Shabunina Ekaterina Mikhailovna
Neurologist, category 2
1. How does dizziness manifest in osteochondrosis?
2. How are dizziness and cervical osteochondrosis related?
2.1 The main causes of the development of osteochondrosis
2.2 The main causes of dizziness in osteochondrosis
3. Clinical picture
4. Diagnostics
5. How to treat?
6. Prevention
Without a doubt, one of the most common symptoms is dizziness. This symptom occupies a leading place in prevalence and is associated with a number of pathological conditions and diseases, which indicates its nonspecificity; however, there are some types of dizziness that occur only in certain conditions, for example, cervicogenic dizziness with pathology of the cervical spine. A symptom such as dizziness can occur with a wide range of neurological, vascular and mental diseases and require a mandatory diagnostic and therapeutic approach, as it is often a symptom of a serious and even life-threatening disease.
The appearance of systematic dizziness occurs in more than 35% of people living in large populated areas. Very often, dizziness accompanies neurological and vascular diseases and can be a harbinger of the development of transient or acute cerebrovascular accident. In more than half of the cases, the occurrence of constant sluggish dizziness is formed against the background of diseases of the musculoskeletal system.
How does dizziness manifest in osteochondrosis?
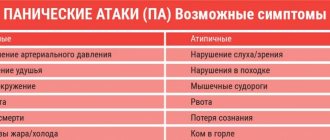
Dizziness, or synonymous with vertigo, is a pathological feeling of uncertainty in assessing the position of one’s body in space, while the sick person feels as if the objects surrounding him are rotating around him, less often the sensations are of the opposite nature, i.e. the feeling of rotating your own body around surrounding objects. These sensations lead to uncertainty in one’s actions, disrupt motor skills and cause awkwardness in the patient’s movements. With fairly severe manifestations of dizziness, in addition to the main symptom - uncertainty in movements, neurological symptoms are added in the form of nausea and even vomiting with severe dizziness. The patient also experiences some autonomic disorders, such as:
- Increased heart rate and pulse;
- Unstable blood pressure;
- Increased sweating, especially of the upper extremities and face;
As dizziness increases, all of the above accompanying symptoms also progress proportionally and become more pronounced.
In neurological practice, it is very convenient to divide dizziness into several main types, depending on the pathogenetic mechanism of its formation. The following types of vertigo are distinguished:
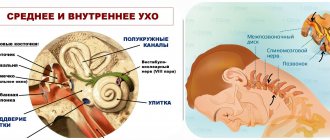
- Systemic dizziness. Such dizziness has a vestibular cause and occurs when moving the head. The patient feels dizziness in the form of falling or continued rotation in response to head movement. Very often, systemic dizziness is complemented by severe hearing problems.
- Syncope or presyncope. Dizziness is a common symptom and warning sign of impending loss of consciousness. Dizziness occurs and increases along with a general deterioration in clarity of consciousness. The person becomes unstable, loses balance, and notices cloudiness or darkening in the eyes. If this condition occurs, the victim may fall and cause serious injury to himself.
- Neuralgic cerebrogenic dizziness. It occurs as a result of organic pathology with localization in the parts of the brain responsible for balance. For example, when the cerebellum is damaged in a person suffering from a stroke or traumatic brain injury, cerebellar ataxia occurs, one of the manifestations of which is constant dizziness. In other cases, cerebrogenic imbalance occurs due to paresis or paralysis, but in this case the feeling of dizziness is false.
- Cervicogenic dizziness. Such dizziness occurs with pathology of the cervical spine, most often with osteochondrosis. The formation of a feeling of awkward body position in space occurs as a result of a violation of proprioceptive sensitivity in the peripheral nervous system. It is the occurrence of dizziness of a cerebrogenic nature that is most often observed in patients.
About cervical vertigo
About the article
46082
0
Regular issues of "RMZh" No. 10 dated May 29, 2004 p. 578
Category: Neurology
Authors: Gorbacheva F.E. , Matveeva L.A. , Chuchin M.Yu.
For quotation:
Gorbacheva F.E., Matveeva L.A., Chuchin M.Yu. About cervical dizziness. RMJ. 2004;10:578.
