Article:
Dysarthria is a complex speech disorder, one of its most common forms is bulbar.
The word “dysarthria” itself comes from the Greek “dys” - “disorder” and “arthroo” - “pronounce clearly”. Bulbar dysarthria manifests itself as slurred, slurred speech with a dull nasal tone. A child with this disorder speaks as if he has porridge in his mouth. A similar disorder occurs due to damage to the speech apparatus of the CNS (central nervous system). The first detailed description of dysarthria appeared more than a century ago. It was compiled by A. Oppenheim and H. Gutzmann. This disorder was studied in more detail in 1888 by A. Kussmaul.
What is bulbar dysarthria
Bulbar dysarthria is a person’s loss of articulate expressive speech caused by a disorder of the articulation apparatus by damage to the cranial nerves (IX, X, XII pairs). The clinical picture of this disorder is as follows:
- slurred speech;
- slow pace (braking);
- monotone;
- paucity of speech;
- dysphonia;
- the swallowing reflex is impaired.
The bulbar type of dysarthria can be established after speech therapy and neurological examination. To identify it, a number of examinations must be carried out - MRI, CT, cerebrospinal fluid analysis and others. The clinical picture of bulbar dysarthria depends on the lesion.
Reasons for the development of the disease
The main cause is damage to the bulbar nerves. If we consider from the point of view of anatomy, the glossopharyngeal nerve connects to the muscles of the pharynx, the vagus nerve to the palatine nerve, the hypoglossal nerve approaches the lingual muscle. Damage occurs precisely to these nerves. Experts identify the following causes of bulbar dysarthria:
| № | Factors of speech impairment | Manifestations |
| 1 | Perinatal factors | Complications during pregnancy, childbirth (improper position of the fetus, gestosis, premature birth, placental abruption, trauma during childbirth) |
| 2 | Head injuries | Bulbar dysarthria can develop due to traumatic brain injury of varying severity |
| 3 | Neoplasms in the brain | The growth of tumors in the brain disrupts the normal functioning of its parts. When localized in the speech department, compression of the bulbar structures occurs. Such tumors can be gliomas, medulloblastomas, benign formations |
| 4 | Neuroinfections | The most common of them are meningoencephalitis, viral encephalitis and others. The infection provokes inflammation and compression of the cranial nerve nuclei |
| 5 | Neurodegenerative processes | Destruction of the cranial nerve nuclei occurs |
| 6 | Encephalopathy and angiopathy | Occurs in somatic diseases (diabetes mellitus, abnormalities of cerebral vessels). As a result of such disorders, the blood circulation in the brain is destabilized. |
Before starting corrective work with bulbar dysarthria, it is necessary to accurately determine the cause of its occurrence. Without eliminating the cause, it is impossible to achieve complete restoration of speech and speech apparatus. Rehabilitation and reasons should be prescribed exclusively by specialized specialists in the field of speech therapy and neurology.
Symptoms
The main symptoms of bulbar dysarthria:
- The child's speech is slurred, inhibited, with poor articulation. The “R” sounds are replaced with fricative ones. Instead of the sound “B”, the sound “P” is pronounced “V”, the sound “P” changes to “F”.
- Consonant voiced sounds are completely or partially absent. Unstressed and stressed sounds are pronounced the same. The letter "A" sounds best.
- There is a noticeable rhythm disturbance. Speech sounds less emotional and monotonous. Expressive speech is not available to a child with dysarthria.
- The child often chokes and has problems swallowing when eating food and water.
- The child's voice is low and nasal.
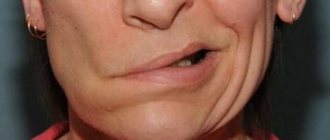
- Facial expressions are poorly expressed, facial asymmetry is observed (with unilateral nerve damage).
A child suffering from this type of dysarthria has simple slurred articulation. In some cases, voiced sounds disappear from speech. The deaf begin to dominate them. Speech loses its expressiveness and emotionality; it is not melodic. Expressive speech causes great difficulty for the patient and quickly tires him.
The exact symptoms depend on which cranial nerves are affected. In some cases, all of these symptoms may occur.
Myasthenia gravis - symptoms and treatment
Treatment methods for myasthenia gravis are divided into two groups:
- conservative - drug treatment, plasmapheresis, radiotherapy and enterosorption;
- surgical - removal of the thymus gland (thymectomy).
Drug treatments include: anticholinesterase drugs, anabolic steroids, ACTH (adrenocorticotropic hormone) and corticosteroids. As a rule, only one drug is used, since the use of several drugs is fraught with a cholinergic crisis.
Anticholinesterase drugs promote the accumulation of acetylcholine in synapses (as they prevent the destruction of the neurotransmitter), as a result, muscle strength increases [22]. They are administered intramuscularly and also taken in tablet form. The dose of the drug is selected individually.
