We usually don’t hear about epilepsy as often as, say, heart attacks and strokes. However, almost each of us, one way or another, is familiar with this disease, if not personally, then from the stories of others whose relatives or friends suffer from this disease. And this is no coincidence, because epilepsy is observed in almost 5% of the population of our planet, and in children this disease is registered three times more often than in adults. And the general term “epilepsy,” according to the conclusion of modern practicing neurologists, combines more than fifty diseases that differ in clinical manifestations and treatment, including the most common generalized epilepsy.
What is generalized epilepsy
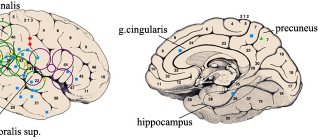
Generalized epilepsy is a chronic pathology of the brain, which is characterized by the formation (in both hemispheres) of neural impulses of excessive intensity. During the resulting attacks (which become repeated), many of the patient’s organic functions are temporarily disrupted:
- motor
- vegetative
- sensitive
- mental
Generalized epilepsy today means all epileptic forms based on the stereotypical occurrence of epileptic seizures. The latter consist of absence seizures (short-term, literally for a few seconds, switching off consciousness), generalized myoclonic (associated with involuntary muscle tension) and tonic-clonic (associated with changes in muscle tension and intermittent muscle contractions) paroxysms.
Juvenile myoclonic epilepsy.
Juvenile myoclonic epilepsy (JME) is one of the forms of idiopathic generalized epilepsy, characterized by onset in adolescence with the occurrence of massive bilateral myoclonic seizures, mainly in the arms, during the period after patients awaken. JME is one of the first forms of epilepsy with a known genetic defect. A two-locus model of inheritance (dominant-recessive) is assumed, with the dominant gene localized on the short arm of chromosome 6. The onset of JME varies from 7 to 21 years with a maximum in the age range of 11-15 years. The disease can begin at an earlier age with absence seizures or DBS, followed by the addition of myoclonic seizures during puberty. Myoclonic seizures are characterized by lightning-fast twitching of various muscle groups; they are often bilateral, symmetrical, single or multiple, varying in amplitude. They are localized mainly in the shoulder girdle and arms, mainly in the extensor muscle groups. During attacks, patients drop objects from their hands or throw them far to the side. In 40% of patients, myoclonic attacks also involve the leg muscles, while the patient feels a sudden blow to the knees and slightly squats or falls (myoclonic-astatic attacks); then immediately gets up. Consciousness is usually preserved during attacks. Myoclonic seizures occur or become more frequent in the morning, after the patient awakens. In 90% of cases they are combined with GSP awakenings and in 40% with absence seizures. The main triggers for attacks are sleep deprivation and sudden violent awakening. Approximately 1/3 of JME patients (usually females) exhibit photosensitivity. Epileptic activity on EEG is detected in 85% of patients in the interictal period. The most typical is generalized fast (from 4 Hz and above) polypeak-wave activity in the form of short bursts. Peak-wave activity of 3 Hz may also occur. Treatment. Along with drug therapy, it is necessary to strictly adhere to sleep and wakefulness; Avoid lack of sleep and photostimulation factors in everyday life. Basic drugs are exclusively derivatives of valproic acid. The average daily dosage is 40-60 mg/kg. If the effectiveness is insufficient, polytherapy is prescribed: depakine + suxilep (for resistant absence seizures); depakine + phenobarbital or hexamidine (for resistant GSP); depakine + lamictal or clonazepam (for resistant myoclonic attacks and severe photosensitivity). Complete drug remission is achieved in 75% of patients, in most cases with valproate monotherapy. However, subsequently, when AEDs are discontinued, relapses are observed in half of the patients. For this form of epilepsy, it is recommended to discontinue AEDs after at least 4 years from the onset of remission.
What types of generalized epilepsy are known?
Depending on the nature of the origin, generalized epilepsy is usually divided into:
- idiopathic - genetically transmitted and, mainly, occurring in childhood or adolescence (or with possible manifestation in adulthood), characterized by the absence of pathologies of the nervous system and, in particular, structural changes in the brain (except for changes recorded using EEG and MRI);
- symptomatic – arising as a result of traumatic brain injuries (in most cases during childbirth), or as a result of extensive organic brain damage after neurointoxication, infectious diseases, as well as against the background of hereditary pathologies, neoplasms, and some dysmetabolic conditions (including intrauterine fetal hypoxia);
- cryptogenic – with unknown etiology.