It is well known that dizziness is a very common complaint among patients of various age groups. Most often it bothers elderly and mature people, but it also occurs among young people, adolescents and children. There are many causes of dizziness, from serious to easily treatable. First of all, it is necessary to clarify what the patient means by the sensation experienced, interpreted as dizziness. Dizziness is often referred to as a disorder of balance and instability, in other cases it refers to a pre-fainting state. True (vestibular, systemic) dizziness is a sensation of imaginary movement of surrounding objects or one’s own body, i.e. illusion of non-existent movement, rotation, “falling through” of the patient or the environment. Systemic vertigo is caused as a result of dysfunction of different parts of the vestibular system - both its peripheral part (semicircular canals, vestibular nerve) and central parts (vestibular nuclei of the brainstem, parietotemporal parts of the cerebral cortex). The vestibular system performs the complex function of maintaining body balance when performing various voluntary and involuntary movements (kinetic loads) and maintaining and changing posture (postural loads). This function is successfully carried out by the vestibular system due to its numerous connections with other parts of the neural system - visual, proprioceptive, cerebellar, extrapyramidal, cortical and spinal. When performing the balance function, the initial impulse comes from the peripheral receptors of the semicircular canals of the labyrinth, from there, through the vestibular nuclei of the brain stem (in particular, the lateral vestibular nuclei), due to their numerous connections with other systems, complex mechanisms for creating balance are activated at each specific moment of the movement - walking, running, changing direction and pace of movement. Of decisive importance is the transmission of impulses from the lateral vestibular nuclei (LVN) to the motor spinal structures through the vestibulo- and reticulospinal tracts, which correct the tonic tension of skeletal muscles, reducing the tone in some muscle groups and increasing it in others, creating a stable equilibrium position.
Damage to the vestibular apparatus leads to three characteristic symptoms - dizziness, nystagmus and impaired coordination of movement (ataxia).
Automatic and conscious spatial orientation suffers - the patient creates a false sensation of displacement of his own body and surrounding objects - the illusion of rotation, movement.
Damage to the vestibular apparatus is accompanied by a disruption of normal reciprocal muscle tone. Movements are deprived of normal regulatory influences and their incoordination occurs - vestibular ataxia, an unsteady gait appears, and falls may occur. A certain place among the systems involved in maintaining balance is occupied by the system of proprioceptive sensitivity.
The greatest flow of impulses to the PVN comes from the structures of the neck - bone-ligamentous, joint and muscle receptors, which increases even more with pathological changes in the neck, in particular, the cervical spine (with osteochondrosis, spondylosis, etc.) Dizziness provoked by movements in the neck has long been attracted attention and was called “cervical vertigo.”
(Dix, 1989). Over the years, various researchers have tried in one way or another to explain the occurrence of dizziness in cervical pathology, but the proposed aspects of the pathogenetic mechanisms remained hypothetical. It was believed that vestibular symptoms in cervical spondylopathies arise from irritation of the cervical sympathetic plexus, resulting in insufficient blood supply to the labyrinth. Another opinion suggested increased excitability and increased proprioceptive impulses from the cervical structures as a result of degenerative changes in the osseous-ligamentous apparatus. It was assumed that these disturbances in somatosensory input cause disturbances in spatial orientation, vertigo and nystagmus, especially during movements of the head and neck (De Yong, 1967). However, many supported the vascular theory of the occurrence of disorders caused by transient ischemia of the labyrinth as a result of compression of the vertebral artery or periarterial sympathetic plexus in the bone canal. Gradually, the concept of vertebrobasilar insufficiency (VBI) replaced the previously existing theory of vascular spasm, and the appearance of dizziness and/or instability began to be explained from this position. Among diseases of the cervical spine, the most common are degenerative processes:
osteochondrosis and spondyloarthrosis.
