase the risk of meningioma. Among them:
- unfavorable family history, in particular, the presence of multiple hemangiomatosis or neurofibromatosis in close relatives;
- being female - the female body produces hormones that contribute to the development of tumors;
- age over forty years;
- exposure to radiation, both in high and low doses. The risk of meningiomas is increased in patients who have previously received radiotherapy for brain tumors.
In the majority of patients, with timely and adequate treatment, which consists of radical removal of the meningioma, their health is completely restored, and relapses are extremely rare. The likelihood of relapse is high in patients with malignant meningiomas and tumors growing in the area of the venous sinuses, which makes their removal difficult.
Meningioma is not a brain tumor because it is formed from its membrane. At the same time, by squeezing brain tissue as it grows, it can cause symptoms characteristic of brain tumors
.
Meningiomas account for about 22% of the total number of brain tumors.
The incidence of intracranial meningiomas averages 3 cases per 100,000 population per year. Meningiomas are sporadic, i.e. non-inherited tumors.
Meningiomas are a group of tumors that arise from the meninges and are not found in other tissues of the body.
The place of initial growth is the pachyonic granulation cells. X-ray and radioactive irradiation, head trauma and dietary nitrates increase the likelihood of meningiomas
There are 11 types of benign meningiomas. About 60% of intracranial meningiomas are meningothelial, 25% are transitional and 12% are fibrous; the remaining histological variants are rare. Papillary meningiomas are classified as a separate group (these very rare malignant tumors occur at a young age and are characterized by a high frequency of relapses and brain invasion).
Location of meningiomas: • Convexital - 40-50%. • Parasagittal (falx, walls of the superior sagittal sinus) - 20 - 30%. • Basal (growing at the base of the skull) - 20-30%.
| MRI, T2-weighted image. Convexital meningioma of the right frontoparietal region. | MRI, T1-weighted image with contrast enhancement. Parasagittal meningima with large hyperostosis and intracranial node, the sinus is completely invaded by the tumor. | MRI, T1-weighted image with contrast enhancement. Basal meningioma (wing of the main bone). |
The degree of malignancy of meningiomas. 1. I degree of malignancy “Typical” (85% of all meningiomas) - the number of relapses up to 10 years after surgery is about 15%. 2. II degree of malignancy “Atypical” (10 – 15%) – relapse of meningioma within up to 10 years occurs in 30% of patients. 3. III degree of malignancy “Anaplastic” (1 – 2%) – relapse after surgery within 3 years occurs in 100% of patients.
Meningioma, like all other tumors, does not have its own capsule. The capsule can be formed only from normal tissues surrounding the tumor, which undergo changes (from lysis to fibrosis) depending on the biochemical characteristics of the tumor and the reactivity of the body. Treatment.
The main treatment for clinically significant meningiomas is surgical removal of the tumor.
| MRI of a patient with a giant meningioma of the olfactory fossa | ||
| MRI of the same patient 1 year after surgery |
The operation should be aimed at ensuring its maximum radicality within the limits of “physiological permissibility” (N.N. Burdenko).
To formalize the degree of radicality of operations for meningiomas, the Simpson scale is used: Type 1 – macroscopically complete removal of the tumor with excision of the dura mater at the site of initial growth and resection of all affected bone; Type 2 - macroscopically complete removal with coagulation of the dura mater at the site of initial growth; Type 3 - macroscopically complete removal without excision or coagulation of the dura mater at the site of original growth and (or) without resection of the entire affected bone; Type 4 – partial removal of the tumor Type 5 – biopsy or decompression.
| CT scan of the brain. Menigioma of the pyramid of the temporal bone before surgery. | CT scan of the brain of the same patient 9 months after surgery. |
Currently, the department has introduced the latest minimally invasive method of destroying hard-to-reach tumors using cryodestruction. The operation is performed through a small incision using modern neuronavigation systems. This technique makes it possible to effectively treat brain tumors that were previously considered inoperable.
The five-year survival rate of currently operated patients is about 92%. Postoperative mortality ranges from 0 to 5% depending on the location of the meningioma.
