Cognitive processes
There are three types of cognitive impairment after a stroke:
- Damage to one of the cognitive functions: memory (amnesia), the ability to perform any actions (apraxia), impairment of visual, auditory, tactile perception (agnosia).
- Violation of several functions that generally do not affect social adaptation.
- Multiple injuries that lead to social maladaptation: impaired attention, memory, volitional processes. In this case, post-stroke dementia is diagnosed. In older people with dementia, household activity decreases and self-care skills are lost. This category of patients is at risk of recurrent stroke.
The first and second variants of the disorder can be corrected due to the plasticity of the brain: damaged functions are compensated by functions that remain intact.
Rehabilitation of older people with post-stroke dementia includes sessions with psychologists. With the help of special exercises, patients develop auditory and visual memory, the ability to concentrate, and solve logical problems. The recovery process is accompanied by drug therapy.
Rehabilitation after a stroke at home
After overcoming the acute period in the hospital, a rehabilitation period begins for a pensioner with a stroke. Relatives need to decide where it is better for an elderly person to undergo a recovery course: at home or in a rehabilitation center.
You may also be interested in the article: How to obtain patronage for an elderly person
If the family has decided to independently care for the patient after a stroke, they need to follow the recommendations of the attending physician and maintain constant contact with specialized specialists: a psychologist, a neurologist, a speech therapist.
At home, a separate place is assigned to a bedridden patient after a stroke. The bed is equipped with an anti-decubitus mattress. A small table is placed nearby, on which essential items are placed: a bottle of water, care products, a table lamp.
Specialists can come to the home 1-2 times a week, work with the patient and teach home methods of conducting developmental activities. The rest of the time, family members carry out the recommended exercises with the pensioner for 10-20 minutes several times a day. During weekly visits, specialists monitor the dynamics of changes, make additions and adjustments.
Motor abilities are restored using a complex of therapeutic exercises. Before performing the exercises, it is advisable for the patient to take a shower or bath to warm up the body. If there are contraindications to taking a bath or other difficulties, the affected areas are warmed with a heating pad. The muscles will be more flexible and there will be no pain.
Examples of gymnastic exercises:
- pulling up while lying on your back, holding the headboard of the bed;
- eye movements left and right, up and down with closed and open eyelids;
- alternately raising the right and left arms and legs;
- bending the knee and grabbing the shin with the hand;
- joint movements of healthy and motionless limbs to the right and left with a rubber ring put on them.
When carrying out therapeutic exercises, the pensioner’s condition is closely monitored. He shouldn't get tired. If such signs are observed, it means that the amount of stress does not correspond to the physical strength of the patient. We need to make an adjustment: reduce the pace and number of exercises.
Speech is restored by memorizing poetry and tongue twisters. At the initial stage, simple children's poems are chosen, which are easier for a pensioner to recite after a stroke. Gradually more complex material is selected.
Looking at family photographs can activate the process of remembering, since it is easier for the patient to recall the past in his memory. An elderly person remembers acquaintances and friends in the images, then the events associated with them. He tries to pronounce the names of the places he has visited, the objects he sees in the images.
Scientists believe that singing has a beneficial effect on people who have suffered a stroke. If they hear singing, sing together with loved ones, speech activity will be restored faster.
For rehabilitation to be successful, an elderly person should not be in a social “vacuum”: you constantly need to communicate with him, talk, ask questions, even if at first he cannot answer them. In this way, the patient’s desire to speak is stimulated, he remembers words and their meaning.
Chess, checkers, and dominoes are used to develop thinking abilities. In a family, even a small child can take part in restoring the health of a grandfather or grandmother by putting together puzzles, mosaics, or playing a board game.
A separate issue is the organization of nutrition for an elderly person after a stroke.
Excluded from use:
- alcoholic drinks;
- fatty and spicy foods;
- coffee, strong tea;
- sweets.
It is advisable to add to the diet:
- drink liquid of at least 1.5 liters. per day;
- increase consumption of fruits and vegetables;
- eat whole grains;
- replace sweets with dried fruits.
Food should consist of useful substances and be easily digestible so that the body is not overloaded.