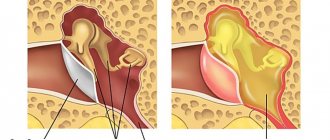
Under the influence of mechanical loads, changes occur not only in the intervertebral discs, but also reactive changes in the adjacent vertebral bodies, their ligamentous apparatus and muscles. Growing osteophytes have different directions and localizations. These manifestations of spondylosis are found both on the anterior surface of the vertebral bodies and on the posterior, and are directed towards the spinal canal and the canal of the vertebral artery. The latter is easily injured with uncovertebral arthrosis. Traumatization of the spinal roots and their membranes causes pain in the cervical-occipital region and shoulder girdle, pain in the arms, and numbness in them. The above disorders occur after prolonged forced positioning of the head and neck, as well as after sleep. Often there is a persistent limitation of neck mobility in one or several directions due to reflexively tense neck muscles. Thus, in cervical osteochondrosis, the leading clinical syndrome is pain, and the source of pain impulses is the receptors of the fibrous ring of the disc, ligamentous apparatus, joint capsule, and tense muscles. If osteophytes develop in the bony canal of the transverse processes of the cervical vertebrae, then irritation of the periarterial sympathetic plexus around the vertebral artery can be expected when bending or turning the head. In this situation, it is possible to develop dizziness, headaches and visual disturbances - i.e. posterior cervical sympathetic syndrome. Dizziness caused by cervical spondylosis can develop when the vertebral artery is compressed during manipulation of the neck. However, in addition to dizziness, other symptoms are observed due to ischemia of the brainstem-cerebellar structures, such as: diplopia, dysarthria, cerebellar disorders. Rare causes of attacks of dizziness and balance disorders are congenital anomalies of the cervical spine and posterior cranial fossa.
Their clinical debut often occurs in childhood and adolescence, less often in young and adulthood.
In type 1 Arnold-Chiari malformation, the mentioned attacks of systemic dizziness are often isolated complaints of patients. At the same time, in patients with degenerative-dystrophic changes in the cervical spine, when suddenly turning the head, “pushes to the side” and instability are often observed, which can lead to a fall. In this case, the patient experiences an inexplicable feeling of spatial disorientation, which he interprets as “dizziness,” but without a clear sense of the imaginary movement of the surrounding. The basis of this “cervical vertigo” is (mainly) imbalance and vestibular ataxia. Currently, there is a widespread belief about the leading role of cervical osteochondrosis and vertebrobasilar insufficiency in the development of attacks of dizziness or instability in elderly and mature people. Nevertheless, the hypothetical nature of this situation continues to persist. positional vertigo
) is unreasonably often explained by pathology of the cervical spine (“cervical vertigo”) .
The clinical picture of DPG is clearly defined and the causes of its occurrence are clarified. DPG occurs when position changes, i.e. movement of the head and neck. This is paroxysmal dizziness that develops when throwing the head back, bending down; the attack of dizziness is strong, but short-lived - within a few seconds; when the position of the head that caused the attack changes, it disappears. The causes of DPG are deposits of calcium carbonate crystals that appear with age, sometimes after trauma, in the semicircular canals of the labyrinth (so-called cupulolithiasis); when the position of the head changes, they irritate the receptor apparatus of the labyrinth, as a result of which an attack of dizziness occurs. The condition is diagnosed using fairly simple Dix-Hallpike tests. Attacks of systemic vertigo that occur in people over 45 years of age, accompanied by nausea and vomiting, horizontal or horizontal-rotatory nystagmus (Menière-like), are also often explained by “cervical vertigo” as a result of osteochondrosis or VBI. Currently, using electrocochleography, it has been established that in a significant proportion of cases they are caused by hydrops of the labyrinth, which, in contrast to idiopathic hydrops in Meniere's disease, is called secondary, i.e. developing against the background of various, often somatic, pathologies. Thus, in our opinion, “cervical dizziness” can only be attributed to those cases when, in persons with severe osteochondrosis or other pathology of the cervical spinal segment, when turning the head, there is an imbalance and even a fall (which patients usually explain by dizziness, although it is not one). The mechanisms of these balance disorders can be explained by Magnus stem reflexes, which occur with the participation of vestibuloreticular structures of the brain stem. A powerful flow of afferent impulses from the proprioceptors of the neck is directed to the LVN, as a result of which there is a sharp increase in muscle tone in the ipsilateral muscles of the trunk and limbs and a decrease in the contralateral muscles, resulting in an imbalance. Since the starting point of impulses to the muscles of the trunk and limbs are the PVN, it is advisable to influence their receptor apparatus in order to reduce the efferentation that causes balance disorders. The histaminergic system plays an important role in the functioning of the vestibular structures (in particular, the LVN). Therefore, if there is an imbalance, as is observed with “cervical dizziness,” the use of antihistamines is justified. , betahistine hydrochloride (Betaserc)
, has been used with the greatest therapeutic effectiveness .