Symptoms and treatment of brain meningioma
In the initial stages, most meningiomas are completely asymptomatic. Signs of the disease appear when the tumor grows, compresses the brain or spinal cord and interferes with normal blood circulation. In such situations, the following may occur:
- pressing headache that worsens at night or in the morning;
- visual disturbances (double or blurry vision);
- memory impairment;
- hearing loss, ringing in the ears;
- loss of smell;
- convulsions;
- weakness or partial paralysis of the limbs;
- change in emotional state (depression, euphoria).
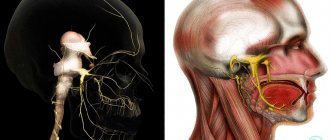
With a certain localization of meningiomas, more specific symptoms are noted:
- in the area of the tubercle of the sella turcica – a sharp deterioration in vision;
- in the temporal lobe – visual and hearing impairment;
- in the area of the tentorium cerebellum – coordination and movement disorders;
- in the convexital area – epileptic seizures.
If you notice one or more neurological symptoms in yourself, your spouse or a relative, do not delay getting tested. Moreover, in our clinic it will take only a few days for a doctor’s consultation, diagnostic measures and preparation of an individual treatment program.
Help is needed? Doctor online. Consultation is free+972-52-651-26-54
Help is needed? Doctor online. Consultation is free+972-52-651-26-54
Symptoms of meningioma
Symptoms depend on where in the brain the tumor is located. In each case, the set of symptoms will be slightly different, since each part of the brain is responsible for performing a specific function. For example, if the tumor is located closer to the frontal lobe, the patient may experience impaired movement in the limbs. If the tumor is located closer to the parietal lobe, the person may have difficulty writing or recognizing written text. Convulsions or paresis on one side of the body may also occur.
A tumor located in the temporal lobe is characterized by symptoms such as memory loss and impaired speech understanding.
As the tumor grows, the patient develops new symptoms: headache that does not go away even with painkillers, drowsiness, nausea and vomiting.
If we summarize all the possible symptoms that appear with brain miningioma, we get the following list:
- Impaired understanding of written text;
- Staggering when walking;
- Visual impairment;
- Hearing impairment;
- Dizziness;
- Inability to say something;
- Convulsions;
- Impaired speech understanding;
- Behavior change;
- Epilepsy;
- Symptoms of increased pressure inside the skull.
- Memory loss;
- Paralysis or paresis, usually starting with weakness in the limbs;
It is important to remember that these symptoms do not appear all at once and do not occur suddenly. They grow gradually, their number increases with the size of the tumor.
Disease detection
To choose the optimal treatment strategy and assess the prognosis, the doctor needs to get the most complete picture of the disease. For this purpose, all patients with suspected meningioma undergo a thorough diagnosis using the most modern equipment.
Before instrumental tests are started, the patient is examined by a neurologist. During the examination, the doctor assesses:
- state of the vestibular apparatus;
- reflexes;
- vision and hearing;
- coordination of movements and other cerebellar functions.
In addition, the doctor will carefully study the medical history and medical documentation provided by the patient, familiarize himself with the data of previously performed medical examinations and test results.
As part of the diagnosis, blood tests are required - general clinical, as well as a special analysis for tumor markers. Most patients are prescribed electroencephalography, a study of the electrical activity of the brain. This is an absolutely safe and painless procedure lasting about half an hour.