It is useful to cook boiled vegetables, dishes from lean fish and meat, and porridge with low-fat milk. If there are paresis and problems with swallowing, the patient is fed through a tube with ready-made nutritional mixtures. As soon as the opportunity arises, you need to take the patient for a walk. Staying in the fresh air is good for brain activity, the body receives oxygen and vitamin D, and appetite appears.
You may also be interested in the article: How to choose a private facility for the elderly
The moral atmosphere in the house is of great importance. Patients who receive family support recover faster. If they experience hostility from others or rudeness, the healing process is slowed down. There is no need to criticize and laugh at clumsiness and awkwardness. Only with encouragement will an elderly person develop a strong desire to overcome the disease.
Consequences of a cerebral stroke
Cerebral stroke ranks second, after myocardial infarction, in the structure of mortality of the Russian population. Considering this fact, stroke belongs to the category of diseases that require mandatory rehabilitation measures - restorative treatment, which is also a guarantee against relapse of the disease.
Brain stroke, its types and risk factors
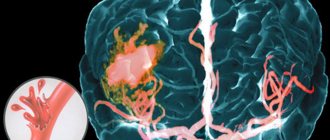
Depending on the cause of stroke, it is divided into three types: hemorrhagic, ischemic and subarachnoid. However, in medical statistics, ischemic stroke predominates (70–85%), when compression or blockage of blood vessels occurs as a result of thrombosis, embolism or other diseases of the blood vessels, heart or blood.
Unlike ischemic stroke, where there is compression of blood vessels, in the hemorrhagic type (20–25%) they rupture, followed by hemorrhage into the brain, under its membranes or into the ventricles. The least common (1–7%) is subarachnoid stroke, which is of a traumatic nature: due to rupture of an arterial aneurysm or traumatic brain injury. When it occurs, hemorrhage occurs in the space between the arachnoid and pia mater of the brain.
A stroke is considered an attack in which a neurological deficit (focal or cerebral) lasts more than a day; this period is called transient disturbances of the blood supply to the brain. A condition in which neurological functions are restored within three weeks is designated a minor stroke.
The mortality rate for different types of strokes varies, and on average is:
- for ischemic stroke – no more than 15%;
- for hemorrhagic stroke – no more than 33%;
- with subarachnoid hemorrhage - up to 50%.
You can reduce the likelihood of a stroke by not forgetting about the risk factors that are considered to be:
- age from 50 years (diet and sleep regime required);
- male gender;
- arterial hypertension (keeping a “blood pressure diary” is recommended);
- chronic heart diseases (timely examinations and surgical operations);
- transient ischemic attacks (considered to be harbingers of heart attacks and brain);
- type of work (for example, with high nervous stress);
- smoking (affects blood pressure);
- obesity and high cholesterol;
- diabetes;
- asymptomatic stenosis of the carotid arteries;
- stroke in direct relatives.
In Russia, risk factors include emergency hospitalization, which does not exceed 30% of all stroke cases, the lack of properly equipped intensive care units and failure to implement rehabilitation programs.
Primary stroke diagnosis and assistance
During the initial examination, the patient is asked to perform several actions:
- Extend your arms in front of you, palms up, with your eyes closed. If one of the arms begins to uncontrollably “go” down and to the side, this is a sign of a stroke.
- Raise both arms above your head. They should rise evenly to the same height.
- Stick out tongue. If it is modified (curved) and/or “falls” to the side, this is another sign of a stroke.
- Say one simple sentence. With a stroke, speech defects often appear, diction and articulation deteriorate.
- Smile. In a patient who has suffered a stroke, the smile will be distorted, and the corners of the lips will “look” in different directions.
If suspicions of a stroke are confirmed, you must immediately call an ambulance and inform doctors about the symptoms noticed, regardless of their disappearance or intensification. Hospitalization is needed urgently: in the hospital, MRI, transcranial Doppler ultrasound, MR spectroscopy and other types of studies that will confirm or refute fears should be performed.