The drug blocks H3 and stimulates H1-histamine receptors. By blocking H3 receptors, Betaserc increases the release of neurotransmitters from the nerve endings of the presynaptic membrane (which is prevented by histamine), thereby exerting an inhibitory effect on the vestibular nuclei of the brain stem. Betaserc has proven itself positively in Meniere's disease and other causes of vestibular dysfunction. Studies conducted to evaluate the effectiveness of the drug, including double-blind studies, indicate the high effectiveness of betahistine dihydrochloride in this disease. At the time of an attack, taking 2-3 Betaserc tablets helps relieve dizziness. For Meniere's disease, Betaserc can be prescribed for a long time, as it is not addictive, does not have a toxic effect on the body, does not have a sedative effect, and does not affect blood pressure and heart rate. Long-term use of Betaserc can stop the progression of the process. In addition, if you have Meniere's disease, it is recommended to limit your coffee intake and stop smoking. The drug reduces the frequency of attacks of systemic dizziness and reduces balance disorders. The great advantage of Betaserc is the fact that it can be taken for a long time, since it has no toxic effect on the body, does not cause a sedative effect, does not affect blood pressure and heart rate, and what is especially important is that it is not addictive. The daily dose of the drug for adults is 48 mg in 3 divided doses. The tablet contains 16 mg of betahistine dihydrochloride. Literature
1. Diseases of the nervous system. Ed.N.N.Yakhno, D.R.Shtulman, ed. 2. M. Medicine, 2001 2. Dizziness. Ed.M.R.Dix, J.D.Hood.M, Medicine, 1989 3. Afanasyeva S.A., Gorbacheva F.E. Isolated systemic dizziness. Neurological Journal. v.8, no. 4, 2003, 36–40 4. Barre JA Sur un syndrome Sympathique cervical posterieur et sa case frequente: l'arthrite cervicale. Revue de Neurologie. 1926, 45, 1246–1253 5. Fisher FE Vertigo in cerebrovascular disease. Arch. of Otolaryngology, 1967, 85, 529–534 6. Barany R. Diagnose von Krankheitserscheinungen im Bereich des Otolithenapparates. Acta Otolaryng. 1921, 2, 434–437 7. Dix MR, Hallpike CS The Pathology, Symptomatology and Diagnosis of Certain Common Disorders of the Vestibular System. Ann. of Otology, 1952, 61, 987–1016 8. Brandt T. Vertigo. Its Multisensory Syndromes. 2nd ed. Springer, London, 2000. p.441–451
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
How are dizziness and cervical osteochondrosis related?
Osteochondrosis is one of the most common and frequent causes of dizziness. With this disease, damage occurs to the cartilage tissue of the intervertebral discs of the cervical spinal column as a result of a violation of their nutrition or trophism. As a result of disturbed metabolism, dystrophic processes are formed in cartilage tissue, which leads to a decrease in the volume of cartilage and its destruction, as a result of which the spinal column loses a significant degree of its shock-absorbing properties. The load on the bodies of the cervical vertebrae increases, which leads to their mechanical trauma and subsequent destruction. Bone growths or spines appear on the vertebrae, the mobility and mobility of the vertebrae is significantly reduced, and their height also decreases, which leads to the gradual involvement of spinal cord neurons and their processes in the inflammatory process, which exit through the lateral openings between the vertebrae in the form of sensory and motor nerve fibers as part of nerve roots. In the absence of timely diagnosis and treatment, osteochondrosis progresses and leads to the development of serious complications in the form of organic damage to nervous tissue, one of the symptoms of which is the development of cervicogenic dizziness.
The main causes of the development of osteochondrosis
Osteochondrosis is a multifactorial disease and it is not possible to identify any specific factor leading to its occurrence. However, among a wide range of pathogenic factors, several leading factors can be identified, which include:
- Hereditary genetic predisposition;
- Systematic long-term physical inactivity or, conversely, increased load on the musculoskeletal system;
- Dysmetabolic disorders;
- History of chronic infectious diseases.
All of the above factors can lead to the development of osteochondrosis, both individually and in combination. When exposed to two or more factors from the above list, the risk of gradual formation of osteochondrosis increases significantly.