Anabolic steroids are administered intramuscularly. They reduce the risk of generalization of the disease and are indicated in cases of intolerance to other methods of conservative therapy, as well as in the presence of contraindications to thymectomy [12]. The drug of choice is Retabolil.
ACTH stimulates the production of corticosteroids by the adrenal glands, which have anti-inflammatory and immunomodulatory effects [22]. They are used intravenously or intramuscularly. Glucocorticoids are considered more effective for the treatment of myasthenia gravis . Their use requires a significant reduction in the dosage of anticholinesterase drugs to avoid a cholinergic crisis.
Long-term use of steroids increases the risk of developing osteoporosis. Therefore, chest radiography is recommended [22].
Immunosuppressants artificially suppress the immune system to reduce antibody production [22]. They are the drug of choice in elderly people with acute myasthenia gravis, as well as in the treatment of patients with inoperable thymomas, contraindications to surgical treatment, ineffectiveness of acetylcholinesterase drugs and corticosteroids [9].
When treating patients with myasthenia gravis, plasmapheresis - taking and purifying blood and returning it or some part of it back into the bloodstream. This procedure allows you to reduce the amount of antibodies to cholinergic receptors in the bloodstream. It is recommended to be performed before thymectomy [12].
For the treatment of myasthenia gravis, intravenous administration of immunoglobulin G 5% and 10% is also used. They quickly but temporarily improve the course of the disease. Since the use of high doses of human immunoglobulins can suppress immune processes, immunoglobulins G can reduce the production of antibodies to cholinergic receptors.
If cytomegalovirus or Epstein-Barr virus is detected in a patient, the use of specific immunoglobulins for herpetic viruses is recommended [23].
Enterosorption can also be an effective method of treating myasthenia gravis. It involves taking medications, such as carbon fiber, to remove autoantibodies. It is most effective in the complex treatment of moderate myasthenia [24].
Thymectomy is performed in patients with thymoma in the absence of contraindications: myasthenic crisis and the presence of multiple metastases. Removal of the thymus gland in the absence of effect from conservative therapy is not justified, since myasthenia gravis is not always associated with pathology of the thymus gland [16].
Improvements after removal of the thymus gland may not occur immediately, but may take several months or years. Therefore, surgery is recommended to be performed when the patient’s condition is stable [22].
Radiological treatment methods include gamma irradiation of the thymus gland . It can be performed if there are contraindications to thymectomy or after removal of a thymoma. Complications of gamma irradiation include radiation dermatitis and pneumonitis [6].
Diagnosis of bulbar dysarthria
Diagnosis of bulbar dysarthria should be carried out only by specialists. To do this, it is necessary to conduct a number of specialized studies:
- Neurological examination. It allows you to determine the location of lesions of the cranial nerves. The doctor must assess the existing pathological process and its severity, as well as determine the causes of their occurrence.
- Speech therapy examination. The specialist evaluates the rhythm of speech and its speed, voice, mobility of the articulatory apparatus, and breathing rhythm during speech. Based on these data, the speech therapist chooses treatment tactics.
- CT studies, electroencephalography, ultrasound, MRI of the brain. It is necessary to obtain complete information about the pathology, the type of disorders, and on their basis decide on a correction program.
- Lumbar puncture. Necessary for identifying and identifying infectious pathogens.
The doctor may refer the child for additional tests and schedule consultations with other specialists. It may also be necessary to monitor the patient's health over time. Repeated studies may be required during the correction of dysarthria.
Also, the specialist must accurately distinguish the manifestations of bulbar dysarthria from pseudobulbar. The reason for the development of the second is damage to the corticobulbar nerves. To develop rehabilitation, it is necessary to exclude motor, dynamic and acoustic-mnestic aphasia from suspicion of diagnosis.
Symptoms of bulbar dysarthria
The symptoms that are observed with dysarthria are grouped into the following groups:
- Dysarthria differs from peripheral speech disorders in its pronounced spastic form and the absence of signs of muscle degeneration. A classic example of pyramidal dysarthria is pseudobulbar palsy. Atonic paralysis, which occurs when the motor nerve nuclei in the medulla oblongata are damaged, differs from peripheral paralysis by the presence of a number of other bulbar symptoms;
- Patients cannot perform articulatory movements with their lips. The movements of the tongue are limited, the soft palate is stretched very weakly, there is a dysfunction of the vocal cords in the larynx - they do not completely contact and do not close the glottis;
- During speech formation, coordination disorders appear, while isolated movements are completely normal. Movements of the tongue for a specific purpose are disrupted;
- Due to damage to the central part of the speech apparatus, dysarthric disorders appear in its higher areas, which relate to the melody of the word, the placement of rhythmic and dynamic stress. During acoustic analysis, speech therapists detect changes in the spectrum of individual sounds. Speech becomes unclear, slurred, and sluggishness of the respiratory and articulatory muscles is noted. This is detected by fluoroscopic examination during spoken speech and phonation.