Medical imaging techniques are recognized as the “gold standard” in the diagnosis of meningiomas: computed tomography and magnetic resonance imaging. Both diagnostic procedures are usually performed with contrast enhancement to assess the size and location of the tumor, its location in relation to critical brain structures, and resectability (the possibility of removal during surgery).
| CT scan | creates a layer-by-layer image of brain structures, allowing you to identify deviations from the norm; |
| magnetic resonance imaging | a modern technique used as an alternative to CT to obtain a detailed picture of the affected organ; |
| angiography | The procedure involves the introduction of a special contrast agent into the blood to monitor the blood supply system of the tumor. This method is mainly used before surgery for the most accurate planning of surgeons’ actions; |
| biopsy | study of the morphological characteristics of a tumor based on a sample of tumor tissue. Biopsy and histological analysis help differentiate benign from malignant meningiomas. At the Assuta clinic, when performing a biopsy, the most modern equipment is used, which allows it to avoid affecting vital areas of the brain. |
Diagnosis of the disease
Brain meningioma grows slowly, and sometimes stops its growth for a while. Therefore, diagnosing a tumor is not easy. Before prescribing treatment, the patient must undergo an examination, including a neurological one.
Diagnosis of the disease is possible only using special methods for detecting the disease.
Clinics in Germany conduct the following types of studies:
- Primary medical examination. The patient is examined by a doctor for the presence of reflexes, skin sensitivity, and the functions of the hearing and vision organs are assessed.
- Three-dimensional computed tomography. Allows you to visualize the structure of the brain and see the connection of the tumor with other structures.
- X-ray diagnostics. Using X-rays, the internal structure of the brain is examined, and it is possible to see changes in bones and the presence of calcifications in the tumor.
- Digital subtraction angiography. Allows you to identify meningioma in more than 80% of patients and examine the cerebral vessels in detail.
- Magnetic resonance imaging. The technique allows you to detect a tumor of any location.
- Electroencephalogram.
- Biopsy of a tumor-like neoplasm to determine the cell type.
Effective assistance from Israeli doctors
The effectiveness of treatment of meningioma in the best medical facilities reaches almost 100% due to the work of first-class world-famous neurosurgeons. Thanks to their skill, as well as the most modern and effective treatment methods, Assuta patients quickly return to everyday life, forever forgetting about their terrible diagnosis - meningioma.
The therapeutic course includes several stages:
- consultation with a specialist, examination, medical history;
- detailed diagnostics (laboratory tests, computer and magnetic resonance imaging, electroencephalography);
- drawing up an individual treatment plan.
When planning treatment, the doctor takes into account the characteristics of the tumor (size, location, histological type, proximity to large vessels or vital centers), as well as the general condition of the patient (age, presence of concomitant diseases, severity of symptoms).
Treatment of meningioma
Treatment for meningioma depends on the size of the tumor and its location.
If the meningioma develops slowly and does not cause any symptoms, you may not need treatment. You may need to have an MRI every year to monitor the tumor's progress. You should also tell your doctor if you develop any symptoms. If the meningioma is cancerous, causes symptoms, or grows quickly, you may need surgery to remove it.
Some meningiomas cannot be removed because they are located near areas of the brain that perform important functions. In this case, you may be prescribed a course of radiotherapy to stop their development. If you have had surgery to remove a meningioma but it is not completely removed, you may also need radiation therapy to stop the tumor from growing. In rare cases, you may need chemotherapy or other treatment.
There are clinical studies that are looking at different treatments for meningiomas.
For more information about clinical trials at Memorial Sloan Kettering (MSK), contact your doctor or visit . to come back to the beginning
Treatment of meningioma without surgery - Cyber and Gamma knife at the Assuta clinic
Surgery is the highest priority method of combating the tumor, since this is the only way to remove it entirely, preventing the development of relapse.
The operation is indicated if the meningioma has already reached an impressive size, but its removal does not pose a danger to the life and health of the patient. For example, it is not always possible to perform resection of meningiomas adjacent to large blood vessels, venous sinuses, brain stem, etc. Assuta specialists recommend treating meningiomas that are difficult to reach or adjacent to critical structures using conservative methods that reduce the risk of complications to almost zero and do not injure healthy tissue.
Using a radio wave cyber knife instead of a traditional scalpel makes the procedure for destroying a tumor absolutely painless. In addition, there is no need for general anesthesia. The proven effectiveness of the cyber knife is 95%, and the course of treatment takes from one day to several months, depending on the size of the tumor and the individual characteristics of the body.