The main causes of dizziness in osteochondrosis
Whether dizziness can occur with cervical osteochondrosis is a complex question. Of course, in most clinical cases this symptom is present, but there are also situations when osteochondrosis progresses in a latent form without dizziness and other vegetative manifestations. It is important to immediately note that only osteochondrosis of the cervical spine is accompanied by the appearance of the symptom of dizziness. As mentioned above, osteochondrosis leads to a decrease in the area and volume of the intervertebral discs, which leads to its flattening and compression or compression of the spinal nerve endings, while in addition to the direct effect on the nervous tissue, compression of the vertebral or vertebral arteries occurs, which entails a chronic impairment of oxygenation nervous tissue of the spinal cord and medulla oblongata. The complex effect of chronic ischemia and trauma to nerve fibers leads to increased sensitivity and irritation of autonomic nerve endings, resulting in cervical dizziness.
The diagnosis of cervical osteochondrosis is a myth.
Competent doctors know that the diagnosis of cervical osteochondrosis is one of the most persistent myths in medicine. And those who are less knowledgeable blame a great many problems on osteochondrosis, including panic attacks and symptoms of VSD.
Scientists have long discovered that osteochondrosis is a natural process of aging of the body. Even teenagers have signs of osteochondrosis on x-rays!
We inherited osteochondrosis from our ancient ancestors homo erectus (homo erectus), this is a natural consequence of the evolution of our species and the acquired ability to walk upright.
In fact, osteochondrosis itself does not contribute to the development of VSD and panic attacks and does not give rise to any pronounced clinical complaints. Even neck pain is not a sign of osteochondrosis! Not to mention other symptoms that are attributed to the diagnosis of cervical chondrosis.
What causes panic attacks, neck pain, and other symptoms that are so often attributed to cervical osteochondrosis?
Clinical picture
The symptoms of dizziness in osteochondrosis are specific. As a rule, awkwardness and impairment of motor activity are of minor intensity. The feeling of imbalance is stable and gradually increases as osteochondrosis of the cervical spine progresses. As mentioned above, dizziness is often accompanied by other neurological symptoms, such as headache, nausea and vomiting, hyperhidrosis or increased sweating, weakness and increased heart rate.
In some cases, patients may experience attacks of dizziness with cervical osteochondrosis.
Cervical osteochondrosis: symptoms and treatment
It’s rare that anyone today does not encounter manifestations of this widespread disease: according to statistics, about 60% of the population in developed countries suffer from manifestations of osteochondrosis to varying degrees.
The main reasons for such widespread prevalence are sedentary work and the lack of movement of modern people. Previously, cervical osteochondrosis in men usually manifested itself starting from 45-50 years, in women - a little later - 50-55 years. But now there is rapid rejuvenation: the typical picture is noticeable signs of the disease in 30-year-olds, and it is not uncommon for the first symptoms to appear at 20 years of age.
Diagnostics
If dizziness appears, especially if the symptom increases, you should not sit idly by. Only a consultation with a qualified specialist and a full diagnostic study will help to conduct a differential diagnostic search and identify a specific pathology. At the Clinical Institute of the Brain there is an entire department dedicated to the treatment of osteochondrosis of the cervical spine and related complications. An integrated approach to diagnosis allows you to accurately assess the severity of neurological disorders and the localization of the pathological inflammatory process. The following diagnostic methods are used at the Clinical Brain Institute:
- Computed tomographic or magnetic resonance imaging study, which allows a detailed assessment of the localization and degree of the inflammatory process in the intervertebral discs and vertebrae.
- X-ray of the cervical spine;
- Ultrasound Doppler mapping of neck vessels;
- Comprehensive analysis of the patient’s vestibular function.
Types of dizziness
The resulting sensations of difficulty in orientation in space vary in duration, frequency, severity and nature of symptoms. In neurology, the following types of dizziness are distinguished:
- vestibular-stem syndrome is manifested by ringing in the ears, a feeling of rotation, vibration of objects, instability when moving, twitching of the eyeballs, attacks of nausea and (or) vomiting. The cause of the development of the syndrome is insufficient blood supply, impaired transmission of nerve impulses in the cerebellum and vestibular apparatus;
- cochlear-trunk syndrome. Its leading symptoms are whistling, ringing in the ears, a feeling of ear fullness, unilateral or bilateral hearing disorders. Cochlear-trunk syndrome occurs due to a malfunction of the organs responsible for maintaining balance.