If signs of a stroke are detected, after calling an ambulance, first aid must be provided, which consists of several actions:
- raise the patient's head above body level by 30 degrees;
- loosen tight clothing: belts, collars, etc.;
- measure pressure;
- take a medicine that normalizes blood pressure from those that have already been used by the patient previously;
- if you don’t have the necessary medications on hand, you can put your feet in a basin of moderately hot water;
- turn the patient onto the right side (place a tray under the lower jaw if there is vomiting).
After completing all the steps, it is recommended to open the front door in advance and wait for the ambulance team to arrive. And after her arrival and the patient’s reluctance to go or the paramedics to take him to the hospital, insist on immediate hospitalization.
Symptoms and consequences of stroke
As a result of the death of nerve cells in the brain from oxygen starvation, neurological disorders occur during a stroke, which, depending on the type of stroke, may initially lead to dizziness, weakness or loss of consciousness, up to the development of a coma, as well as perspiration on the forehead, pulsation of the cervical arteries, a sharp drop in pressure, vomiting, hoarse unnatural breathing, rare pulse, numbness of the limbs, pallor, pain in the head and sometimes in the heart area. Symptoms may be more or less pronounced, depending on the location of the circulatory disorder and its extent.
A stroke can occur in three variants: favorable (consciousness is restored after a few minutes or hours), intermittent or progressively severe (when consciousness returns only after three days or more). With a favorable prognosis of treatment for a stroke, over time it is possible to restore all impaired brain functions; in the intermittent variant, most of the disorders are subject to restoration, although a recurrent stroke and the addition of additional diseases are possible: pneumonia, heart disease. The progressive course of a stroke is accompanied by an increase in symptoms and often ends in death.
Neurological disorders typical of a stroke include partial or complete paralysis, speech defects or complete loss, visual impairment, hearing impairment, and memory loss.
The consequences of a stroke cannot be avoided, but conditions can be created for partial or complete recovery. Among these conditions the following should be highlighted:
- quick and correct diagnosis;
- immediate hospitalization;
- compulsory rehabilitation.
Of course, there are factors that a person cannot influence, such as the strength and type of stroke, its location and extent, with the exception, perhaps, of careful attention to risk factors and preventive actions.
Rehabilitation after stroke
In Russia, no more than 20% of patients who have suffered a stroke are admitted to rehabilitation centers and departments. The rest are either treated at home or do not undergo active rehabilitation programs at all. Moreover, statistics show that early thirty-day mortality in patients after a stroke occurs in 43% of cases if they were treated at home, and 24% if they were treated in a hospital.
- pedagogy;
- psychotherapy;
- drug therapy;
- occupational therapy;
- speech therapy;
- physiotherapy;
- kinesiotherapy;
- acupuncture;
- manual therapy and massage;
- hirudotherapy;
- dietetics, etc.
It is very important to conduct active rehabilitation programs in environmentally friendly places where fresh, unpolluted air is available. After all, the human brain consumes up to a quarter of all inhaled oxygen, and after a stroke, the requirements for air quality increase.
People who have had a stroke often experience neurocognitive problems such as sudden mood changes or fatigue. All this requires rehabilitation in conditions as close as possible to home ones, reproducing not only everyday coziness and comfort, but also ensuring attentive attention from all service and treatment personnel.
The rehabilitation center uses traditional, latest and original recovery methods for people who have suffered a stroke.
Extensive practice and rich knowledge of the treating staff in the field of rehabilitation medicine allow us to provide comprehensive rehabilitation at the highest level, meeting Western standards.
Rehabilitation service. located in a picturesque coniferous forest, corresponds to the status of a four-star hotel with 35 single rooms. The fruits of the joint work of a nutritionist and the chef of the Three Sisters restaurant, who knows how to make balanced nutrition tasty, will not leave anyone indifferent.
Persons Ministry of Health of the Moscow Region
No. LO-50-01-003671 dated August 29, 2012
There are contraindications. Consult your doctor.
Recovery in a boarding house
Rehabilitation of an elderly person after a stroke at home requires the full-time employment of one of the relatives for the next six months. While the patient is bedridden, he cannot be left at home alone for two reasons: he is helpless and it is necessary to deal with him several times a day. The volume of care is so large and multidirectional that soon the caregiver himself will need support and replacement.