Depending on the presence of seizures in attacks, generalized epilepsy is divided into:
- non-convulsive (characterized by the presence of absence seizures in attacks);
- convulsive (characterized by tonic-clonic phases of the attack).
Idiopathic generalized epilepsy
All forms of idiopathic epilepsy are characterized by:
- Genetic predisposition (often a family history of epilepsy).
- Limited age of disease onset.
- No changes in neurological status.
- Normal intelligence of patients.
- Preservation of the basic rhythm on the EEG.
- Absence of structural changes in the brain during neuroimaging.
- The drugs of choice for treatment are valproic acid derivatives.
- Relatively favorable prognosis with therapeutic remission achieved in the vast majority of cases.
What are the symptoms of generalized epilepsy
The symptoms of generalized epilepsy usually depend on its form.
IdiopathicSymptomatic
Age of first manifestation Childhood and adolescence (mainly up to 21 years). Any age period, but for congenital and hereditary pathologies manifestations in early childhood are typical.
Neurological status Symptoms are scattered, occasionally focal. Depends on the underlying disease, which determines general cerebral and focal symptoms.
Nature of attacks Epileptic paroxysms of a primary generalized nature: with myoclonic convulsions (short-term twitching of the limbs), absence seizures (with lack of attention), generalized tonic-clonic convulsions (muscle tension, followed by intermittent muscle contractions against the background of a lack of consciousness, which often ends in involuntary urination and muscle pain). relaxation).Generalized epileptic seizures (against the background of clinical manifestations of the underlying disease). They are characterized by general muscle tension with a short-term cessation of breathing, followed by convulsions that can last from 10 seconds to 20 minutes.
Cognitive manifestations Mental abilities are normal, although sometimes they may temporarily decrease slightly (in approximately 5-8% of patients). There is a decrease in intellectual abilities; mental retardation and cerebral palsy may develop in children.
Juvenile absence epilepsy.
Juvenile absence epilepsy (JAE) is a type of idiopathic generalized epilepsy, which is characterized by the main type of seizures - absence seizures, debuting in the pubertal period with a high probability of the addition of DBS and characteristic EEG changes in the form of generalized peak-wave activity with a frequency of 3 Hz or more. The onset of absence seizures in JAE varies from 9 to 21 years, with an average of 12.5 years. In the vast majority of patients (75%), absence seizures begin in a relatively short time period - 9-13 years. An important feature of JAE is the frequent onset of the disease with GSP - 40% of cases. Absence seizures in patients suffering from JAE are manifested by a short loss of consciousness with freezing and hypomimia. Characterized by a significant predominance of simple absences, that is, attacks without any motor component. The duration of attacks ranges from 2 to 30 seconds, on average 5-7 seconds. At the same time, half of the patients experience very short absence seizures, not exceeding 3 seconds. A characteristic feature of JAE is the relatively low frequency of attacks compared to DAE. In most patients, single absence seizures predominate during the day or 1 attack every 2-3 days. Generalized convulsive seizures are observed in the majority of patients – 75%. In the group of patients with GSP, the disease most often debuts not with absence seizures, but with tonic-clonic convulsive paroxysms. GSPs are characterized by short, infrequent tonic-clonic seizures, usually occurring upon awakening or falling asleep. Unlike DAE, hyperventilation provokes absence seizures in no more than 10% of patients with JAE. HSP in 20% of patients is provoked by sleep deprivation. During an EEG study in the interictal period, results close to normal are found in 25% of patients. The main EEG pattern is generalized peak-wave activity with a frequency of 3 Hz or more (4-5 per second), which is predominantly symmetrical and bilaterally synchronous. Treatment. The effectiveness of treatment for JAE is significantly lower than for DAE. Therapeutic remission is achieved, on average, in 60% of patients, a significant reduction in attacks - 35%, no effect - 5%. Treatment begins with monotherapy with valproic acid. The average dosage is 30-50 mg/kg/day. Due to the extremely high probability of the addition of GSP in JAE, starting treatment with succinimides, as well as using them as monotherapy, is strictly contraindicated. If there is no significant effect from monotherapy with valproate in sufficiently high doses, a combination of valproate with succinimides or lamictal is used. Average doses of suxilep are 20 mg/kg/day; Lamictal – 1-5 mg/kg/day.