Despite the various causes of dizziness, the severity of the accompanying symptoms increases with any sudden, awkward movement of the head or with prolonged stay in one body position.
How to treat?
I feel dizzy with cervical osteochondrosis, what should I do? First of all, you should consult a specialist for advice. Only after the examination can we talk about drawing up an effective treatment plan. Treatment of dizziness with osteochondrosis of the cervical spine consists of complex therapy using both medications and physical procedures. For the purposes of pharmacotherapy, the following groups of drugs are used:
- Non-steroidal anti-inflammatory drugs. They can significantly reduce the amount of inflammation, relieve swelling and, accordingly, compression of the nerve roots and spinal cord. For a more effective effect at the time of therapy, a course of injectable forms of anti-inflammatory drugs is used. The main drugs in this group include: Diclofenac, Ibuprofen, Nurofen and Meloxicam.
- Cerebroprotectors and nootropics are drugs that improve cerebral circulation and metabolic processes in nervous tissue. These drugs include: Piracetam, Cinnarizine, Cavinton or Vinpocetine.
- Chondroprotojectors are means that protect cartilage tissue from destruction. This group of drugs improves the elastic and shock-absorbing properties of the cartilage tissue of the intervertebral disc, thereby relieving compression syndrome.
It is important to note once again that treatment must be comprehensive and complex; only in this case can one hope for a good effect from therapy. For this purpose, in addition to medications, physiotherapy is also used: therapeutic electrophoresis on the neck area, ultrasound and magnetic therapy. The systematic implementation of therapeutic exercises also plays a significant role.
Why is cervical osteochondrosis dangerous?
Many vital vessels, arteries, and capillaries are concentrated in the neck area, so any disturbance there can have unpleasant consequences, including oxygen starvation, hypertension, and vegetative-vascular dystonia.
Cervical osteochondrosis affects the segments of the spine that control the functioning of the shoulder and elbow joints, the thyroid gland, hands and other organs. With osteochondrosis, if left untreated, there is a high probability of pinched nerves and compression of blood vessels, which inevitably affects the functioning of other organs.
Prevention
In order to prevent the development or progression of osteochondrosis of the cervical spine and associated dizziness, as well as other neurological manifestations, the same complex of physiotherapeutic methods is used. To avoid the development of this disease, it is important to understand that only the absence of pathogenic factors can eliminate the unnecessary risk of developing osteochondrosis and its complications. To do this, you need to change your lifestyle and attitude towards your own health. Such simple things as an active lifestyle, proper nutrition, alternating work and rest significantly reduce the risk of osteochondrosis and its manifestations. Take good care of your body and be healthy.
Clinical Brain Institute Rating: 4/5 — 126 votes
Share article on social networks
In what case should you see a doctor?
Since constant dizziness can cause the development of a stroke of ischemic origin, you should consult a doctor at the first signs of osteochondrosis. This is pain of any severity in the back of the neck. It usually intensifies when turning or tilting the head. You should make an appointment with a vertebrologist or neurologist if you experience dizziness more than 2-3 times a month, especially if they are accompanied by visual or auditory disorders.
Treatment methods for dizziness
Cervical osteochondrosis is a degenerative disease that cannot yet be completely cured. Therefore, its therapy uses methods that help achieve sustainable remission. At this stage, there are no significant symptoms, including dizziness.
At the beginning of treatment, patients are advised to wear Shants collars during the daytime for 3-4 hours. When using these devices, there is no compression of the vertebral artery by osteophytes or displaced discs. Doctors also recommend purchasing an orthopedic mattress and pillow for sleeping to prevent circulatory disorders in the brain at night.
Drug therapy
When choosing drugs to eliminate dizziness, the vertebrologist takes into account the cause of its occurrence - muscle spasm, inflammatory edema, hernial protrusion, irritation of nerve endings. The nature of the accompanying symptoms, the age of the patient, and the presence of chronic pathologies of internal organs are also important.
Muscle relaxants
Muscle relaxants are used for muscle spasms to reduce skeletal muscle tone. Treatment regimens include Sirdalud, Tolperisone, Baclosan (Baclofen). For severe pain, the Mydocalm injection solution, which contains the anesthetic Lidocaine, is especially in demand.