A gamma knife can be used to remove very small tumors. Gamma therapy is a modern non-invasive, gentle method of meningioma removal, practiced in medicine in Israel. It involves targeted irradiation of the lesion from different sides with small doses of radiation, which are focused directly in the area of tumor growth. The accuracy of the gamma knife is amazing - 0.3mm (for the cyber knife - 1.0mm).
After removing the meningioma using any of the above methods, the patient is observed for some time at the Assuta clinic and undergoes repeated checks. If there are residual tumor cells, a stereotactic course of radiation is prescribed, during which they are completely destroyed.
Israeli doctors do not recommend using chemotherapy and external beam radiation therapy to treat meningiomas due to the low effectiveness of these techniques. Chemotherapy is rarely used for inoperable meningiomas that are resistant to radiotherapy.
Treatment of meningioma in the most popular Assuta clinic in Israel is carried out under the close supervision of experienced neurosurgeons - Zvi Ram, Zvi Cohen, Moshe Adani, Dvora Blumenthal.
Material and methods
From 2013 to 2021 in the 7th neuro-oncology department of the National Scientific Research Center for Neurology named after. acad. N.N. Burdenko, 7 patients (5 women, 2 men) were operated on from the supraorbital transbrow approach: with meningioma of the anterior cranial fossa area - 3 patients and tubercle of the sella - 4. The age of the patients ranged from 51 years to 75 years (median 60 years). Clinical symptoms before surgery were represented by cephalgic syndrome in 4 cases and decreased visual acuity in 3 cases. The choice of surgical approach was determined by the severity of hair in the eyebrow area, the size of the frontal sinus, the anatomical and topographical features of the tumor, and the patient’s consent. The size of the removed tumors in maximum dimension ranged from 20 to 60 mm (median 40 mm). All operations were performed using the Mari microscope control device, without using retractors.
Patient position on the operating table
The patient is placed in a supinated position with the head fixed in a Mayfield brace (Fig. 1).
Rice. 1. The patient’s head is tilted to the right side by 20°. The zygomatic tuberosity is the most elevated area.
For suprasellar meningiomas, the head is rotated 30°. For meningiomas of the olfactory fossa, the head is rotated 45-60° to the side contralateral to the access. The degree of head rotation depends on the location and projection of the tumor: large tumors located in the anterior parts of the anterior cranial fossa require the greatest rotation of the head in order to reach the edge of the tumor opposite from the trepanation. The head should be slightly extended so that the zygomatic tuberosity is the highest point. If it is necessary to close the frontal sinus, a small section of the anterior abdominal wall is prepared to take subcutaneous fat.
Surgical approach
For a skin incision, the eyebrow is shaved, after which the boundaries of the incision are marked. The landmark for the medial border of the incision is the supraorbital notch. The incision in this area should be made superficially to avoid damage to the supraorbital nerve. Next, the incision extends laterally along the eyebrow, and then slightly down along the frontozygomatic process of the zygomatic bone (Fig. 2).
Rice. 2. A skin incision was made along the left eyebrow. The supraorbital nerve (S) passes near the medial border of the incision. Laterally, the incision extends to the temporalis muscle (T).
To expose the supraorbital area, the skin flap is pulled up and secured with several hooks. After exposing the periosteum, a semicircular incision is made, and then it is also tilted upward. In the area of transition of the periosteum into the fascia of the temporalis muscle, a small incision is made in the temporalis muscle, which is also retracted using hooks to expose the “key point” posterior to the frontozygomatic process of the zygomatic bone (Fig. 3, a).
Rice. 3. A skin incision was made along the left eyebrow. After preparation, soft tissues are pulled back with hooks on springs. a — a milling hole is placed in the area of the key point; b — osteoplastic trephination of about 15×25 mm was performed in the left supraorbital region. A single burr hole is placed posterior to the key point and inferior to the superior temporal line using a high-speed bur. After this, an osteoplastic craniotomy of approximately 15-20 by 20-25 mm is performed, not including the orbital roof (see Fig. 3, b).