What is the diagnosis of generalized epilepsy?
Generalized epilepsy is diagnosed by a doctor based on:
- careful collection of anamnesis (including information about the presence of the disease in the family, the age of the patient at which the first attack was observed, the duration and nature of the attack, the presence of seizures)
- laboratory testing of blood and urine
- echoencephalography (including EEG monitoring)
Additionally, to clarify the diagnosis, you may need:
- CT
- NMRI
- biochemical examination of blood and cerebrospinal fluid
- consultations with other specialists (neurosurgeon, infectious disease specialist, pediatric ophthalmologist)
What is the treatment for generalized epilepsy
Effective treatment of this type of epilepsy directly depends on the form of the disease, as well as the nature of the attacks. And if it does not always allow the patient to forget about his illness, ideally it should be aimed at maximizing the reduction in the frequency and severity of attacks.
Anticonvulsant therapy for generalized epilepsy is usually recommended to begin no earlier than the second attack and only if an accurate diagnosis has been established. It is usually started by prescribing a base drug specifically for this epiform (for example, valproate, etc.), starting with a dose that is approximately a quarter of the standard therapeutic dose. Over the next two to three weeks (with the indispensable condition of good tolerability and the absence of a therapeutic effect), the starting dose is increased by another half, further bringing it to the average therapeutic dose. Such monotherapy is usually quite effective in the case of idiopathic generalized epilepsy.
If no positive dynamics are observed as a result of treatment, or the condition is worsened by various side effects, the doctor may replace the drug with another one. Therapy can be considered successful when complete remission occurs (without attacks) within three years from the start of treatment, after which a dosage reduction is possible.
Generalized epilepsy today is not a death sentence for the patient, because a timely correct diagnosis and effective therapy allows the patient to significantly improve the quality of his life already in the first stages of treatment. Are you or your loved ones concerned about this disease? Experienced medical specialists are always ready to provide you with the necessary assistance and give you the opportunity to look into the future with confidence!
Epilepsy with isolated generalized seizures.
Epilepsy with isolated GSP is defined as a syndrome of idiopathic generalized epilepsy, manifested by a single type of seizure - primary generalized tonic-clonic convulsive paroxysms in the absence of an aura and a clear focus on the EEG. The onset of the disease is observed in a very wide age range: from 1 to 30 years with a maximum in the puberty period (average - 13.5 years). Clinically, GSP is manifested by a sudden (without aura) loss of consciousness with the patient falling, convulsions, eyeballs turning, and pupils dilating. First, there is a short tonic phase, which turns into a longer clonic phase, followed by post-ictal stunning. The duration of the GPS ranges from 30 seconds to 10 minutes (average 3 minutes). The frequency of attacks is low - from single per year to 1 time per month, without a tendency to a serial and status course. It is extremely characteristic that most attacks coincide with the period of awakening and, less often, falling asleep. The most significant provoking factor is sleep deprivation and sudden violent awakening. There may be an increase in attacks during the perimenstrual period. An EEG study in the interictal period may be within normal limits in half of the patients. Characterized by generalized peak-wave activity with a frequency of 3 Hz and higher, often with amplitude asymmetry or bifrontal predominance. Different regional patterns may emerge. Treatment. Remission is achieved in 75-80% of patients. Basic drugs are carbamazepine and valproate. In the absence of generalized peak-wave activity on the EEG, treatment begins with carbamazepine, which is more effective than valproate. When generalized convulsive attacks are accompanied by absences or myoclonic paroxysms, or when generalized peak-wave activity appears on the EEG, the basic drug is only valproate. The average dosage of carbamazepine is 15-25 mg/kg/day in 3 divided doses; valproate 20-50 mg/kg/day in 3 divided doses. Reserve drugs include barbiturates (phenobarbital 1.5-3.0 mg/kg/day in 1-2 doses; hexamidine, benzonal), hydantoins (difenin 4-8 mg/kg/day in 2 doses). In rare resistant cases, combinations are possible: carbamazepine + valproate; carbamazepine + barbiturates; valproate + barbiturates; barbiturates + hydantoins. With inadequate treatment, it is possible that absence seizures or myoclonic seizures may be added to GSP with transformation into juvenile myoclonic epilepsy.