In patients suffering from dysarthria, the rate of speech may be accelerated or slowed down. Patients place accents incorrectly. Due to insufficient function of the closing pharyngeal ring, an open nasal sound appears. Excessive contraction of the muscles of this ring is accompanied by a closed nasal sound. The articulation of speech is blurred, in rare cases it becomes explosive. Hoarseness and sometimes paretic aphonia appear (loss of sonority of the voice while maintaining the ability to speak in a whisper). Sometimes, due to too much closeness and compression of the vocal cords, patients develop spastic aphonia.
Treatment of bulbar dysarthria
Treatment of bulbar dysarthria has better results with parallel rehabilitation measures. A variety of specialists should take part in this work, depending on the causes and severity of the speech disorder. Corrective work consists of several components:
- Etiopathogenetic treatment. It is carried out if dysarthria is caused by infectious diseases. If tumors are present, a special treatment plan is developed together with neurosurgeons.
- Neurometabolic correction. This treatment is aimed at restoring the functioning of cerebral neurons and fibers.
- Speech therapy classes. Aimed at establishing correct sound pronunciation and subsequent automation. Special speech therapy exercises and breathing exercises are used. At later stages, the rhythm of speech and its expressiveness are corrected.
- Rehabilitation therapy. Restores motor skills and psycho-emotionality of the child. This is necessary for proper social adaptation. This work is carried out jointly with a psychologist and psychotherapist.
BULBAR PARALYSIS
BULBAR PALSY, a syndrome of damage to the glossopharyngeal, vagus and hypoglossal nerves or their motor nuclei located in the medulla oblongata, with peripheral paralysis of the muscles of the tongue, lips, soft palate, pharynx, vocal cords and epiglottis. The lesion can be bilateral or unilateral (to a less pronounced degree). Clinical manifestations: aphonia, dysphagia (especially liquid food that gets into the nose, the patient chokes), dysarthria, deviation of the tongue to the side or its immobility, lack of closure of the vocal cords, pharyngeal and palatal reflexes are not evoked. In the atrophied muscles of the tongue of the affected side, fibrillary twitching is observed (with damage to the nucleus of the hypoglossal nerve), impaired electrical excitability (degeneration reaction). The development of bulbar palsy depends on the underlying disease and can be acute and gradually progressive.
Acute bulbar palsy develops as a result of circulatory disorders in the medulla oblongata (thrombosis, embolism), intoxication, as well as acute compression (hematoma, upper cervical vertebra during a fracture or dislocation). In mild cases, the patient recovers, but his neurological impairment remains. With severe lesions, cardiac and respiratory disorders develop, which often leads to death. Progressive bulbar palsy is observed in amyotrophic lateral sclerosis, chronic poliomyelitis, tick-borne encephalitis, tumor of the posterior cranial fossa, craniovertebral anomalies, cicatricial adhesions, chronic cerebral circulatory failure due to atherosclerosis and hypertension. In this case, the motor nuclei of the cranial nerves are predominantly affected; the conduction systems usually remain intact. Disorders of swallowing, articulation, phonation, and later breathing also increase gradually.
Clinical variants are identified.
Duchenne
bulbar palsy (subacute anterior poliomyelitis). It manifests itself as disorders of swallowing, speech, salivation, breathing due to atrophic paralysis of the lips, tongue, nasopharynx and larynx. Characterized by a subacute progressive course without remissions; patients usually die during the first two years of the disease from respiratory and cardiac disorders.
Myasthenic bulbar palsy (Erb-Goldflam disease) develops as a result of conduction disturbances at neuromuscular synapses (see Myasthenia Gravis).
It is necessary to differentiate bulbar palsy from pseudobulbar palsy, in which there is no atrophy of the tongue muscles, increased pharyngeal and palatal reflexes, there are reflexes of oral automatism, and violent crying and laughter are observed. The diagnosis is made based on characteristic clinical symptoms. Treatment is aimed at eliminating the underlying disease and compensating for impaired vital functions. To improve swallowing, prozerin, glutamic acid, vitamins, ATP, nootropic drugs are prescribed, and for increased salivation - atropine; in case of respiratory failure - artificial respiration. When indicated, dehydration therapy is carried out, vasodilators and drugs that normalize blood clotting are prescribed. The prognosis is determined by the nature of the pathological process that caused the disease and the severity of clinical symptoms. Mostly unfavorable.