After performing a craniotomy, to improve visibility and reduce traction on the brain, it is very important to grind down the inner bone plate along the edges of the craniotomy with a bur, while the outer bone plate should remain intact (Fig. 4).
Rice. 4. The dura mater is retracted downward with a vacuum aspirator (1), and in parallel, the internal bone plate is ground down at the edges of the trepanation with a pneumatic bur (3). The outer bone plate remains intact (2). Large bony protrusions at the base of the anterior cranial fossa should also be ground down with a bur if they interfere with adequate visibility and access to the tumor. If the frontal sinus is opened, it must be closed with an autograft.
Stitching
After tumor removal, the dura mater is sutured with a continuous suture. To seal the seam, Tachocomb is laid on top of it. It is necessary to check the anteromedial wall of the trepanation for the presence of a defect in the frontal sinus. If there are no defects, the bone flap is placed in place and fixed with 3-4 titanium plates. The site of the burr hole is covered by the superior temporal muscle and fascia. To achieve a good cosmetic result, the bone flap is placed at an equidistant distance from the edges of the trepanation. Next, sutures are placed on the subcutaneous fatty tissue and skin, the latter is sutured with an intradermal absorbable suture. If a defect is detected in the frontal sinus, fatty tissue, previously taken from the paraumbilical area, is placed into it. The fatty tissue is additionally fixed with fibrinthrombin glue.
Prices for treatment of brain meningioma at the Assuta clinic
Basic screening program for brain tumors in Israel:
| Description of the procedure | Cost ($) |
| advanced blood tests | 440 |
| field of view | 350 |
| consultation with a neurosurgeon | 550 |
| preoperative preparation (ECG + x-ray of the lungs + consultation with an anesthesiologist) | – |
| navigation MRI | 1350 |
Therapy includes:
| Description of the procedure | Cost ($) |
| surgery and 4 days of hospitalization in the neurosurgery department (1 day in intensive care) | 23900 |
| use of neuro-physiological monitoring | 1450 |
| surgical materials and equipment | 2250 |
| rapid biopsy during surgery and final histopathology of the tumor | 1250 |
After completion of the operation and during the further rehabilitation period, the patient is advised not to leave Israel for fourteen days. During this period, Israeli doctors will develop an individual program of further medical observation and treatment for you.
About meningioma
Meningioma is a type of brain tumor that develops in the meninges.
The meninges are the tissues that surround your brain and spinal cord. Meningiomas usually appear in the skull, but can also appear in the spine. In most cases, people with meningioma develop only 1 tumor in 1 place, but it is possible for several tumors to appear simultaneously in different parts of the brain and spinal cord.
Most meningiomas are benign (not cancerous). Some meningiomas can be malignant (cancerous), but this is rare. Even if the tumors are not cancerous, due to their location they can cause serious problems. If they grow too large, they can affect the functioning of the brain, and they can also cause problems if they are located too close to important nerves or blood vessels.
After undergoing radiation therapy to the brain or spinal cord, a person's risk of developing meningioma increases. Hormonal changes or your genes (DNA) can also increase your risk of developing meningioma.
to come back to the beginning
Methods of radiation and combined treatment
Medical specialists abroad often use combination treatment methods to get rid of the disease:
- Radiation therapy. The traditional method for treating this disease may be the only method of treatment for large tumors and in cases where there are contraindications to surgery. Treatment is carried out in several sessions by exposing the tumor to radiation. Radiation therapy is considered less effective than the “cyber knife” because it acts with less precision.
- Method of combined treatment. In Germany there are a number of clinics that practice combination treatment. The technique involves the use of traditional beam therapy and “cyber knife” sessions. This treatment allows you to significantly increase the effectiveness of the permissible dose of radiation and provides comfort to the patient within one medical institution.
Diagnosis and treatment of meningioma in German clinics allows experienced specialists to completely remove tumors even in hard-to-reach areas of the brain. The availability of all necessary technical means abroad guarantees successful and painless treatment without consequences. Upon completion of rehabilitation treatment, specialists continue to provide consultations and monitor the condition of patients after their return to their homeland.