In boarding houses for the elderly, professionals are involved in the rehabilitation of patients. Special equipment is used for treatment. An individual program is developed for each patient. Restoration methods that have been developed over the years produce positive results within a month.
Ischemic stroke or cerebral infarction
Ischemic stroke, or cerebral infarction, is an acute condition in which cerebral circulation is impaired, accompanied by damage and softening of tissue, changes in brain function due to the cessation of blood supply to its areas.
The disease is characterized by a sudden onset and an increase in symptoms over the course of a day.
During this period, death or a significant reduction in a person’s vital abilities occurs. A period of 28 days from the onset of the first signs of stroke (acute period) is also considered dangerous. At this time, about 35% of initially surviving patients die.
Commitment to stroke
Among all strokes, ischemic ones account for about 85%. Over the course of a year, more than 5 million people worldwide die from this disease; in Russia, more than 400 thousand become completely disabled; approximately 40% of those who survive survive and only 8% are able to return to full-time work.
People over 45 years of age are most susceptible to strokes, more often men. In recent years, there has been a trend towards the development of cerebral infarction among young people - 30 years and older.
Pathogenesis: what happens during an attack?
The degree of damage to brain tissue depends on the duration and extent of the decrease in cerebral blood flow. The optimal intake is 50-60 ml. blood per 100 g of brain tissue per minute. If this figure drops to 35 ml. There is a violation of glycolysis (the breakdown of glucose), which leads to a change in the state of the cerebral cortex.
If the blood flow volume decreases to 15 ml. this causes rapid irreversible damage to neurons and the formation of an infarct area (softening).
Progression of the disease is observed due to further disruption of the blood supply to the area adjacent to the damaged area. The final formation of the ischemic area ends after 56 hours.
Pathological processes are accompanied by cerebral edema, increased intracranial pressure, as well as the migration of leukocytes into tissues and their damage to healthy cells. A common cause of death in patients is compression of the medulla oblongata or cerebellum by swollen tissue.
Causes of the disease
The disease is preceded by disruption of the activity of cerebral vessels as a result of the pathological influence of certain diseases. The carotid, vertebral and cerebral arteries and their branches are predominantly affected.
The etiology of ischemic stroke includes the following factors:
- Vascular atherosclerosis.
- Thromboembolism.
- Diabetes.
- Congenital vascular pathologies.
- Hypertension.
- Rheumatism.
- Vasculitis.
- Carotid artery stenosis with progression of osteochondrosis, spondylosis.
- Infectious and allergic arteritis.
- Blood diseases (for example, leukemia).
- Diseases of the heart muscle (defects, coronary disease).
- Severe renal dysfunction.
- Bronchial asthma.
Often, a hemorrhagic stroke resulting from a rupture of an aneurysm is complicated by an ischemic one.
Old age and a hereditary predisposition to vascular diseases also affect the incidence of strokes.
The following can serve as a trigger for the development of the disease or long-term aggravate the condition of the blood vessels:
- stress;
- smoking;
- abuse of fatty foods, obesity;
- alcoholism.
Classification
Depending on the period of occurrence, strokes can be:
- Primary (developing for the first time in life).
- Secondary (repeated ischemic stroke in a patient who previously had the disease).
According to etiology, ischemic strokes are distinguished as follows:
- Thromboembolic (occur due to blood thickening and impaired blood supply to the brain).
- Cardioembolic (resulting from myocardial infarction or heart valve disease).
- Hemodynamic (develop due to spasm of cerebral vessels, for example, due to abnormal blood pressure).
- Lacunar (observed when small arteries are affected - up to 15 mm.).
According to severity, strokes are:
- Transient ischemia (focal disorders that regress within 1 day).
- Small strokes (symptoms of the disease regress within 21 days).
- Progressive stroke (a disease with an increase in symptoms up to 3 days).
- Total stroke (formed area of cerebral infarction).