Painkillers
Intramuscular administration of Baralgin, Spazgan, and Ketorolac can quickly eliminate pain in the neck. These medications are then prescribed to the patient in tablet form. You can cope with pain with the help of acetylsalicylic acid, Paracetamol, Analgin. Analgesics are not intended for long-term course use. They are recommended to be taken only once to eliminate pain.
Vasodilators of the neutropic or myotropic group
To improve blood circulation in the cervical spine, eliminate oxygen and nutrient deficiency, Xanthinol nicotinate, Pentoxifylline, and Eufillin are used. Therapeutic regimens also include Vinpocetine and Cinnarizine (Stugeron). The drugs have a vasodilating effect, exhibit moderate antihistamine activity, and reduce the excitability of the vestibular apparatus.
Betahistine is used directly to eliminate dizziness. The drug affects blood flow, stimulating microcirculation and permeability of the capillaries of the inner ear.
Anti-inflammatory
Nonsteroidal anti-inflammatory drugs are the first choice drugs in the treatment of cervical osteochondrosis. They eliminate pain and swelling, relieve inflammation, and reduce temperature. Patients with mild discomfort are prescribed ointments and gels Voltaren, Fastum, Artrosilen. Intramuscular administration of Ortofen, Ketorolac, and Movalis helps relieve acute pain. And when they are moderate, tablets Nise, Ketorol, Diclofenac, Celecoxib, Nurofen are used.
Blockades
Drug blockades are indicated for patients with acute, piercing pain that cannot be eliminated with NSAID injections. To carry them out, glucocorticosteroids (Triamcinolone, Diprospan) and anesthetics (Lidocaine, Novocaine) are used. With the help of blockades you can get rid of pain for several weeks.
Vitamins and vitamin complexes
In the treatment of osteochondrosis, clinically manifested by dizziness, drugs with B vitamins are necessarily used. Milgamma, Combilipen, Neuromultivit improve the condition of the nerve pathways and restore innervation. To strengthen the immune system and replenish nutrients in the vertebral structures, balanced complexes of vitamins and microelements are prescribed - Supradin, Complivit, Vitrum, Selmevit.
Physiotherapy and manual procedures
For physiotherapeutic treatment of osteochondrosis complicated by dizziness, 5-10 sessions of magnetic therapy, laser therapy, UHF therapy, shock wave therapy, electrophoresis with anesthetics, analgesics are carried out. Applications with paraffin and ozokerite, hirudotherapy, and acupuncture are used.
It is often possible to avoid surgery by visiting a chiropractor. He presses his hands on the vertebrae, increasing the distance between them.
Physiotherapy
The most effective method of treating osteochondrosis is daily physical therapy exercises. Regular training helps strengthen the muscles of the neck and shoulder girdle and improves blood supply with oxygen to the brain. Exercise therapy doctors recommend that patients tilt and turn the head with resistance, and rotate it in a circular motion. All exercises are performed smoothly, without sudden movements.
Folk recipes
Folk remedies will not help cope with dizziness. But their use at the stage of remission will prevent relapses of osteochondrosis, in which they occur. Ointments, compresses, and applications with ingredients that have a local irritant effect are especially effective. And the use of herbal teas helps improve the quality of sleep and strengthen the body's defenses.
Compresses
A mixture for compresses is prepared from fresh leaves of burdock, cabbage, horseradish, plantain or dandelion. They are ground until a homogeneous mass is formed, a tablespoon of thick honey is added, a drop of essential oils of juniper, rosemary, and eucalyptus are added. Stir thoroughly and apply to the back of the neck. Fix with film, woolen cloth, gauze or elastic bandage. Leave for 2 hours, wash off the residue with warm water, rub any moisturizer into the skin.
Decoctions and infusions of herbs
To prepare a soothing, tonic tea, pour a glass of boiling water into a teaspoon of dry plant materials St. John's wort, chamomile, lemon balm, abalone or thyme. Leave covered for 30-40 minutes, cool, filter. Take the infusion before bed, after adding a little flower honey to it.
A decoction is prepared from a dry mixture of equal parts of calendula, eucalyptus, elecampane and peppermint. Pour 3 tablespoons of plant material into a glass of hot water, bring to a boil and simmer for 20 minutes. Cool and filter. Soak a bandage folded in several layers in the broth and apply it to the back of the neck for an hour.