Periods of ischemic stroke:
- very acute (3 days), including the first 3 hours – the “therapeutic window”, when brain cells are able to recover subject to the restoration of blood supply;
- acute (28 days);
- early recovery (6 months);
- late recovery (2 years).
Symptoms and common signs of stroke
The clinical picture is largely determined by the area of brain damage . Most strokes occur in the carotid region as a result of dysfunction of the middle cerebral and carotid arteries. If the disease develops due to occlusion of a large artery, an extensive ischemic stroke is possible when the area of softening of the brain is large. This entails an immediate increase in the clinical picture of a stroke, most often leading to death in the first hours.
A stroke can occur at any time of the day, more often after drinking alcohol, stress, or swimming in hot water.
Depending on whether the patient has a left- or right-sided stroke, symptoms may affect only one side of the body.
Focal neurological symptoms of the disease, increasing over 3-4 hours, several weeks or developing at lightning speed:
- leg weakness;
- numbness of hands;
- unilateral decreased vision, strabismus;
- paresis and paralysis of organs in one part of the body (feet, hands);
- violation of flexion, grasping reflexes, fine motor skills;
- urinary retention;
- inability to swallow, chew;
- hearing and speech disorders;
- failure of respiratory functions;
General cerebral symptoms of stroke do not occur in every case and are determined by the degree of development of edema, more often
- for bilateral strokes:
- vomit;
- clouding of consciousness;
- severe headache;
- dizziness;
- overexcitement;
- falls;
- disorientation in space;
- mental disorders;
- decreased or absent sensitivity;
- increased body temperature, sweating;
- in the case of a major stroke, coma may develop.
Consequences and complications for humans
Complications that often accompany the course of a stroke and can cause the death of the patient are:
- pneumonia;
- myocardial infarction;
- renal failure;
- thromboembolism;
- dehydration, bedsores.
After an ischemic stroke, the patient's condition is caused by changes in the left hemisphere of the brain.
Health consequences may include:
- Inability to swallow food.
- Partial, complete loss of vision.
- Deviant behavior – aggression, phobias, reluctance to communicate.
- Incontinence of feces and urine.
- Mental and cognitive disorders.
- Headaches, seizures, epilepsy.
With a stroke of the brain stem or other significant parts, surviving patients often completely lose functions coordinated by the nervous system, which leads to disability with the inability to self-care.
Prognosis for recovery
The prognostic calculation for the preservation of life and recovery depends on the volume of cerebral infarction, as well as the location of its localization.
A third of people die within a month after the onset of the disease, most of them 1-2 days after the attack.
The lowest incidence of deaths is among patients with lacunar stroke (only 2%). Only a small proportion of patients recover completely. The majority of people who have suffered an ischemic stroke and survived become disabled to varying degrees of severity. Restoration of basic vital functions is possible within 1 year after the episode of illness. The 5-year survival rate is about 50%. A recurrent stroke develops in 30% of people.
Diagnosis
During a physical examination, the doctor evaluates the signs of the disease, notes murmurs in the heart and carotid artery, and the difference in pressure measured on the left and right arms. A person's medical history can help determine the cause of an ischemic stroke.
Instrumental research methods are ultrasound with Doppler sonography, angiography, CT or MRI of the brain. An ECG, ultrasound of the heart, and laboratory tests (general clinical, biochemical) are required. The disease is differentiated from hemorrhagic stroke, tumors, inflammatory diseases or toxic brain lesions.
First aid for stroke
First aid to the patient should be provided immediately after the first symptoms of the disease are detected. The person must be placed in bed, preventing any movement. In case of loss of consciousness, it is necessary to revive him with the help of ammonia, wine vinegar, and splashing cold water on the face.
To avoid tongue sinking, the head should be slightly higher than the level of the body. Feet and hands can be rubbed with a soft brush or a towel moistened with warm water.
Treatment options
The patient is urgently hospitalized, after which emergency therapy is performed (can also be carried out by an ambulance team):
- Improving blood circulation in the stroke area - reopolyglucin drip.
- Normalization of neuronal metabolism - cerebrolysin, nootropil intravenously.
- Reducing blood pressure - Relanium, droperidol, dibazol intravenously.
The complex of treatment measures for stroke includes:
- Normalization of respiratory function using air ducts, sometimes tracheostomy, intubation.
- Relieving pulmonary edema - cardiotonic drugs, oxygen inhalations, sodium bicarbonate injections.
- Reducing cerebral edema - glucocorticosteroids, mannitol, Lasix injection.
- For fever - a solution of amidopyrine, analgin, diphenhydramine, novocaine.
- Improving cerebral circulation - nootropic, vasodilating, antiaggregation agents.
- Planned correction of blood pressure.
- With a sharp decrease in pressure - solutions of mezaton, korglykon, norepinephrine intravenously.
- Prevention of dehydration – up to 2.5 l. saline solution with glucose per day, drip.
- For potassium deficiency - injections of potassium chloride, potassium nitrate.
- Reducing vascular permeability - ascorbic acid in the form of injections.
- If pneumonia develops, use antibacterial therapy.
- In case of urinary retention - catheterization and lavage of the bladder.
- To avoid bedsores, wipe the patient’s skin with camphor alcohol, antiseptics, and turn over 4 times a day.
- After removal of acute symptoms - anticoagulant therapy (heparin, phenylin, ecofemin, fibrinolysin), administration of antihypoxants (phenobarbital, gutimin), neuroprotectors.
- In some cases, surgical intervention may be necessary, the purpose of which is to reduce intracranial pressure and restore cerebral blood flow.
After the patient leaves the hospital, lifelong prevention of recurrent strokes is recommended:
- taking antihypertensive drugs, antiplatelet agents, anticoagulants, muscle relaxants, antioxidants, lipid-lowering drugs;
- correction of blood glucose levels;
- treatment of heart rhythm disorders.
The patient undergoes examinations several times a year by a neurologist and other specialists, and also adheres to a diet and engages in exercise therapy.
Lifestyle and rehabilitation
After a person is placed in a rehabilitation ward, bed rest is gradually replaced by ward rest, and then by free rest. After 2-3 months he is discharged from the hospital. The best option for recovery after a stroke is to visit a specialized sanatorium. At home, mandatory measures to maintain and improve the health of a stroke survivor are:
- Massage, electrical stimulation of muscles.
- Acupuncture.
- Passive and active gymnastics (twice a day for 40 minutes).
- Water procedures.
- Learning to walk or use a wheelchair.
- Providing tube feeding in case of swallowing dysfunction.
- Use of diapers or convenient location of the patient near the toilet.
- Skin care.
- Classes with a speech therapist.
- Psychotherapy, fight against depression.
- Teaching self-care skills, writing, reading, counting.
- Occupational therapy.
The patient's relatives should monitor any changes in his condition, since the risk of a recurrent stroke at first is very high.
Diet after stroke
The main goal of the nutritional system is to reduce animal fats and salt in the diet, as well as normalize weight.
Products allowed for consumption after a stroke:
- any vegetables, fruits;
- juices;
- fermented milk food (low fat);
- lean meat, fish;
- cereals;
- fructose-based sweets;
- compotes, jelly, herbal infusions.
You should eat bananas, citrus fruits, dried apricots, carrots, and cabbage as often as possible. Drinking regime – up to 1 liter. liquids per day.
Foods recommended for exclusion:
- fat meat;
- eggs;
- fatty dairy products;
- baked goods, sweets;
- marinades, pickles;
- smoked meats;
- over-salted food.
Treatment with folk remedies
During the rehabilitation period, it will be useful to give the patient remedies prepared according to folk recipes:
- To improve the functioning of the nervous system - tincture of marina root (1 liter, 3 times a day).
- For the same purpose - mumiyo (according to the instructions).
- Visual and hearing impairments can be eliminated by regular intake of infusions of hawthorn berries, walnut partitions, birch leaves, and onion peels.
- Every day you need to consume pollen, as well as 1 spoon of lemon juice and beet juice.
- Restoration of paralyzed limbs: infuse 3 l. bay leaf per 200 ml. vegetable oil 7 days. Then lubricate the affected areas daily.